Overview
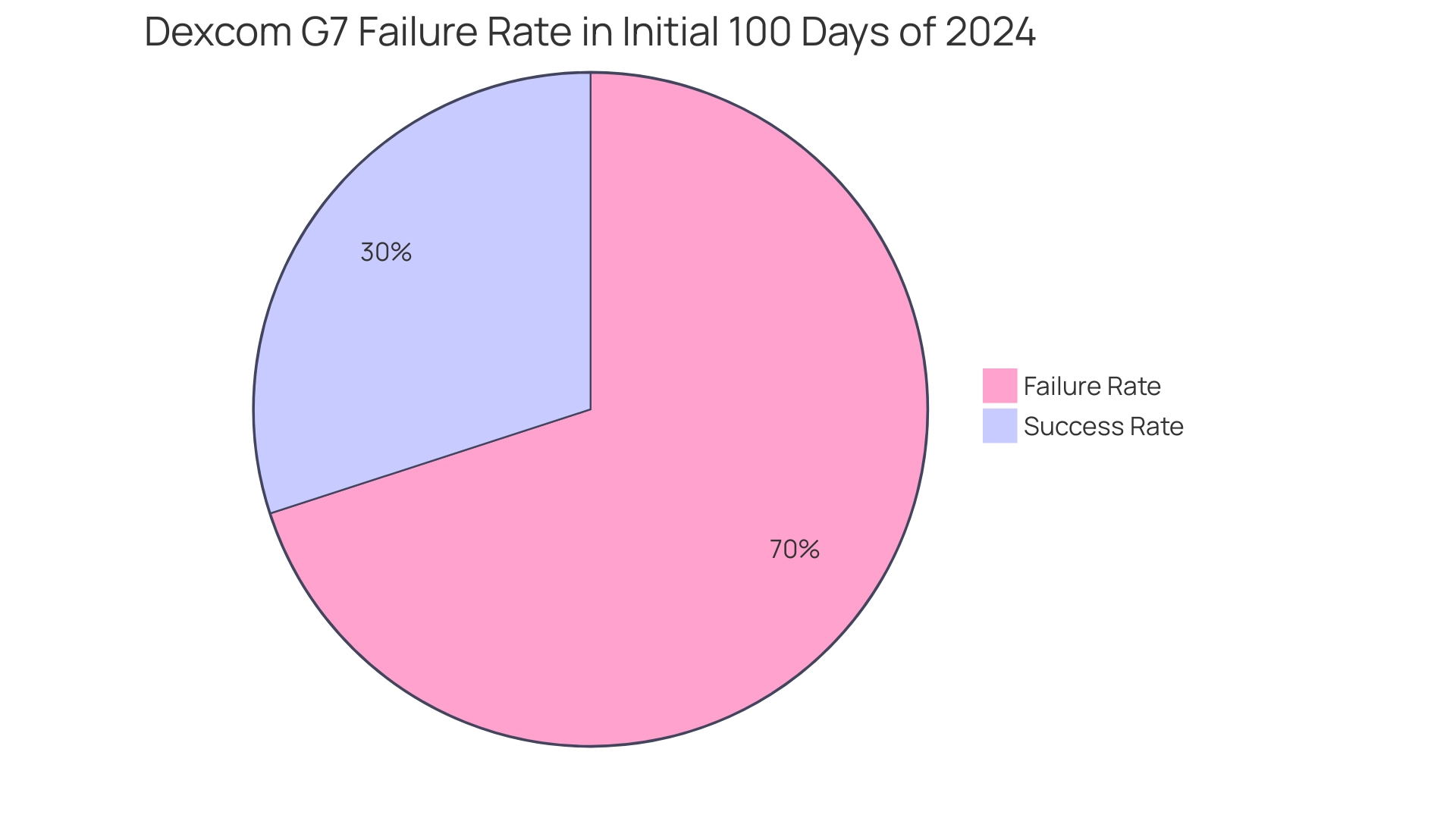
The article highlights a concerning issue: the Dexcom G7 has experienced a significant failure rate, reportedly reaching 70% within the first 100 days of 2024. This alarming statistic raises valid concerns about its reliability for those managing diabetes. It's understandable to feel distressed when faced with such challenges. Many users have reported inconsistent readings, which can lead to emotional turmoil and practical difficulties in managing their health.
For individuals relying on this device for accurate glucose monitoring, the emotional weight of these experiences cannot be overlooked. You're not alone in this journey; many share your concerns and frustrations. This situation underscores the pressing need for community support and effective strategies to navigate these challenges together.
We encourage you to seek out resources and connect with others who understand what you're going through. Sharing your experiences can foster a sense of belonging and provide valuable insights. Remember, we are here to support you every step of the way.
Introduction
In the realm of diabetes management, the Dexcom G7 stands out as a groundbreaking tool, transforming how individuals monitor their glucose levels. This innovative continuous glucose monitoring (CGM) system not only provides real-time insights but also features a user-friendly design that enhances the overall experience for those managing diabetes. As the landscape of diabetes technology evolves, the G7's advanced capabilities hold the potential to improve health outcomes significantly. It can truly be an essential companion for patients navigating the complexities of their condition.
However, it’s understandable to feel concerned about challenges, such as reported failure rates and the emotional impacts on users. By exploring the multifaceted role of the Dexcom G7, this article delves into its accuracy, user experiences, and strategies for optimizing diabetes management. We want to emphasize that you are not alone in this journey. Community support is vital, and we are here to support you every step of the way.
Understanding the Dexcom G7: A Key Tool in Diabetes Management
The G7 represents a significant leap forward in continuous sugar monitoring (CGM) technology, thoughtfully designed to provide real-time sugar readings that empower individuals to manage their diabetes more effectively. This innovative system features a compact, all-in-one sensor that simplifies application and offers a quicker warm-up time than its predecessor, the G6. Such enhancements are vital for patients who need consistent monitoring of their sugar levels, enabling proactive management of blood sugar fluctuations.
For those living with Type 2 and Type 3 Diabetes, the benefits of the Dexcom G7 are profound. By providing immediate access to sugar data, the system supports timely interventions that can lead to improved health outcomes. It's understandable to feel overwhelmed by the complexities of diabetes management, but studies indicate that a stable ambulatory sugar profile requires 15-30 days of CGM data. This underscores the importance of continuous monitoring in understanding glycemic variability and the frequency and severity of hypo- and hyperglycemia.
Moreover, the capabilities of the Dexcom G7 extend beyond mere monitoring; it plays a crucial role in evaluating new therapies and enhancing diabetes management strategies. As healthcare professionals increasingly recognize the value of real-time blood sugar readings, incorporating this system into daily routines can significantly lower the risk of hypoglycemia. As Dr. David Rodbard notes, "The dual-hormone control systems are able to reduce the risk of hypoglycemia by approximately a factor of three relative to the risk when using SAP."
Looking ahead to 2025, the continuous glucose monitoring market continues to evolve, shaped by regulatory approvals and reimbursement policies that enhance accessibility for patients. These factors are essential in transforming the landscape of blood sugar management. The G7 device stands out not only for its technological advancements but also for its potential to revolutionize care for those managing blood sugar through enhanced patient engagement and outcomes.
Real-world experiences illustrate its effectiveness, with many users expressing greater confidence in managing their condition. As specialists in metabolic conditions emphasize, the importance of real-time glucose readings cannot be overstated. The G7 device empowers individuals to take control of their health, fostering a sense of community and support among those facing similar challenges. T2DSolutions is dedicated to ensuring that individuals with blood sugar issues have the tools they need to thrive, offering a wealth of information and resources that enhance the functionality of the G7 device.
By integrating educational support and community engagement, T2D Solutions enriches the overall diabetes management experience for newly diagnosed patients. You're not alone in this journey, and we are here to support you every step of the way.
Evaluating Accuracy and Precision: The Core of Continuous Glucose Monitoring
The precision of the G7 is assessed through the Mean Absolute Relative Difference (MARD), a vital measure that indicates how closely the continuous monitoring device readings align with laboratory results. Recent evaluations show that the G7 achieves a MARD of approximately 8.2%. This positions it among the most precise continuous glucose monitors (CGMs) currently available. This level of accuracy is essential for users, as it directly influences their ability to make informed decisions regarding insulin administration and dietary adjustments.
Additionally, the study reported a Mean Absolute Rate of Change (MARoC) of approximately 1.3 mg/dL/min, further illustrating the performance of the Dexcom G7 in real-time sugar monitoring.
To ensure the reliability of sugar readings, it’s advisable for users to routinely compare CGM data with fingerstick tests, especially during the initial days of sensor application. This practice not only reinforces confidence in the device's performance but also aids in identifying any discrepancies that may arise as the sensor calibrates.
Recognizing the significance of precise glucose measurements is crucial for effective management of your condition. Research studies have consistently highlighted that precise monitoring can significantly impact overall health outcomes, enabling users to maintain better control over their condition. As Manuel Eichenlaub noted, "We, therefore, conclude that minimum CGM performance criteria cannot be established without comprehensive guidelines for study procedures, in particular the collection of comparator data."
This emphasizes the necessity for standardized testing protocols, as shown in the case study titled 'Comparative Analysis of CGM Systems,' which assessed the performance of various CGM systems, including the G7 model.
As the landscape of blood sugar management evolves, the G7 model stands out for its dedication to providing trustworthy information. This empowers users to navigate their health journey with assurance. The study included 318 adult participants, predominantly overweight or obese, which adds relevance to the findings for many users managing diabetes. Remember, you're not alone in this journey; we are here to support you every step of the way.
Examining the Failure Rate of the Dexcom G7: What the Data Shows
Recent analyses reveal that the G7 has faced significant challenges, with reports indicating a Dexcom G7 failure rate reaching as high as 70% within the initial 100 days of 2024. This alarming statistic highlights concerns regarding the reliability of the device, particularly during the critical warm-up period and thereafter. Many users have shared their experiences of inconsistent readings, noting that some sensors do not last the full 10-day duration as promised.
It's understandable to feel frustrated by these challenges. To navigate them effectively, it is crucial for users to meticulously document their experiences with the G7 device. This documentation not only aids in personal monitoring but also serves as a valuable resource when communicating with the company regarding potential replacements for sensors that fail prematurely.
Moreover, individuals may save over $200/month on Dexcom G7 without CGM coverage, providing a financial perspective that is important for many users. As Kevin Hanson, MD, emphasizes, "The significance of precise glucose information for managing the condition and making decisions cannot be overstated."
At T2DSolutions, we are dedicated to serving as a resource hub for individuals managing Type 2 and Type 3 conditions. By promoting a culture of sharing experiences, T2DSolutions encourages individuals to connect with one another, enhancing resilience and assistance within the community. This community-focused approach is further illustrated in the case study titled 'Community Building in Diabetes Management,' which highlights how shared knowledge and support can lead to improved health outcomes.
Additionally, users can silence all alerts for up to 6 hours while still receiving visual notifications on the lock screen. This may help in managing device functionality during challenging times. Remember, you are not alone in this journey. This collective approach not only empowers users but also contributes to improved health outcomes as they advocate for their needs.
Impact of Monitoring Failures on Users: Emotional and Practical Considerations
The dexcom g7 failure rate can lead to profound emotional distress for users, particularly for those who depend on accurate readings for their daily health management. It’s understandable to feel anxiety, frustration, and helplessness when confronted with inconsistent data. Many individuals report these feelings, and studies indicate that a significant percentage of patients with diabetes-related issues experience heightened anxiety and frustration due to the dexcom g7 failure rate, which can exacerbate their overall condition.
In fact, the Type 1 Diabetes Exchange Registry shows that CGM use increased from 7% in 2010-2012 to 30% in 2016-2018. This highlights the growing reliance on such devices. However, the dexcom g7 failure rate can lead to poor glucose control, increasing the risk of serious health complications such as hypoglycemia or hyperglycemia. The psychological impact of the dexcom g7 failure rate is substantial, leading many users to express concerns about their ability to manage their diabetes effectively. Expert opinions emphasize that the emotional effects of device failures can be as important as the physical health risks, underscoring the need for comprehensive assistance.
At T2D Solutions, we recognize the challenges faced by individuals dealing with these issues. Engaging with groups or communities can be invaluable for those navigating these challenges. Sharing experiences with others who face similar struggles fosters a sense of belonging and provides encouragement. These groups often serve as a platform for discussing coping strategies and emotional support, which are essential for managing the psychological burden of this condition.
By interacting with others, users can find comfort and practical guidance, helping to reduce the emotional effects of the dexcom g7 failure rate and improving their overall management journey. Furthermore, it is crucial to recognize that diabetes was the 8th leading cause of death in the U.S. in 2021, accounting for 31.1 deaths per 100,000 of the population. This underscores the seriousness of management and the implications of device failures.
Additionally, a case study titled 'Basal-Bolus Regimen in General Surgery Patients' found that improved glucose control significantly reduced the frequency of composite complications, illustrating the real-world impact of accurate glucose monitoring. Lastly, it is important to remember that mobile health tools do not replace the need for frequent patient contact and feedback in managing blood sugar. This reinforces the significance of comprehensive assistance beyond technology.
To stay updated on resources and support from T2D Solutions, we encourage you to subscribe for updates as we launch our platform dedicated to empowering individuals and families in diabetes management. You're not alone in this journey; we are here to support you every step of the way.
Strategies for Effective Monitoring with the Dexcom G7: Tips for Users
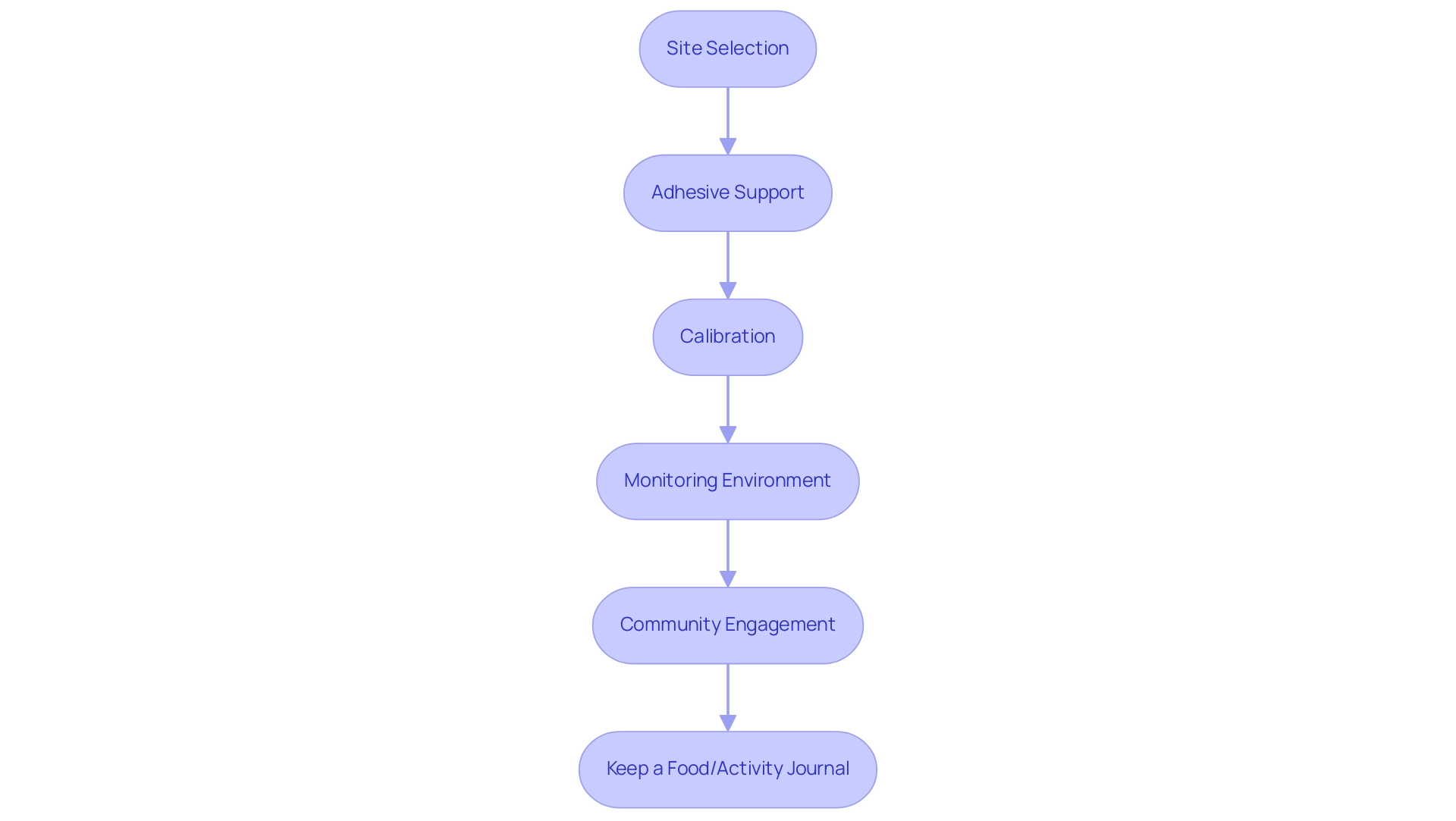
To effectively monitor sugar levels with the Dexcom G7, it’s important to implement a few thoughtful strategies that can make a significant difference in your experience:
- Site Selection: Choose a clean, dry area for sensor placement. Avoid regions that are prone to excessive movement or pressure, as these can impact sensor performance.
- Adhesive Support: Consider using additional adhesive patches to enhance sensor stability. This extra layer helps secure the sensor, reducing the risk of it detaching during your daily activities.
- Calibration: Although the G7 is designed for minimal calibration, it’s essential to conduct occasional fingerstick tests. This practice not only ensures the accuracy of your readings but also builds your confidence in the device's performance.
- Monitoring Environment: Keep the sensor close to the display device to minimize signal loss. A close connection can enhance the reliability of your sugar readings.
- Community Engagement: Actively participate in online forums or local support groups. Sharing your experiences and learning from others can provide valuable insights into effective monitoring techniques and foster a sense of belonging.
- Keep a Food/Activity Journal: It can be helpful to maintain a detailed food and activity journal while using the CGM. This practice aids in linking glucose readings with your dietary and physical activity patterns, enhancing your overall management.
By adopting these best practices, you can optimize your experience with the Dexcom G7, reducing the chances of device failure and leading to more accurate glucose monitoring. It’s encouraging to note that CGM use among insulin-treated beneficiaries increased from less than 1% in 2021 to 30% by the end of 2022, highlighting the growing acceptance of these devices. Moreover, expert insights suggest that pharmacy access has provided significant cost savings for patients, making CGM devices more accessible.
Real-world examples, such as the case study on older adults with Type 1 Diabetes, demonstrate the benefits of CGM in managing the condition effectively. By integrating these strategies and insights, you can feel more empowered in your management journey. Remember, you’re not alone in this journey; we are here to support you every step of the way.
Building a Supportive Community: Sharing Experiences and Insights in Diabetes Management
Creating a supportive community is crucial for individuals managing their condition, especially when facing challenges related to the Dexcom G7 failure rate. It's understandable to feel overwhelmed, but interacting with others through online forums, social media groups, and local assistance networks can be incredibly beneficial. Users can share experiences, exchange tips, and offer emotional support. Research suggests that peer assistance significantly enhances management outcomes for blood sugar conditions. Studies show that individuals who actively engage in networks experience better health results and improved emotional well-being.
In fact, the utilization rate of management care for blood sugar conditions is significantly lower than in other models. In the Netherlands, up to 60% of individuals with this condition obtain regular medical follow-ups. This highlights the need for community assistance to encourage consistent care.
T2DSolutions, a new resource center for education and community assistance, emphasizes the importance of engaging with others who understand the intricacies of managing this condition. By participating in community discussions, sharing personal stories, and seeking advice from peers, individuals can foster resilience and cultivate a sense of belonging. As we look ahead to 2025, the landscape of blood sugar management continues to evolve, with online forums becoming more popular as platforms for sharing insights and encouragement.
These spaces not only facilitate knowledge exchange but also create a supportive environment where individuals can feel understood and empowered. Moreover, advocates for managing blood sugar stress the importance of creating supportive networks. QS, a Professor in health economics, notes, "our findings show the actual utilization of these services was poor among the patients." This highlights the potential role of community assistance in enhancing involvement with health management services. As individuals navigate their health journeys, the connections formed within these communities can provide vital encouragement and motivation, reinforcing the idea that managing this condition is a shared endeavor.
Additionally, case studies on cardiovascular disease and risk management illustrate how community support can play a role in managing health factors related to blood sugar conditions. By leveraging the power of community, individuals can enhance their diabetes management and overall quality of life, especially in light of recent interventions aimed at lowering albuminuria. Remember, you're not alone in this journey; we are here to support you every step of the way.
Conclusion
The Dexcom G7 marks a significant step forward in continuous glucose monitoring, providing users with real-time insights that are essential for effective diabetes management. With its user-friendly design and precise readings, individuals are empowered to take charge of their health, enabling timely interventions that can lead to improved health outcomes. Yet, the journey can be challenging; device failures and their emotional toll can deeply affect users, underscoring the importance of community support and shared experiences.
Despite these challenges, there are strategies to enhance the experience of using the Dexcom G7. By implementing best practices—like choosing the right site, keeping a food and activity journal, and connecting with support networks—users can alleviate some frustrations tied to device issues. The value of community engagement is immense; connecting with others who understand the intricacies of diabetes fosters resilience and provides vital emotional support.
As diabetes management continues to evolve, the Dexcom G7 remains a crucial tool in navigating this complex condition. While obstacles may arise, the promise of better health outcomes through effective technology use and community support is encouraging. By embracing these resources, individuals not only manage their diabetes but also thrive within a nurturing community, reinforcing the comforting truth that they are not alone on this journey.
Frequently Asked Questions
What is the Dexcom G7 and how does it improve sugar monitoring?
The Dexcom G7 is a continuous glucose monitoring (CGM) system that provides real-time sugar readings, allowing individuals to manage their diabetes more effectively. It features a compact, all-in-one sensor that simplifies application and has a quicker warm-up time compared to its predecessor, the G6.
What are the benefits of using the Dexcom G7 for individuals with Type 2 and Type 3 Diabetes?
The Dexcom G7 offers immediate access to sugar data, which supports timely interventions for better health outcomes. Continuous monitoring helps users understand glycemic variability and manage blood sugar fluctuations effectively.
How does the Dexcom G7 contribute to diabetes management strategies?
Beyond monitoring, the Dexcom G7 plays a crucial role in evaluating new therapies and enhancing diabetes management strategies. It helps reduce the risk of hypoglycemia by providing real-time blood sugar readings.
What is the significance of a stable ambulatory sugar profile in diabetes management?
A stable ambulatory sugar profile requires 15-30 days of CGM data, which is important for understanding glycemic variability and the frequency and severity of hypo- and hyperglycemia.
What is the Mean Absolute Relative Difference (MARD) of the Dexcom G7?
The Dexcom G7 has a MARD of approximately 8.2%, indicating it is among the most precise continuous glucose monitors available, which is essential for making informed decisions regarding insulin and dietary adjustments.
How should users ensure the reliability of their sugar readings with the G7?
Users are advised to routinely compare CGM data with fingerstick tests, especially during the initial days of sensor application, to reinforce confidence in the device’s performance and identify any discrepancies.
What impact does precise glucose measurement have on diabetes management?
Precise monitoring can significantly improve overall health outcomes, enabling users to maintain better control over their condition.
What is the Mean Absolute Rate of Change (MARoC) for the Dexcom G7?
The Dexcom G7 has a MARoC of approximately 1.3 mg/dL/min, which illustrates its performance in real-time sugar monitoring.
How does the Dexcom G7 enhance patient engagement and support?
The G7 device, along with resources from T2D Solutions, fosters a sense of community and support for individuals managing blood sugar, enriching the overall diabetes management experience.
What should users keep in mind as they navigate their diabetes management journey with the G7?
Users should recognize that they are not alone in their journey, and support is available to help them manage their condition effectively.



