Introduction
The A1C test, a pivotal tool in diabetes management, serves as a key indicator of long-term blood glucose control. By measuring the percentage of glycated hemoglobin, this test provides invaluable insights into a patient's average glucose levels over the past two to three months. As diabetes rates continue to rise, understanding the nuances of the A1C test becomes increasingly vital for effective treatment and management strategies.
This article delves into the significance of the A1C test, its comparison with average glucose measurements, the factors that can affect its accuracy, and the limitations that healthcare providers must consider. By exploring these topics, readers will gain a comprehensive understanding of how to leverage A1C testing for optimal diabetes care.
Understanding the A1C Test: A Cornerstone of Diabetes Management
The A1C test, often called glycated hemoglobin, plays an essential role in managing blood sugar levels by assessing the A1C and average glucose concentrations over the past two to three months. This test is expressed as a percentage, representing the proportion of hemoglobin molecules that are attached to sugar. For individuals diagnosed with the condition, the A1C test is essential for evaluating long-term glucose control, including A1C and average glucose levels, and it is recommended that patients undergo this assessment at least twice a year.
A significant decreasing trend in the occurrence of diabetes-related issues was detected after 2008, with an incidence of 8.4 per 1,000 adults, emphasizing the importance of A1C testing in managing the condition effectively. While a general target for A1C and average glucose is set below 7% for most adults, it is important to note that individual goals may differ based on personal health circumstances and conditions. As indicated in recent findings, 'A1C measurement was effective and convenient for screening for blood sugar issues,' emphasizing its role in managing this condition.
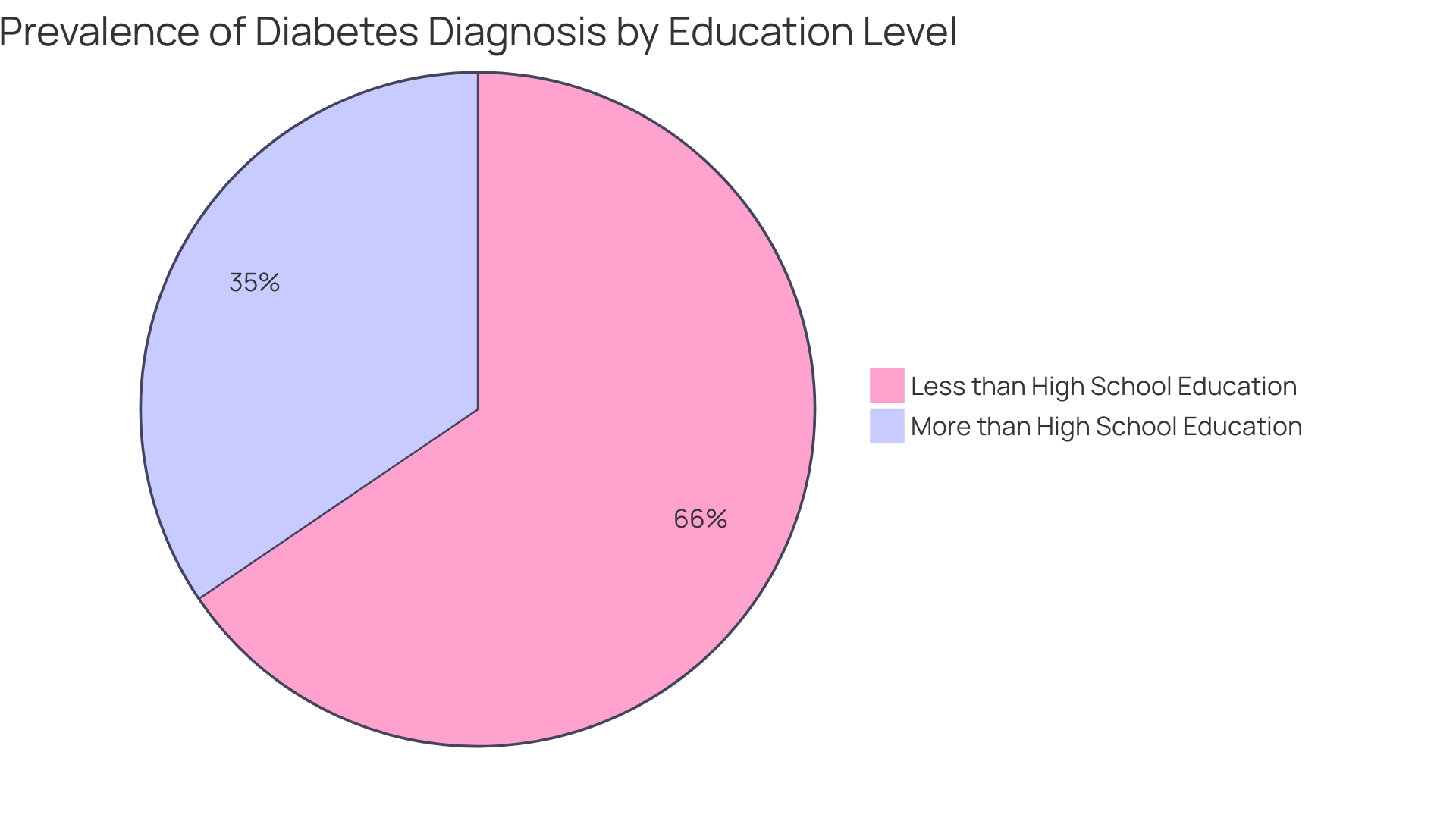
Additionally, case studies have indicated that the prevalence of diagnosed health conditions related to blood sugar varies significantly by education level, with:
- 13.1% of adults with less than a high school education diagnosed
- 6.9% of those with more than a high school education diagnosed
Understanding the A1C test and average glucose levels is fundamental for effective management of the condition, as it offers a comprehensive perspective on blood sugar control over time, rather than merely providing a momentary snapshot. At T2DSolutions, we aim to empower newly diagnosed patients by providing educational resources that explain how to interpret A1C results and set personalized health goals.
Recent studies have underscored the A1C test’s accuracy and its pivotal role in screening for blood sugar disorders, establishing it as a cornerstone of effective healthcare and a key focus of our community support initiatives.
A1C vs. Average Glucose: Key Differences and Their Clinical Implications
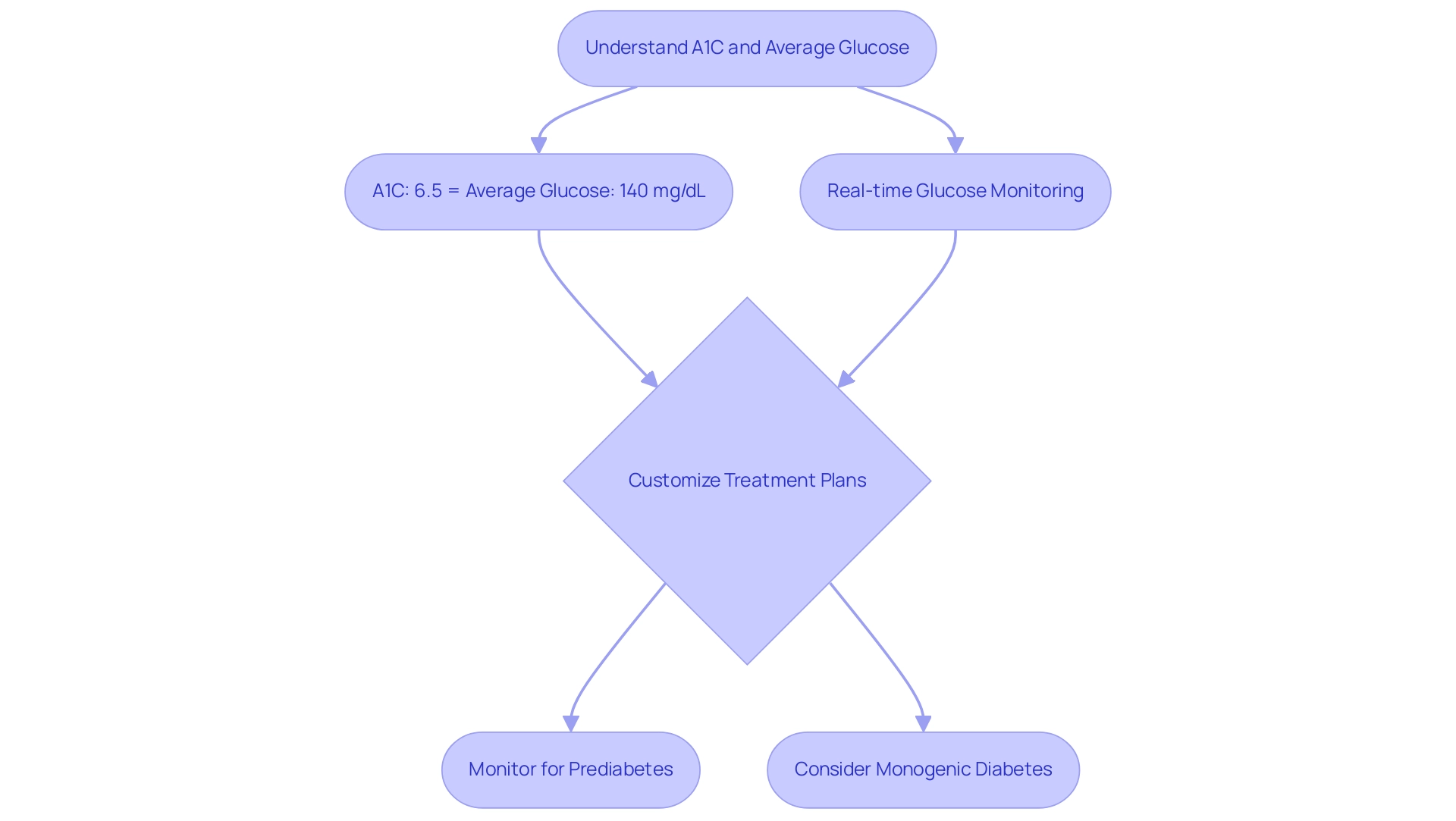
Comprehending the A1C test and average glucose readings is essential for diabetes management, particularly for recently diagnosed individuals seeking assistance from T2D Solutions. The A1C test indicates A1C and average glucose levels, reflecting blood sugar concentrations over the past three months and offering a glimpse of long-term glycemic management. In contrast, the measurement of A1C and average glucose, often obtained from continuous sugar monitoring, captures real-time fluctuations in blood sugar amounts, offering a dynamic view of daily sugar variability.
Clinical studies indicate that an A1C value of 6.5% corresponds with an average glucose concentration of roughly 140 mg/dL, highlighting the importance of A1C and average glucose metrics in patient care. By recognizing these differences, healthcare providers can customize treatment plans and modify medications based on individual sugar patterns. This tailored method is crucial, especially considering the increasing incidence of prediabetes—impacting approximately 97.6 million U.S. adults in 2021—where comprehending both A1C and average glucose readings can significantly affect patient results and management plans.
T2D Solutions serves as a valuable resource for patients to learn more about these metrics and access support. Additionally, varying diagnostic criteria can identify different levels of maternal hyperglycemia and associated risks, sparking ongoing discussions among experts regarding optimal strategies for diagnosing gestational glucose intolerance (GDM). The CoviDIAB registry also provides insights into new-onset COVID-19-related blood sugar conditions, underscoring the necessity of comprehensive glucose monitoring.
Lastly, in cases of diabetes diagnosed in early adulthood, the possibility of monogenic diabetes should be considered, emphasizing the importance of accurate diagnosis for effective diabetes management.
Factors Affecting A1C Accuracy: What You Need to Know
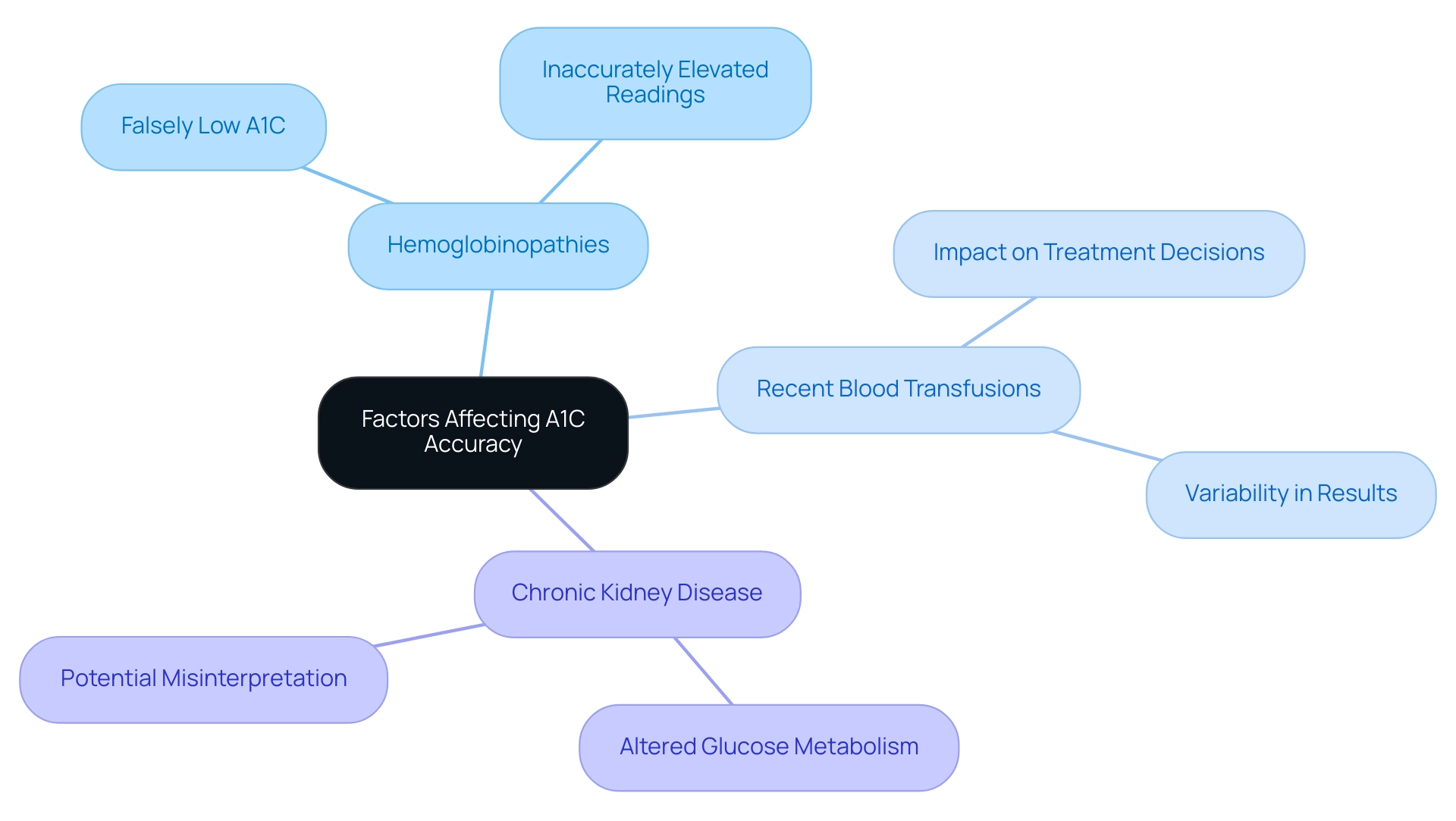
The accuracy of A1C and average glucose test results is influenced by several critical factors, including:
- Hemoglobinopathies
- Recent blood transfusions
- Specific medical conditions such as chronic kidney disease
For example, individuals with anemia often exhibit falsely low A1C and average glucose readings, which can lead to misinterpretation of their glycemic control. Conversely, genetic variants of hemoglobin in certain patients may lead to inaccurately elevated readings of A1C and average glucose.
Based on a CV (coefficient of variation) of 5.7%, A1C levels can vary significantly, which underscores the importance of understanding these factors. It is crucial for healthcare providers to account for these variables when assessing A1C and average glucose results, as discrepancies can substantially impact treatment decisions and overall patient outcomes. A systematic review on the epidemiology of depression and blood sugar levels highlighted these challenges, underscoring the need for healthcare professionals to remain vigilant and informed about factors that may skew A1C measurements.
Additionally, a case study titled 'Exposure and Outcome Variables Definition' established a framework for understanding glycemic control in hospitalized patients with blood sugar issues, emphasizing the importance of accurate measurements of A1C and average glucose and the implications of glycemic gaps. This comprehensive approach ensures optimal management for patients with the condition.
Setting Effective Diabetes Management Goals: The Role of A1C and Average Glucose
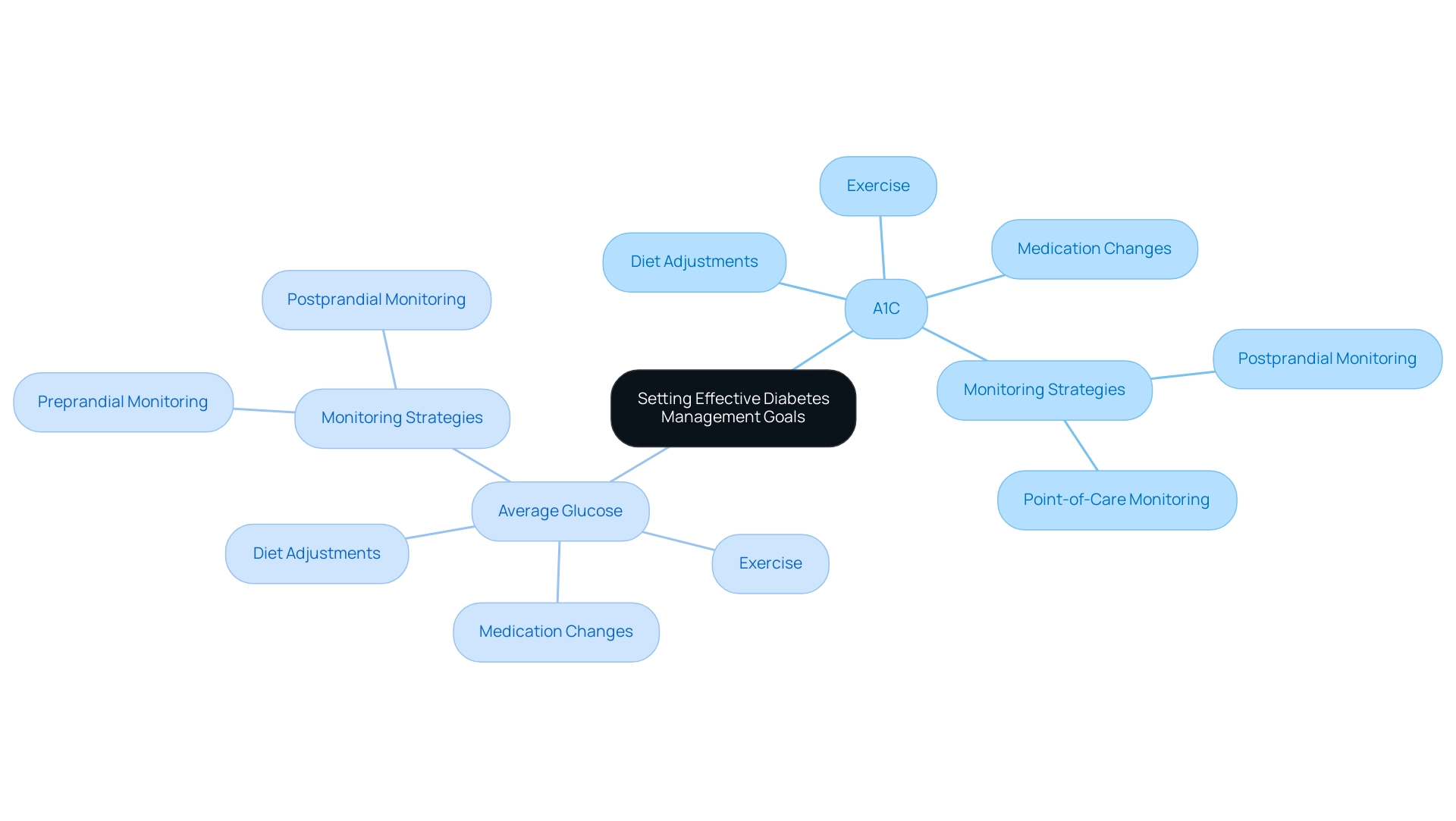
At T2DSolutions, we recognize that setting effective management goals is essential for those newly diagnosed with Type 2 and Type 3 conditions. A1C and average glucose measurements are crucial metrics in this process. A1C and average glucose reflect average blood sugar over two to three months, serving as a long-term target for diabetes management, while A1C levels provide insight into daily fluctuations and inform management strategies.
For instance, if a patient's A1C measurement exceeds the recommended range, it signals a need for adjustments in diet, exercise, or medication to achieve better control. Furthermore, persistently elevated average blood sugar readings may suggest the risk of hypoglycemia, requiring a reassessment of the existing treatment strategy. T2DSolutions aims to empower patients by providing resources and tools to help them understand these metrics and their implications for health.
Recent reports emphasize the significance of addressing postprandial sugar amounts when A1C goals are not achieved, promoting a thorough strategy for monitoring in treatment plans. Furthermore, point-of-care sugar monitoring should be conducted prior to meals in hospitalized individuals with high blood sugar, emphasizing the importance of sugar monitoring in different environments. This multifaceted approach is supported by educators who recommend individualizing management plans based on a combination of A1C and average glucose.
Furthermore, managing blood sugar levels during pregnancy requires careful oversight to mitigate risks to both maternal and fetal health. Expert opinions, such as the assertion that 'the presence of DR is not a contraindication to aspirin therapy for cardioprotection,' reinforce the need for thoughtful adjustments in treatment plans. Ultimately, this comprehensive strategy leads to improved health outcomes, establishing T2D Solutions as a valuable resource in your management journey.
Limitations of the A1C Test: Understanding Its Role in Diabetes Care
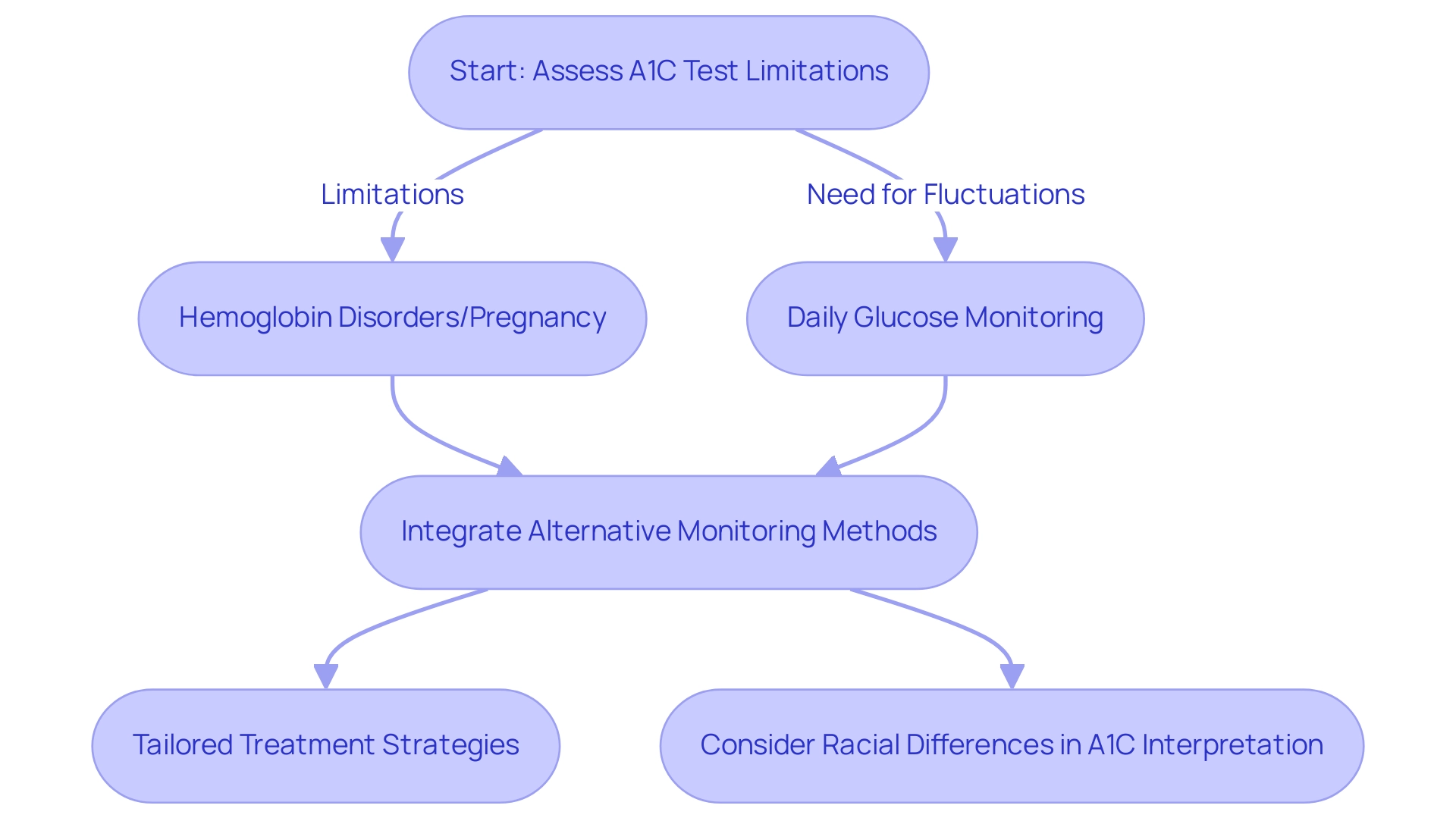
While the A1C and average glucose tests remain cornerstones in managing blood sugar levels, they have notable limitations that warrant consideration. For example, it may not precisely reflect blood sugar amounts for individuals with hemoglobin disorders or during pregnancy. Furthermore, the A1C test fails to capture daily sugar fluctuations, which are crucial for effective diabetes management.
A1C levels correspond to estimated average glucose (eAG) values ranging from 97 mg/dL (5.4 mmol/L) to 298 mg/dL (16.5 mmol/L), highlighting the variability in sugar control that the A1C and average glucose test may not fully reflect. According to the American Diabetes Association Professional Practice Committee, 'alternative monitoring methods, such as continuous glucose monitoring (CGM) and regular self-monitoring of blood glucose, should be utilized alongside A1C and average glucose measurements.' This dual approach enables healthcare providers to achieve a more comprehensive understanding of a patient’s glycemic control, allowing for tailored treatment strategies that better address individual needs.
As part of your journey in managing diabetes, T2DSolutions is here to offer resources and support tailored specifically for newly diagnosed patients. We provide educational materials, community forums, and personalized guidance to ensure you have access to vital information and community assistance. Recent discussions have also highlighted the clinical implications of racial differences in A1C and average glucose values, underscoring the necessity for a nuanced interpretation of A1C results across diverse populations.
Additionally, the addition of SGLT2 inhibitors or GLP-1 receptor agonists is recommended for patients with established cardiovascular disease, chronic kidney disease, and heart failure, regardless of current A1C levels, suggesting a strategic approach to treatment that complements the limitations of A1C testing. By acknowledging these limitations and integrating complementary monitoring techniques, healthcare professionals can enhance diabetes care outcomes.
Conclusion
Understanding the A1C test is fundamental for effective diabetes management, providing insights into long-term blood glucose control that are crucial for tailoring treatment strategies. The test measures the average glucose levels over a two to three-month period, making it an invaluable tool for assessing a patient's glycemic control. However, it is essential to recognize that while the A1C test serves as a cornerstone in diabetes management, it should not be used in isolation. The interplay between A1C levels and average glucose measurements offers a more comprehensive view of a patient's condition, allowing healthcare providers to make informed decisions regarding treatment adjustments.
Moreover, several factors can influence the accuracy of A1C results, including:
- Underlying medical conditions
- Genetic variations
Awareness of these factors is vital for healthcare professionals to interpret results accurately and avoid mismanagement of patient care. In addition, continuous glucose monitoring and regular self-monitoring of blood glucose are recommended to capture daily fluctuations and enhance overall management strategies.
Despite its limitations, the A1C test remains a critical component of diabetes care. By integrating this test with other monitoring methods, healthcare providers can develop personalized treatment plans that address individual patient needs. As the understanding of diabetes evolves, so too must the approaches to managing it, ensuring that patients receive the support and resources necessary for optimal health outcomes. Empowering newly diagnosed individuals with knowledge and tools available through organizations like T2DSolutions can significantly improve their journey toward effective diabetes management.



