Overview
Managing Type 2 Diabetes effectively begins with understanding insulin resistance, making necessary lifestyle changes, exploring medication options, and closely monitoring your progress. It's important to recognize that a comprehensive approach can significantly improve your experience. By incorporating dietary modifications, regular exercise, and personalized treatment plans, you can enhance your blood sugar control and overall health outcomes.
You're not alone in this journey. Many individuals find that these changes not only help with managing diabetes but also lead to a more fulfilling life. It's understandable to feel overwhelmed, but taking small, manageable steps can make a big difference. Consider reaching out for support or exploring resources that can guide you through this process.
Remember, we are here to support you every step of the way. Sharing your experiences with others can foster a sense of community and connection. Together, we can navigate the challenges of Type 2 Diabetes and work towards a healthier future.
Introduction
Type 2 Diabetes is more than just a health condition; it represents a complex interplay of biological, lifestyle, and psychological factors that require a multifaceted approach for effective management. As insulin resistance takes hold, it’s understandable to feel overwhelmed. Recognizing the underlying mechanisms and risk factors becomes crucial for those navigating this chronic illness. With a staggering number of individuals affected, early recognition of symptoms can lead to timely interventions that significantly improve health outcomes.
Moreover, the implications extend beyond physical health, impacting mental well-being and raising the potential for serious complications if left unmanaged. You're not alone in this journey. This article delves into essential concepts surrounding Type 2 Diabetes, offering actionable lifestyle changes, exploring treatment options, and emphasizing the importance of monitoring progress. We are here to support you every step of the way as you work toward better health.
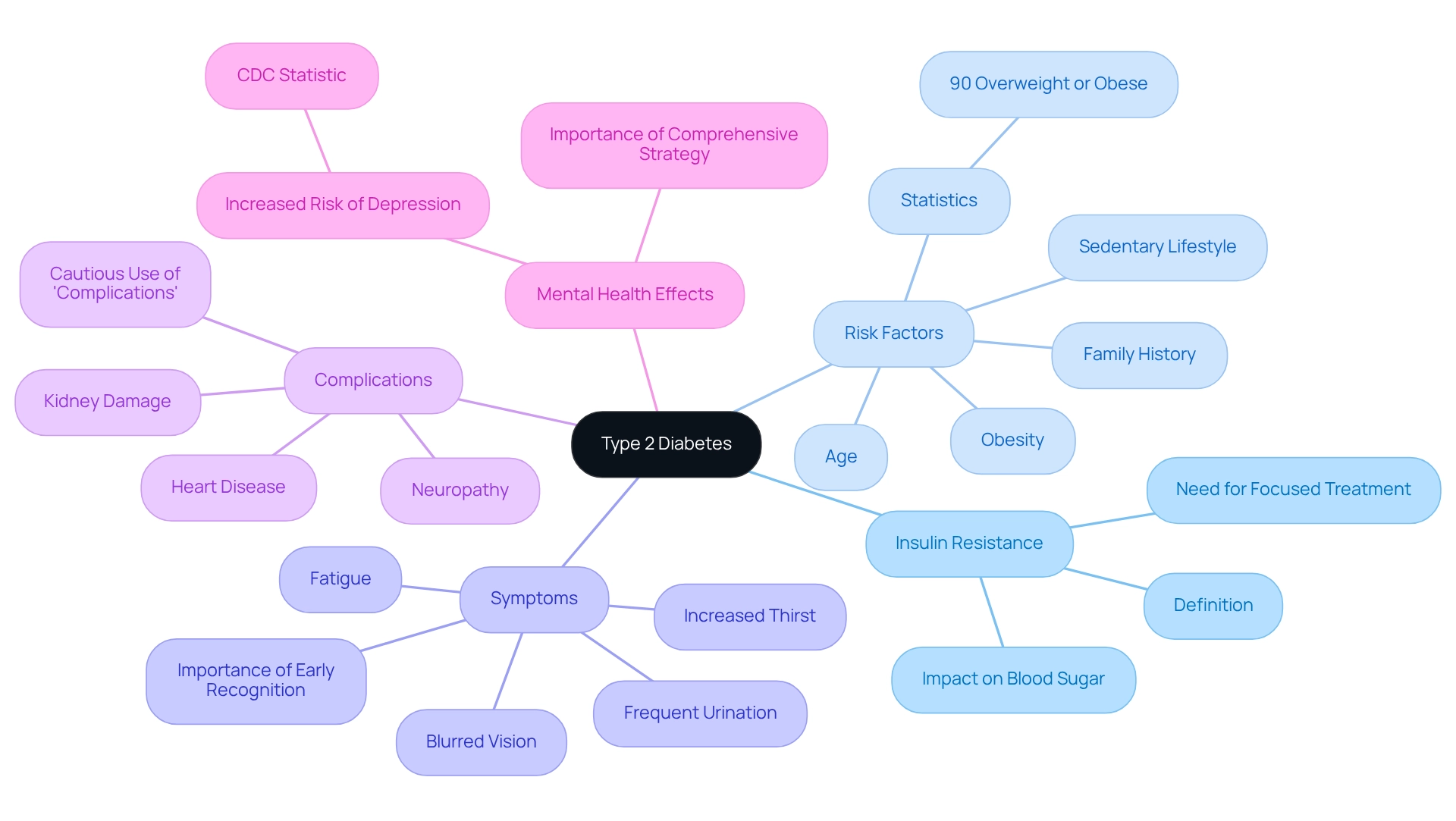
Understand Type 2 Diabetes: Key Concepts and Implications
Diabetes mellitus 2 is a long-lasting condition that can feel overwhelming. It is characterized by insulin resistance, which means the body struggles to use insulin effectively, leading to increased glucose levels. Understanding the following key concepts is essential for effective management, and we are here to support you every step of the way:
- Insulin Resistance: This occurs when the body's cells become less responsive to insulin, complicating blood sugar regulation. Recent studies show that insulin resistance is common among individuals with diabetes of the second type, emphasizing the necessity for focused treatment approaches. It's understandable to feel confused about this process, but recognizing it is the first step toward effective management.
- Risk Factors: Common risk factors include obesity, a sedentary lifestyle, family history, and age. Recognizing these factors is crucial for prevention and management. Statistics indicate that roughly 90% of individuals with Diabetes 2 are overweight or obese, highlighting the significance of lifestyle changes. Remember, small steps can lead to significant improvements in your health.
- Symptoms: Symptoms such as increased thirst, frequent urination, fatigue, and blurred vision can signal the onset of diabetes. Early recognition of these symptoms can facilitate timely intervention and improve health outcomes. If you notice any of these signs, reach out to your healthcare provider for guidance.
- Complications: If unmanaged, Type 2 Diabetes can lead to severe complications, including heart disease, kidney damage, and neuropathy. However, it is important to use the term 'complications' cautiously. Effective handling strategies can mitigate potential health issues. Awareness of these risks emphasizes the necessity of proactive health measures, and you are not alone in this journey.
Furthermore, it is crucial to take into account the mental health effects of managing this condition. According to the Centers for Disease Control and Prevention (CDC), "Individuals with this condition are twice as likely to experience depression as those without it." This highlights the importance of a comprehensive strategy in managing diabetes-related health.
By grasping these essential concepts, you can navigate your diabetes care journey more effectively and engage in proactive health measures that promote a better quality of life. Additionally, insights from case studies, like the one on ectopic lipid deposition in the pancreas, illustrate the physiological aspects of diabetes mellitus and its management, increasing the educational value of this information.
For more resources and assistance in managing Diabetes 2, consider visiting T2DSolutions, where you can find valuable information and community support tailored for newly diagnosed patients. Remember, you are not alone, and there are people and resources ready to help you on this path.
Implement Lifestyle Changes: Diet and Exercise Strategies
Managing Type 2 Diabetes can feel overwhelming, but making some thoughtful lifestyle changes can make a significant difference in your journey.
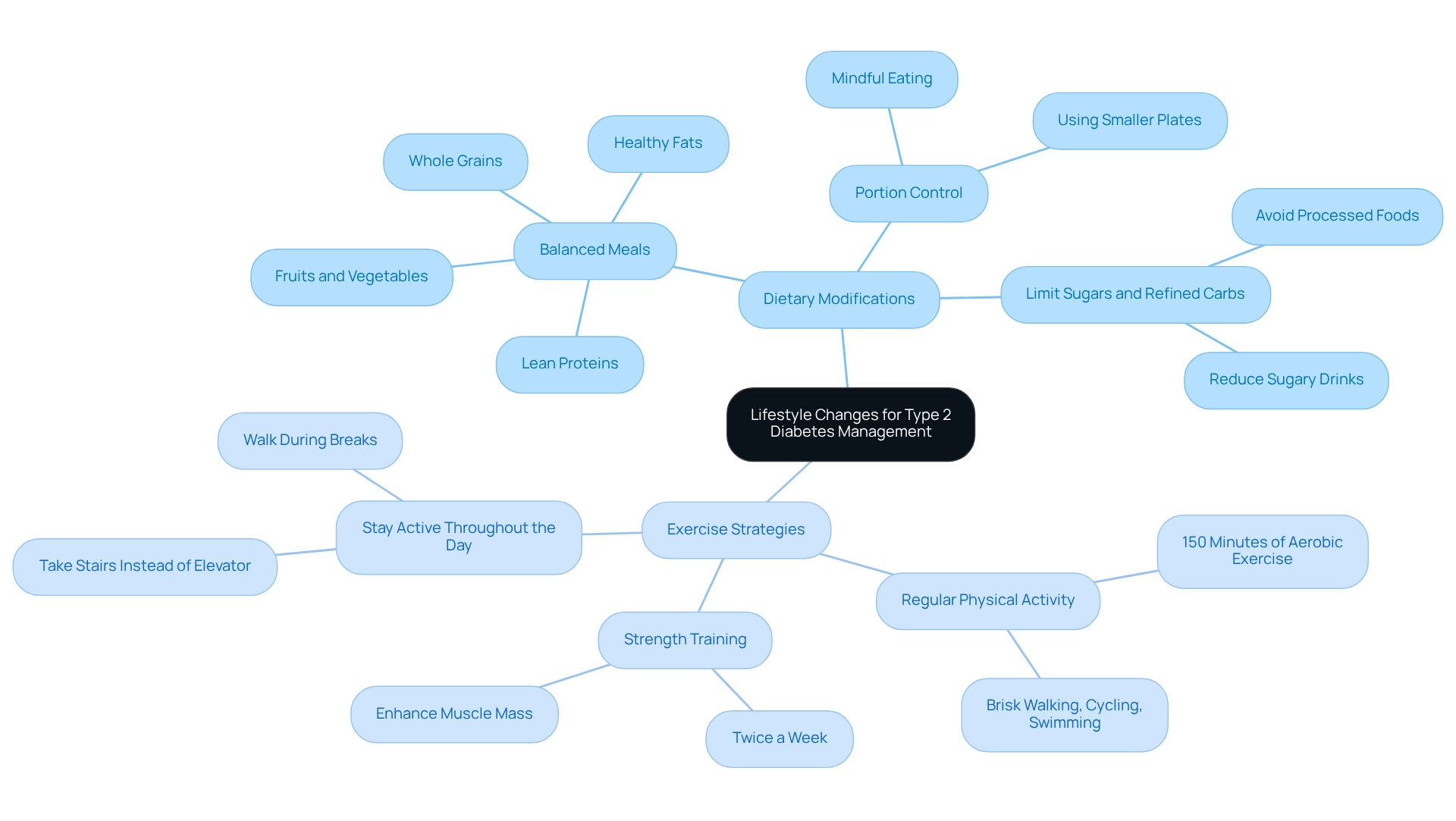
Dietary Modifications:
- Balanced Meals: Focus on a diet rich in whole grains, lean proteins, healthy fats, and a colorful array of fruits and vegetables. A balanced plate not only helps stabilize blood sugar levels but also supports your overall well-being.
- Portion Control: Being mindful of portion sizes is crucial to prevent overeating. Using smaller plates can be a helpful strategy to manage portions effectively, promoting healthier eating habits.
- Limit Sugars and Refined Carbs: Try to reduce the intake of sugary drinks, sweets, and processed foods, as they can cause spikes in blood sugar levels.
Exercise Strategies:
- Regular Physical Activity: Aim for at least 150 minutes of moderate-intensity aerobic exercise each week, such as brisk walking, cycling, or swimming. This level of activity is linked to improved blood glucose control.
- Strength Training: Incorporating strength training exercises at least twice a week can enhance muscle mass and improve insulin sensitivity, which is vital for managing diabetes.
- Stay Active Throughout the Day: Look for small ways to increase your daily movement, like taking the stairs instead of the elevator or walking during breaks. These little changes can add up and greatly impact your health.
By embracing these dietary and exercise strategies, you can significantly improve your management for type 2 diabetes. Research shows that regular physical activity can lower the risk of complications, while the management for type 2 diabetes, including dietary changes, plays a crucial role in maintaining stable blood glucose levels. It's important to note that there were approximately 202,000 emergency room visits for low blood sugar among adults in 2020, highlighting the need for effective management for type 2 diabetes. Additionally, the financial burden of management for type 2 diabetes has increased, with average medical expenses per individual rising from $10,179 in 2012 to $12,022 in 2022. This highlights the importance of these lifestyle adjustments not only for your physical health but also for your mental wellness, as individuals with diabetes are twice as likely to experience depression compared to those without it. Remember, you're not alone in this journey. For more resources and community support regarding diabetes management, consider visiting T2DSolutions, your comprehensive center for diabetes education on levels 2 and 3.
Explore Treatment Options: Medications and Their Roles
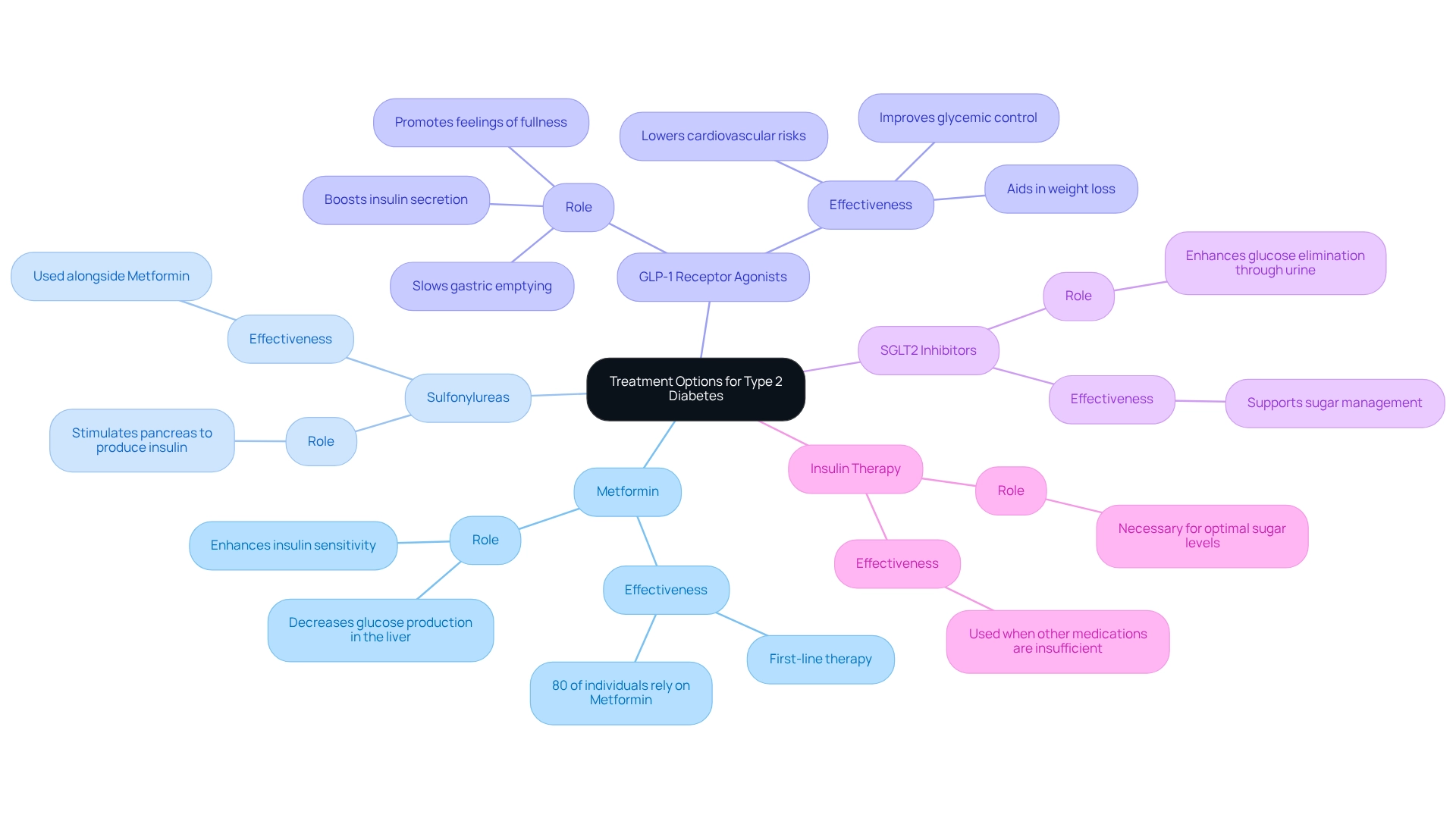
At T2DSolutions, we are committed to providing valuable resources for the management of type 2 diabetes. We understand that the management of type 2 diabetes often requires a combination of medication and lifestyle changes. Here are some common treatment options that may help you on your journey:
-
Metformin: This first-line medication is widely recognized for its ability to lower sugar levels by enhancing insulin sensitivity and decreasing glucose production in the liver. It's comforting to know that around 80% of individuals with Type 2 Diabetes rely on Metformin for effective control, making it a cornerstone in the management of type 2 diabetes. A recent study visualized treatment paths of patients, showing that Metformin is often the initial therapy before other medications are introduced.
-
Sulfonylureas: These medications work by stimulating the pancreas to produce extra insulin, which can help lower sugar levels. They are often used alongside Metformin for enhanced efficacy.
-
GLP-1 Receptor Agonists: This class of injectable medications not only boosts insulin secretion but also slows gastric emptying and promotes feelings of fullness, which can aid in weight loss. Real-world examples show their effectiveness in improving glycemic control, making them a valuable option for many patients. According to endocrinologists, GLP-1 Receptor Agonists have significant advantages in managing weight and lowering cardiovascular risks, which are crucial for effective management of type 2 diabetes in individuals with diabetes mellitus.
-
SGLT2 Inhibitors: These medications enhance the kidneys' ability to eliminate excess glucose through urine, providing an additional method for sugar management that supports the management of type 2 diabetes.
-
Insulin Therapy: In certain situations, insulin therapy may be necessary to achieve optimal sugar levels, especially when other medications are insufficient for the management of type 2 diabetes.
It's vital to work closely with a healthcare provider to determine the most suitable medication regimen tailored to your individual health needs and lifestyle factors, particularly in the context of management of type 2 diabetes. This personalized approach, supported by collaborative efforts in the management of type 2 diabetes, is essential for achieving improved health outcomes. Remember, you're not alone in this journey. For more information and support, explore the resources available at T2DSolutions.
Monitor Progress: Adjusting Management Strategies for Optimal Results
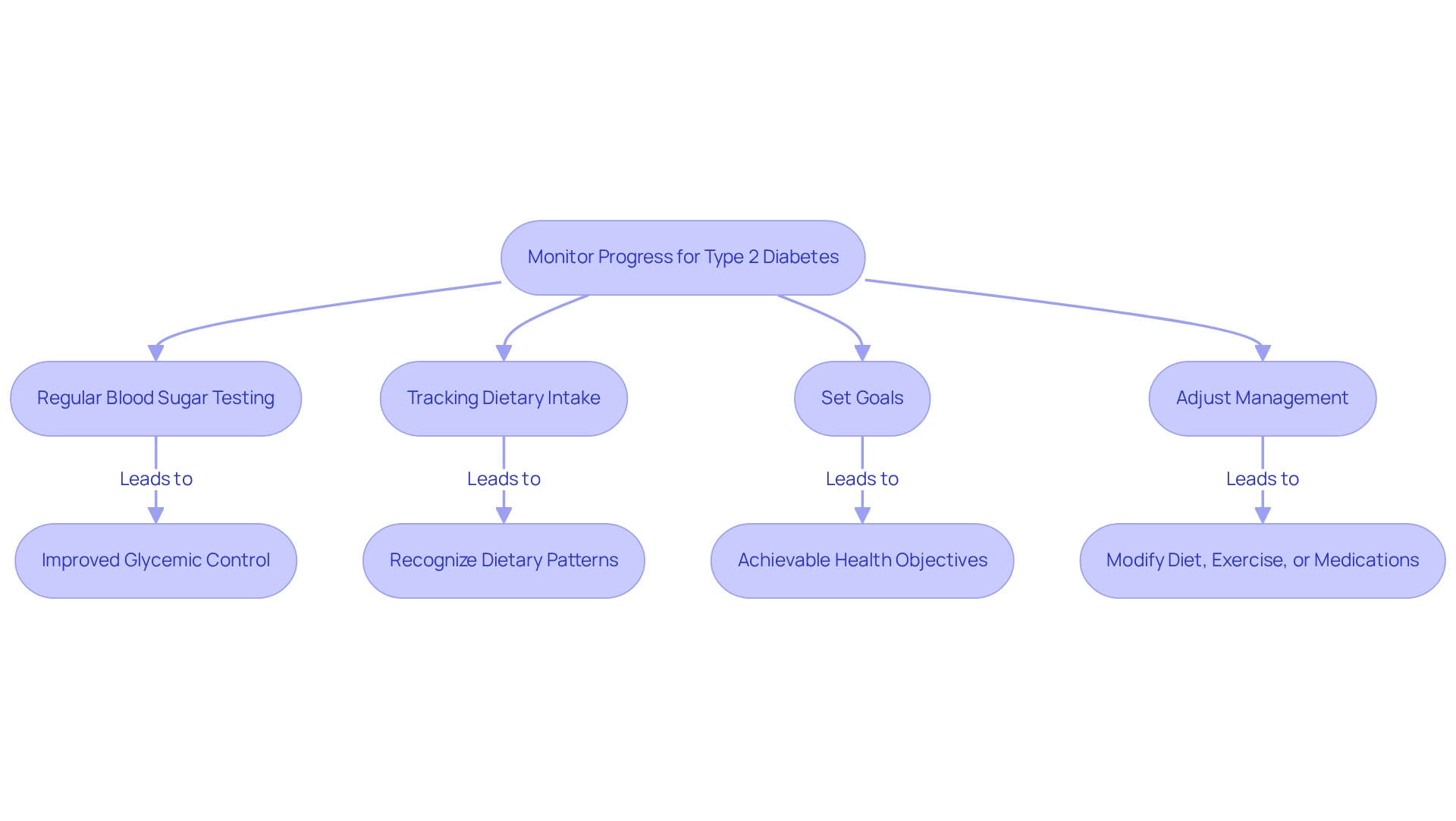
To ensure effective management of Type 2 Diabetes, consider implementing the following monitoring strategies:
-
Regular Blood Sugar Testing: It's important to consistently check your blood glucose levels as advised by your healthcare provider. This practice is crucial for understanding how your diet, exercise, and medications influence your blood sugar. Studies indicate that frequent testing can lead to better glycemic control. Patients who monitor their levels regularly often experience improved outcomes. As Dr. Kelly Wood observes, "Type 2 sugar disease can lead to health conditions that reduce your life expectancy," highlighting the importance of diligent monitoring.
-
Tracking dietary intake through a food diary can significantly impact your management for type 2 diabetes. By documenting what you consume and its effects on your sugar levels, you can recognize patterns and make necessary adjustments. Real-life instances demonstrate that individuals who consistently monitor their dietary intake frequently attain improved management for type 2 diabetes, resulting in better overall health. This aligns with findings from the study titled "Future Directions for CGM Research," which emphasizes the benefits of continuous glucose monitoring (CGM) in diverse patient populations.
-
Set Goals: Collaborate with your healthcare team to establish realistic and achievable objectives for the management for type 2 diabetes, focusing on blood sugar levels, weight control, and physical activity. Setting specific goals can inspire you and offer a clear guide for your health journey. The growing occurrence of Type 2 condition, which experienced a 4.8% increase from 2002 to 2012, underscores the necessity for effective goal-setting in control strategies.
-
Adjust your management for type 2 diabetes by being prepared to modify your diet, exercise routine, or medications based on your monitoring results. Regular follow-ups with your healthcare provider are essential for discussing any necessary changes. Recent advancements in tracking tools for blood sugar control, such as mobile applications and continuous glucose monitors, have simplified the process of monitoring progress and adjusting plans effectively.
By actively participating in these monitoring strategies and making informed adjustments, you can optimize your management for type 2 diabetes and enhance your overall health. Remember, shared knowledge and support can lead to improved health outcomes for everyone involved. You're not alone in this journey. For more resources and support, visit T2DSolutions, your comprehensive hub for Type 2 and Type 3 diabetes education and community support.
Conclusion
Managing Type 2 Diabetes can feel overwhelming, but understanding its key concepts—like insulin resistance, risk factors, symptoms, and potential complications—can empower you. Recognizing these elements is crucial for effective management and early intervention. Lifestyle modifications, such as dietary changes and regular physical activity, are vital for stabilizing blood sugar levels and improving your overall health. By implementing a balanced diet and engaging in consistent exercise, you can significantly reduce the risk of complications and enhance your quality of life.
In addition to lifestyle changes, exploring treatment options, including medications, is essential. Medications like Metformin, GLP-1 receptor agonists, and SGLT2 inhibitors provide critical support in managing blood sugar levels. Collaborating with healthcare providers to tailor a treatment plan ensures that you receive the most effective care suited to your unique needs.
Monitoring your progress through regular blood sugar testing, tracking your dietary intake, and setting achievable goals is fundamental for optimizing diabetes management. By actively engaging in these practices and making informed adjustments, you can enhance your health outcomes. Remember, with the right knowledge and support, managing Type 2 Diabetes can become a more navigable journey. You're not alone in this; we are here to support you every step of the way.
Frequently Asked Questions
What is Diabetes mellitus type 2?
Diabetes mellitus type 2 is a long-lasting condition characterized by insulin resistance, where the body struggles to use insulin effectively, leading to increased glucose levels.
What is insulin resistance?
Insulin resistance occurs when the body's cells become less responsive to insulin, complicating blood sugar regulation. It is common among individuals with diabetes type 2 and requires focused treatment approaches.
What are the common risk factors for developing type 2 diabetes?
Common risk factors include obesity, a sedentary lifestyle, family history, and age. Approximately 90% of individuals with type 2 diabetes are overweight or obese, making lifestyle changes significant for prevention and management.
What are the symptoms of type 2 diabetes?
Symptoms include increased thirst, frequent urination, fatigue, and blurred vision. Early recognition of these symptoms is crucial for timely intervention.
What complications can arise from unmanaged type 2 diabetes?
If unmanaged, type 2 diabetes can lead to severe complications such as heart disease, kidney damage, and neuropathy. Proactive health measures are essential to mitigate these risks.
How does managing type 2 diabetes affect mental health?
Individuals with type 2 diabetes are twice as likely to experience depression compared to those without the condition, highlighting the importance of a comprehensive strategy for managing both physical and mental health.
Where can I find more resources for managing type 2 diabetes?
For additional resources and community support tailored for newly diagnosed patients, consider visiting T2DSolutions, which offers valuable information and assistance.



