Overview
The article outlines essential ADA clinical guidelines that every diabetes patient should know, emphasizing their role in effective diabetes management and improved health outcomes. It supports this by detailing updates in screening practices, treatment targets, and the importance of personalized care, which collectively empower patients to engage actively in their health management and adapt strategies based on individual needs.
Introduction
In the realm of diabetes care, the American Diabetes Association (ADA) clinical guidelines stand as a beacon of hope and direction for patients and healthcare professionals alike. These guidelines, rooted in the latest research and expert consensus, provide a structured framework that informs best practices for managing diabetes effectively.
With a focus on personalized treatment plans and the importance of patient education, the ADA empowers individuals to take charge of their health.
As diabetes continues to pose significant challenges, understanding and adhering to these guidelines is crucial for improving health outcomes and fostering proactive self-management strategies.
The latest updates and innovations in diabetes care, along with the emergence of supportive resources like T2DSolutions, highlight the ongoing commitment to enhancing the lives of those affected by diabetes.
Understanding the ADA Clinical Guidelines: A Foundation for Diabetes Care
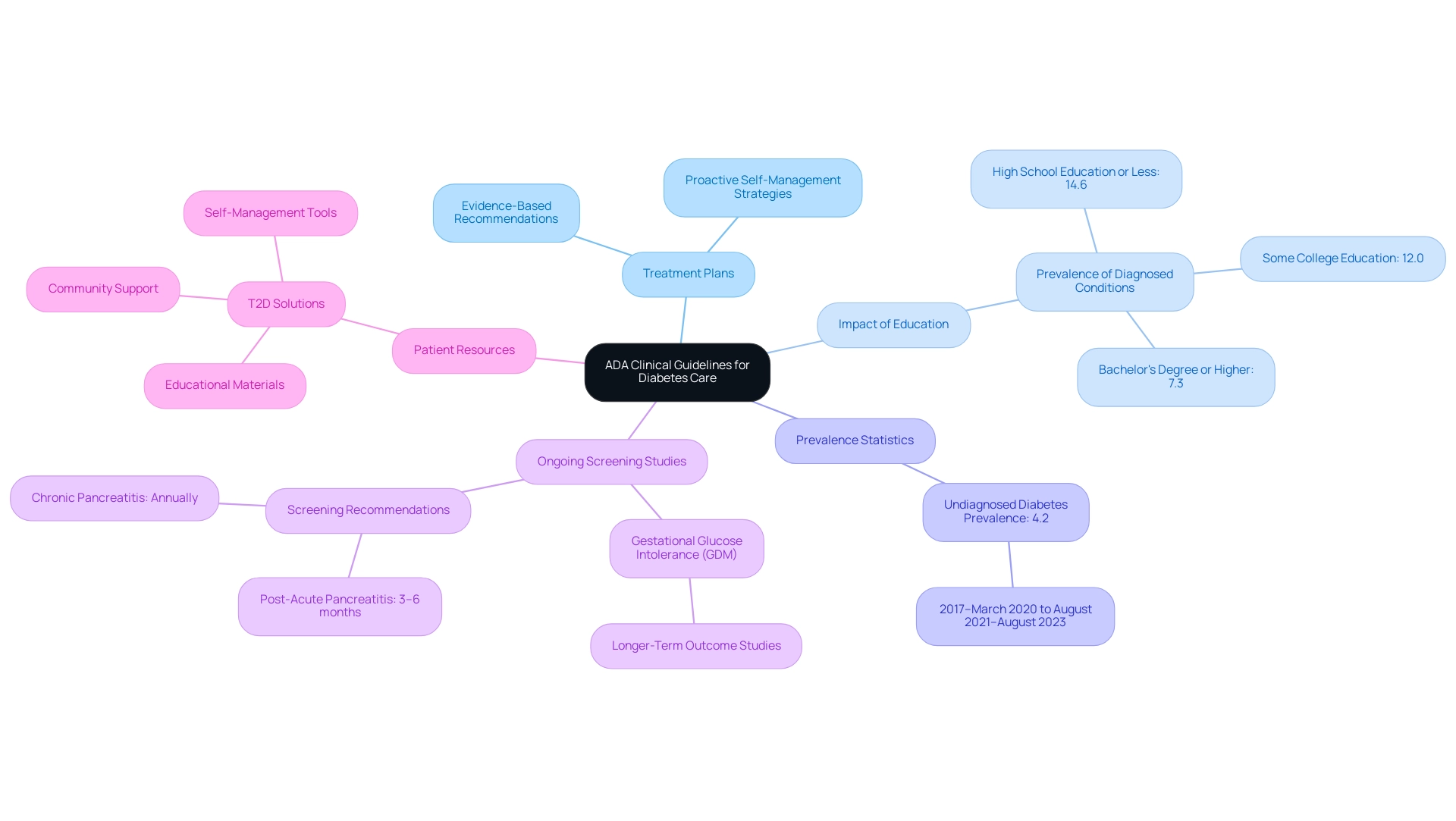
The ADA clinical guidelines are essential for effective diabetes care, providing a structured framework that delineates best practices for treatment and management. These guidelines originate from the latest research and expert agreement, providing healthcare professionals and individuals with evidence-based recommendations aimed at enhancing health outcomes. Understanding the significance of following these guidelines is vital for individuals, as it enables them to make informed choices and participate in proactive self-management strategies.
For example, following treatment plans can greatly enhance health outcomes, as emphasized by recent data showing that the occurrence of diagnosed conditions varies with educational attainment, decreasing from 14.6% among individuals with a high school education or less to 7.3% in those with a bachelor’s degree or higher. This statistic illustrates how informed patients tend to manage their condition more effectively, reinforcing the importance of the ADA clinical guidelines in guiding successful management. Additionally, the age-adjusted prevalence of undiagnosed blood sugar issues remained at 4.2% from 2017–March 2020 to August 2021–August 2023, highlighting the ongoing need for effective screening and intervention strategies.
Furthermore, longer-term outcome studies on gestational glucose intolerance (GDM) screening strategies are currently underway, which will provide valuable insights into comprehensive metabolic care. The methodology of estimating the prevalence of the condition, based on survey responses and clinical measurements, ensures precise representation of the illness in the U.S. civilian population, further supporting the significance of the ADA clinical guidelines in improving outcomes. As part of this effort, T2D Solutions serves as an essential resource hub for newly diagnosed patients, offering educational materials, community support, and tools for effective self-management, ensuring that patients have access to the information and resources they need to navigate their health journey successfully.
Latest Updates in ADA Clinical Practice Guidelines for Diabetes
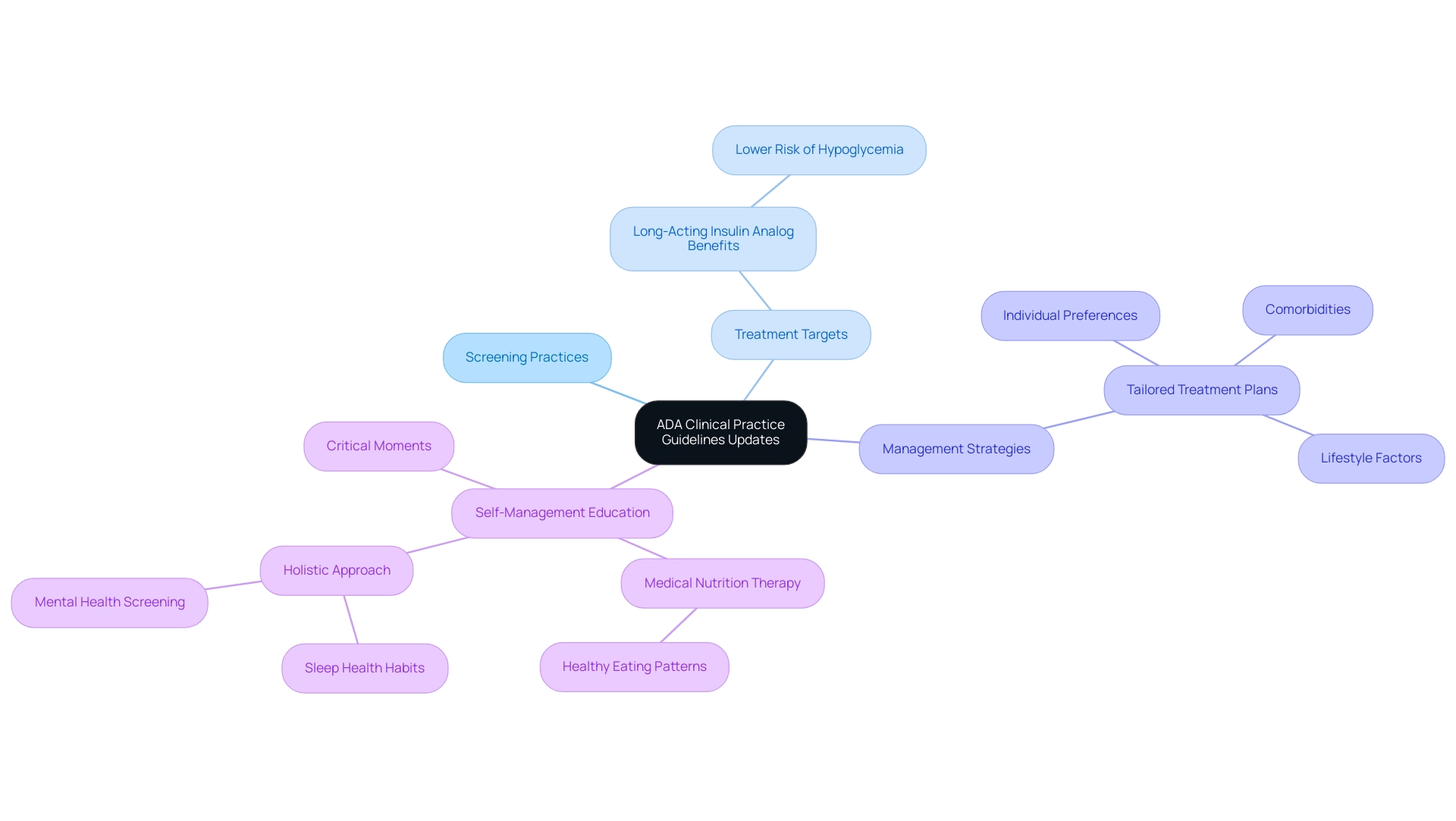
The American Diabetes Association (ADA) consistently updates its ADA clinical guidelines to include the latest findings and advances in blood sugar control. The 2023 updates introduce significant changes in:
- Screening practices
- Treatment targets
- Management strategies tailored for both type 1 and type 2 conditions as outlined in the ADA clinical guidelines.
A significant emphasis is placed on the development of tailored treatment plans that consider individual preferences, comorbidities, and lifestyle factors.
This approach is further supported by new guidance for healthcare professionals, which highlights the need for self-management education at critical moments and underscores the importance of medical nutrition therapy focusing on healthy eating patterns. In particular, long-acting insulin analogs have been found to be associated with a lower risk of hypoglycemia compared to NPH insulin in the Medicare population, providing a safer treatment option for patients. Moreover, the advocacy statement 'Care of Young Children With Diabetes in the Child Care and Community Setting' has been refreshed, reflecting the commitment to comprehensive care as outlined in the ADA clinical guidelines for all age groups.
As Charles “Chuck” Henderson, the ADA’s chief executive officer, states, > Enhancing the lives of individuals impacted by the condition is a key part of the ADA’s mission <, underscoring the relevance of these updates. Additionally, the case study titled 'Facilitating Positive Health Behaviors' illustrates the new guidance for healthcare professionals, emphasizing the importance of evaluating the need for self-management education and promoting a holistic approach to care. Therefore, it is essential for individuals to maintain regular consultations with their healthcare providers to stay informed on how the evolving ADA clinical guidelines may impact their personal health care plans.
Personalizing Diabetes Management: Tailoring ADA Guidelines to Individual Needs
Customizing diabetes care is crucial in adapting the ADA guidelines to meet the distinct requirements of every individual. Key factors such as age, lifestyle, cultural background, and existing health conditions play a crucial role in shaping effective management strategies. For instance, younger individuals may benefit from a more aggressive approach to glycemic control, while older adults might prioritize maintaining their quality of life and minimizing medication side effects.
A study revealed that when recommendations diverged from standard care, individuals experienced an average HbA1c improvement of 0.44% (4.8 mmol/mol), underscoring the potential benefits of personalized interventions. However, it is important to acknowledge the limitations of this study, including the lack of randomization and potential biases in EMR data, which may affect the generalizability of these findings. Cooperation with healthcare professionals allows individuals to develop a tailored care strategy that corresponds with their personal objectives and preferences while adhering to the ADA clinical guidelines.
This tailoring is exemplified by initiatives like the Torbay Care Trust in the UK, which successfully integrated health and social care providers to develop a variety of community-based, person-centered services. Furthermore, telemedicine has emerged as a vital tool in managing diabetes-related conditions, particularly for individuals with limited mobility or those residing in remote areas. By providing blended care that integrates online consultations with in-person interactions, healthcare teams can deliver flexible and customized solutions to meet individual needs.
As an expert from Advanced Technology Corporation noted, 'I have reviewed the report and find it very useful and comprehensive,' emphasizing the importance of thorough strategies in managing the condition effectively. Furthermore, efficient team-oriented IPDM services necessitate defined roles, shared trust, and effective communication among team members and patients, which are crucial for successful collaboration in health care.

The Role of Lifestyle Changes in Effective Diabetes Management
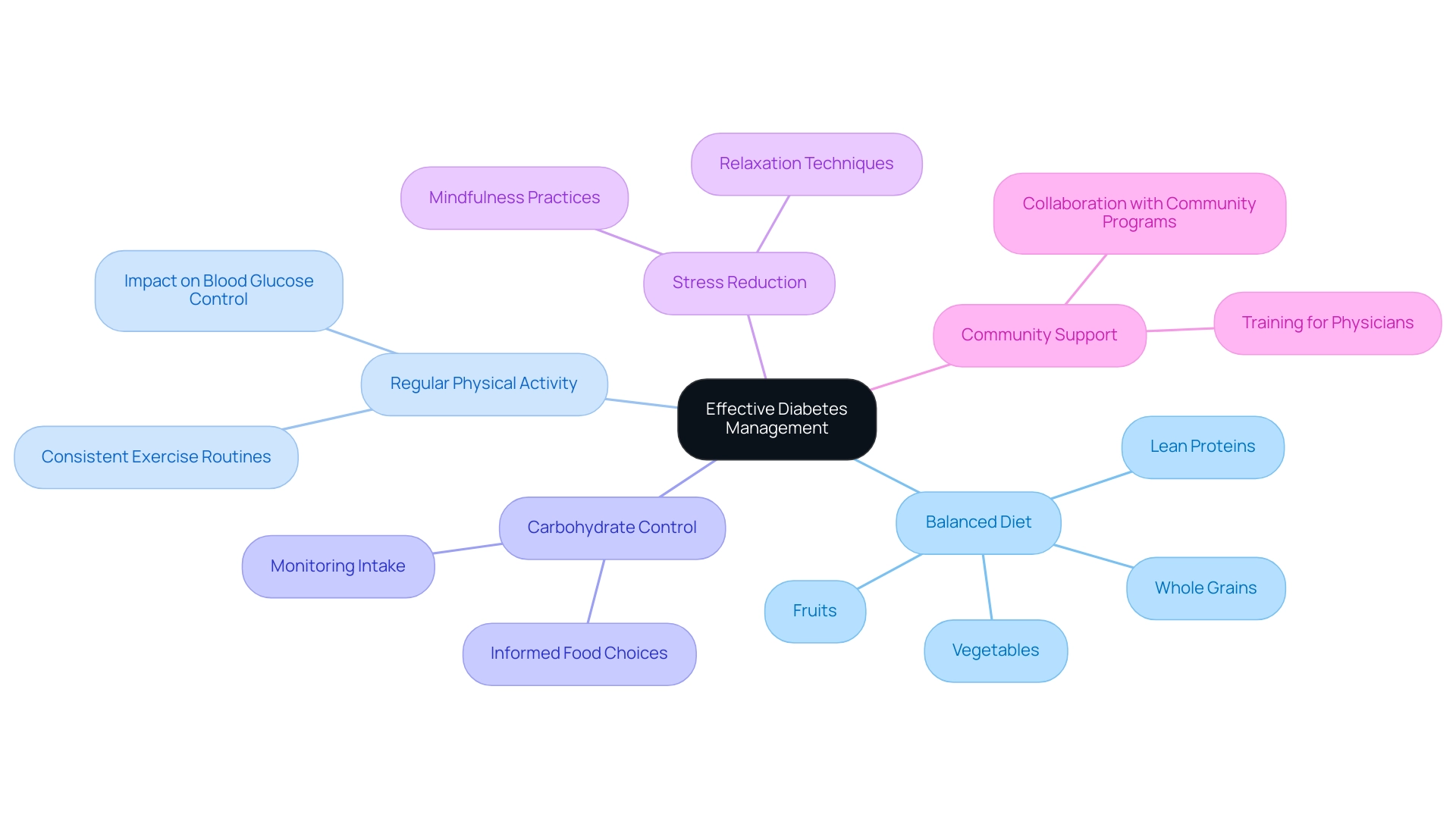
Implementing lifestyle alterations is crucial for effective control of the condition, as highlighted in the ADA clinical guidelines of 2023. Key recommendations include a balanced diet, which should be rich in whole grains, fruits, vegetables, and lean proteins. This dietary approach not only supports overall health but also aids in controlling blood glucose levels.
Regular physical activity is another cornerstone of diabetes care; individuals are encouraged to engage in consistent exercise routines, which have been shown to significantly affect blood glucose control. Research indicates that lifestyle changes can lead to improved results, with various studies demonstrating positive impacts on weight and waist circumference reductions among high-risk populations.
Moreover, effective carbohydrate control is crucial; patients are advised to monitor their carbohydrate intake and make informed food choices to maintain stable blood glucose levels. Stress reduction methods, like mindfulness and relaxation practices, further aid in improving overall well-being and blood sugar regulation. Significantly, the overall direct and indirect projected expenses related to diagnosed health issues in the United States in 2022 reached $413 billion, emphasizing the economic influence of this condition and the necessity of effective oversight strategies.
A pertinent case study named 'Clinical Practice Implementation of Lifestyle Counseling' demonstrates how lifestyle prevention strategies have been adapted for clinical environments, encouraging weight and waist circumference reductions in high-risk patients. Despite challenges in adoption, strategies such as collaboration with community programs and training for physicians have been identified as promising for integrating lifestyle counseling. As Diana Sagastume, a corresponding author at the Institute of Tropical Medicine, aptly notes,
The manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned have been explained and registered.
This demonstrates the dedication to offering thorough insights into the positive impacts of lifestyle changes in health control, emphasizing that these adjustments are not only advantageous but essential for optimal health outcomes. Furthermore, it is crucial to acknowledge that in 2021, this condition was the eighth leading cause of death in the United States, underscoring the urgency and significance of implementing lifestyle changes for its management.
As T2DSolutions launches as a new resource hub, it aims to provide valuable support and education for newly diagnosed patients. By providing resources related to the ADA clinical guidelines, T2D Solutions will empower individuals to make informed lifestyle changes essential for effectively managing their condition.
Managing Comorbidities: A Key Component of ADA Guidelines
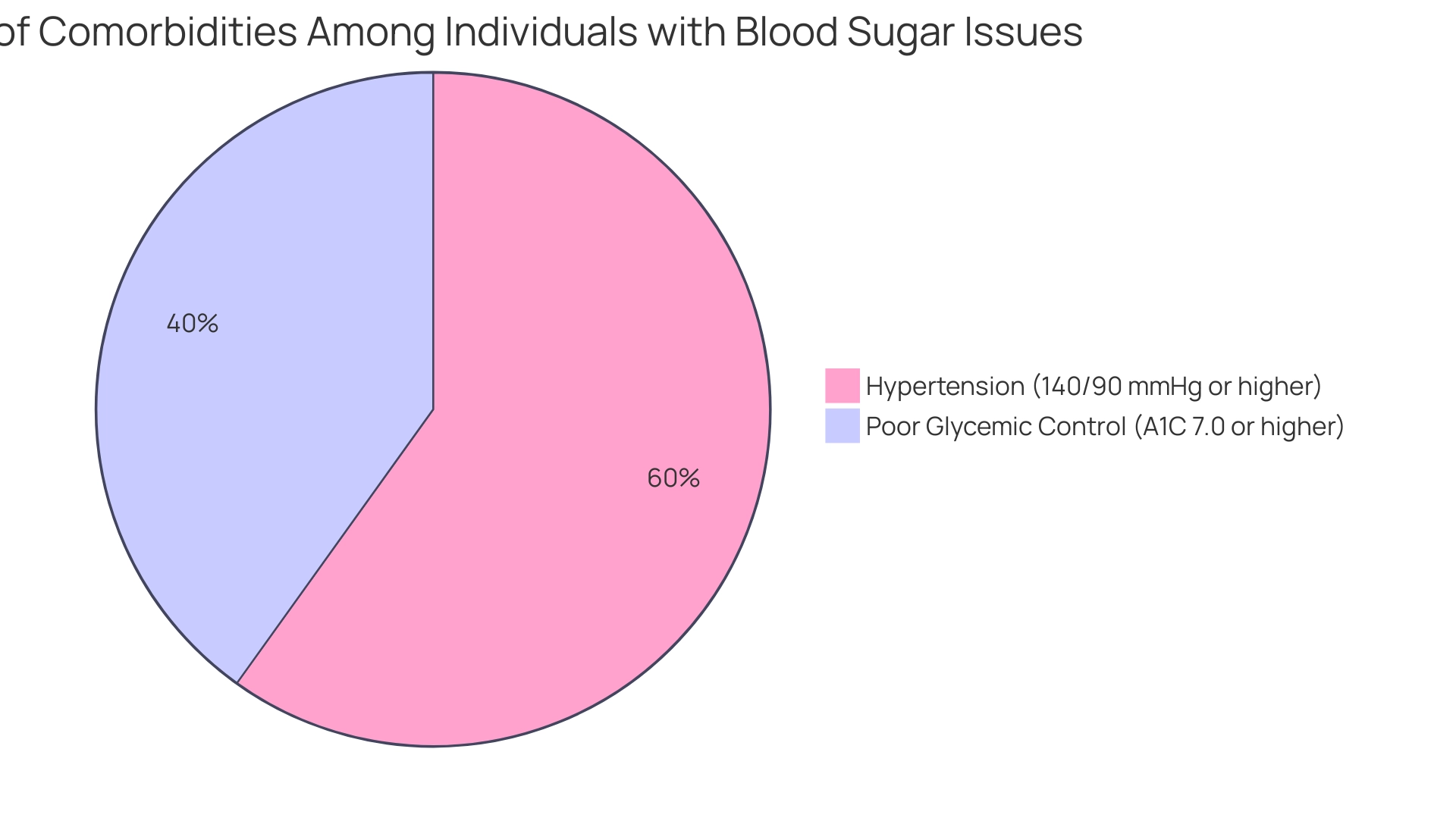
Managing comorbidities is a vital component of the 2023 ADA Standards of Medical Care, particularly given that a significant percentage of individuals with this condition also face additional health challenges. For example, statistics reveal that:
- 70.8% of U.S. adults diagnosed with this condition had a systolic blood pressure of 140 mmHg or higher, or a diastolic blood pressure of 90 mmHg or higher, underscoring the necessity for regular screening for hypertension and dyslipidemia.
The strengths of the study include a substantial number of participants and standardized clinical measurements, which lend credibility to these findings.
The ADA clinical guidelines promote organized monitoring and oversight strategies that focus on both blood sugar regulation and its related comorbidities. Effective blood pressure and cholesterol management can significantly reduce the risk of cardiovascular complications, which are common among individuals with blood sugar issues. Furthermore, a recent case study indicated that among adults with diagnosed conditions related to blood sugar:
- 47.4% had an A1C value of 7.0% or higher, indicating a pressing need for improved management strategies to enhance glycemic control.
This emphasizes the significance of a cooperative healthcare strategy, particularly in tackling the difficulties encountered by older adults with blood sugar issues, who frequently experience variability in clinical presentation and require enhanced social assistance.
T2DSolutions functions as an extensive resource center aimed at assisting newly diagnosed individuals in managing their condition and related health concerns. By offering access to educational resources, expert guidance, and community assistance, T2DSolutions aims to empower individuals in their journey towards improved health.
As healthcare professionals MN and AE emphasize, they have managed and supervised all authors with their experience and vision, reinforcing the importance of expert collaboration in managing the complexities of care.
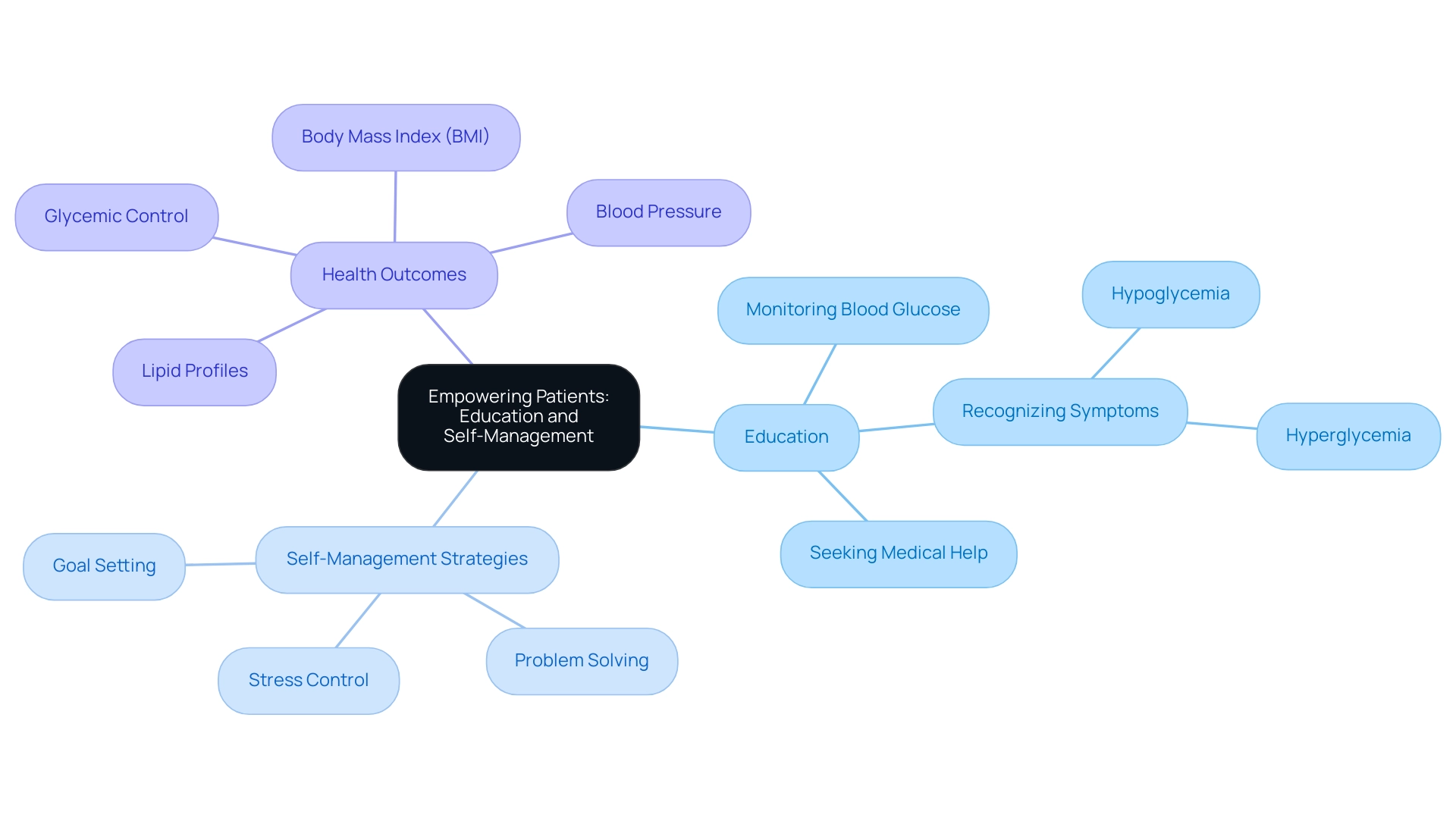
Empowering Patients: Education and Self-Management Strategies in ADA Guidelines
Empowering individuals through education is a cornerstone of the ADA guidelines and a foundational principle at T2DSolutions, your new resource hub for Type 2 and Type 3 health education and community support, launching soon. As we prepare to launch, it is essential for individuals to take an active role in managing their diabetes. A fundamental aspect of this empowerment involves educating individuals about their condition, treatment options, and essential self-management techniques.
This includes:
- Learning how to effectively monitor blood glucose levels
- Recognizing the early signs of hypo- and hyperglycemia
- Understanding when to seek medical assistance
Additionally, self-regulation strategies such as goal setting, problem-solving, and stress control play a crucial role in supporting optimal health and preventing complications. Be sure to subscribe to stay updated on our launch and receive emails when new content is published.
Research highlights the effectiveness of patient education in managing blood sugar levels, with studies showing that two out of five investigations into self-efficacy and foot care revealed significant relationships. This suggests that enhanced self-efficacy can lead to better self-management behaviors. As Weidi Qin, a leading expert in the field, noted, "HCPs could focus efforts on increasing self-efficacy in middle-aged and older adults with this condition, and especially older Mexican Americans, to help them self-manage diet, medication, and glucose testing."
Such insights underline the importance of culturally tailored educational programs that resonate with diverse populations, particularly given the differing effects of self-efficacy by race, which suggests a need for services that cater to specific cultural contexts.
In practice, self-management education (DSME) programs have demonstrated remarkable effectiveness in improving:
- Glycemic control
- Lipid profiles
- Body mass index (BMI)
This is in accordance with ADA clinical guidelines, while also showing modest success in enhancing blood pressure levels. T2DSolutions will offer a variety of features, including personalized education resources, community support forums, and expert-led workshops. However, it is important to acknowledge the limitations of existing studies, primarily their small sample sizes and high risk of bias, which may affect the generalizability of the findings.
Despite these limitations, the call for further research into DSME effectiveness in varied populations remains urgent. This ongoing commitment to education and empowerment at T2Solutions will ultimately lead to improved health outcomes and quality of life for individuals with blood sugar issues.
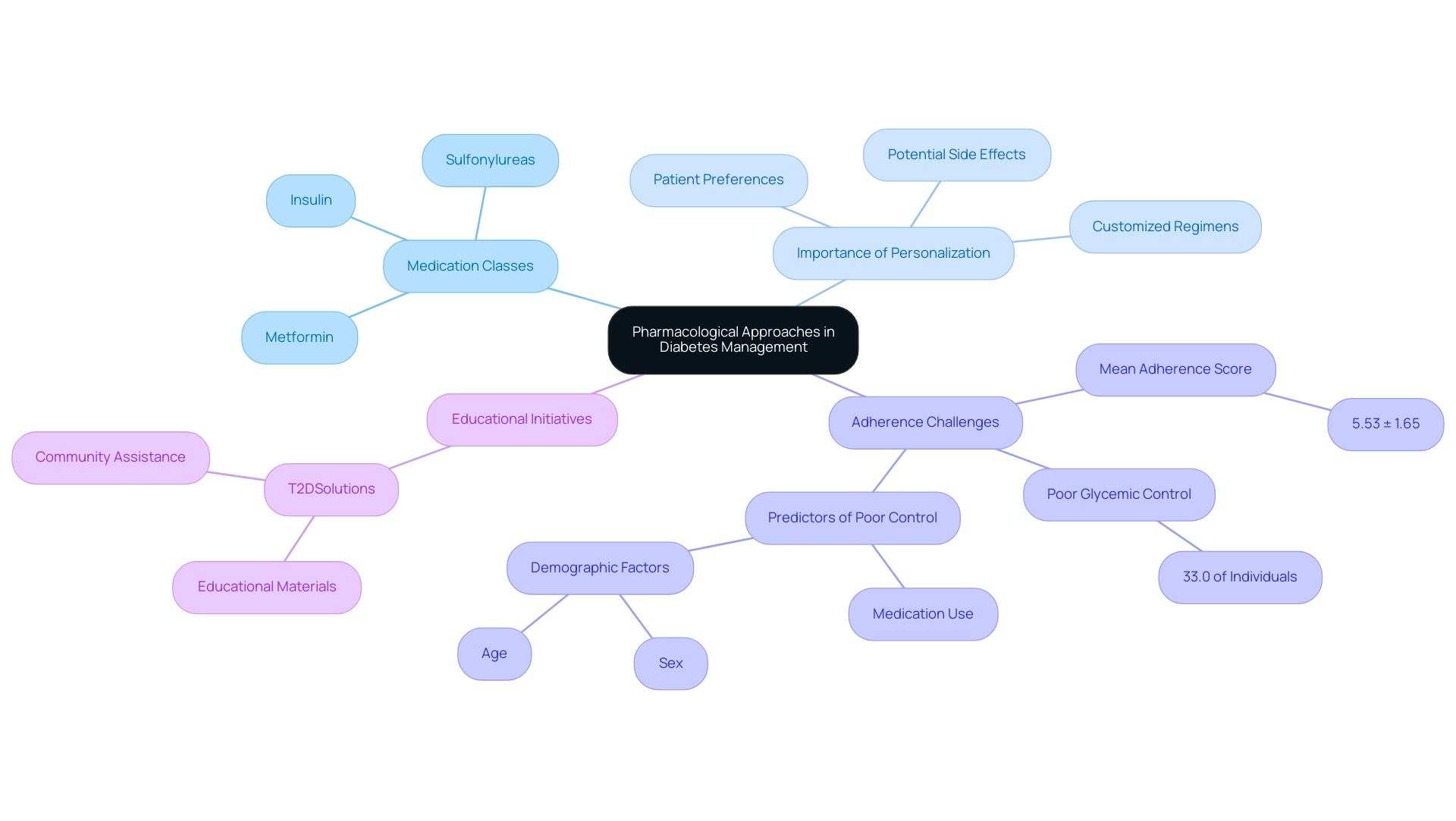
Pharmacological Approaches: Understanding Medication Management in ADA Guidelines
Pharmacological approaches play a crucial role in managing the condition, as highlighted by the ADA guidelines. Medications are often necessary to control blood glucose levels, tackle comorbidities, and mitigate complications associated with the condition. Common classes of diabetes medications include:
- Metformin, which primarily improves insulin sensitivity
- Sulfonylureas that stimulate insulin secretion
- Various forms of insulin that provide direct glucose regulation
The ADA guidelines highlight the significance of healthcare providers working together with individuals to customize medication regimens that suit personal health requirements, preferences, and potential side effects. Comprehending the specific functions of these medications not only enhances adherence but also empowers individuals throughout their treatment journey. Recent data from a study indicated a mean score of 5.53 ± 1.65 for medication adherence among individuals, underscoring the necessity for strategies that promote consistent use.
A case study titled 'Glycemic Control Factors' revealed that 33.0% of individuals exhibited poor glycemic control, with predictors including the use of specific medications for managing blood sugar and demographic factors. As observed by specialists in the domain, compliance with recommended plans is essential for the best results in managing the condition, emphasizing the significance of individual education and continuous assistance in exploring treatment choices. T2DSolutions seeks to enhance these pharmacological methods by offering educational materials and community assistance, enabling individuals to more effectively manage their condition.
Marzieh Khatooni emphasized that all authors read and approved the final version of the manuscript, underscoring the collaborative effort in addressing medication adherence challenges. Moreover, a recent cross-sectional study on medication adherence among individuals with Type II Diabetes Mellitus conducted in Eastern India adds timely context to the discussion, further illustrating the adherence challenges faced by individuals.
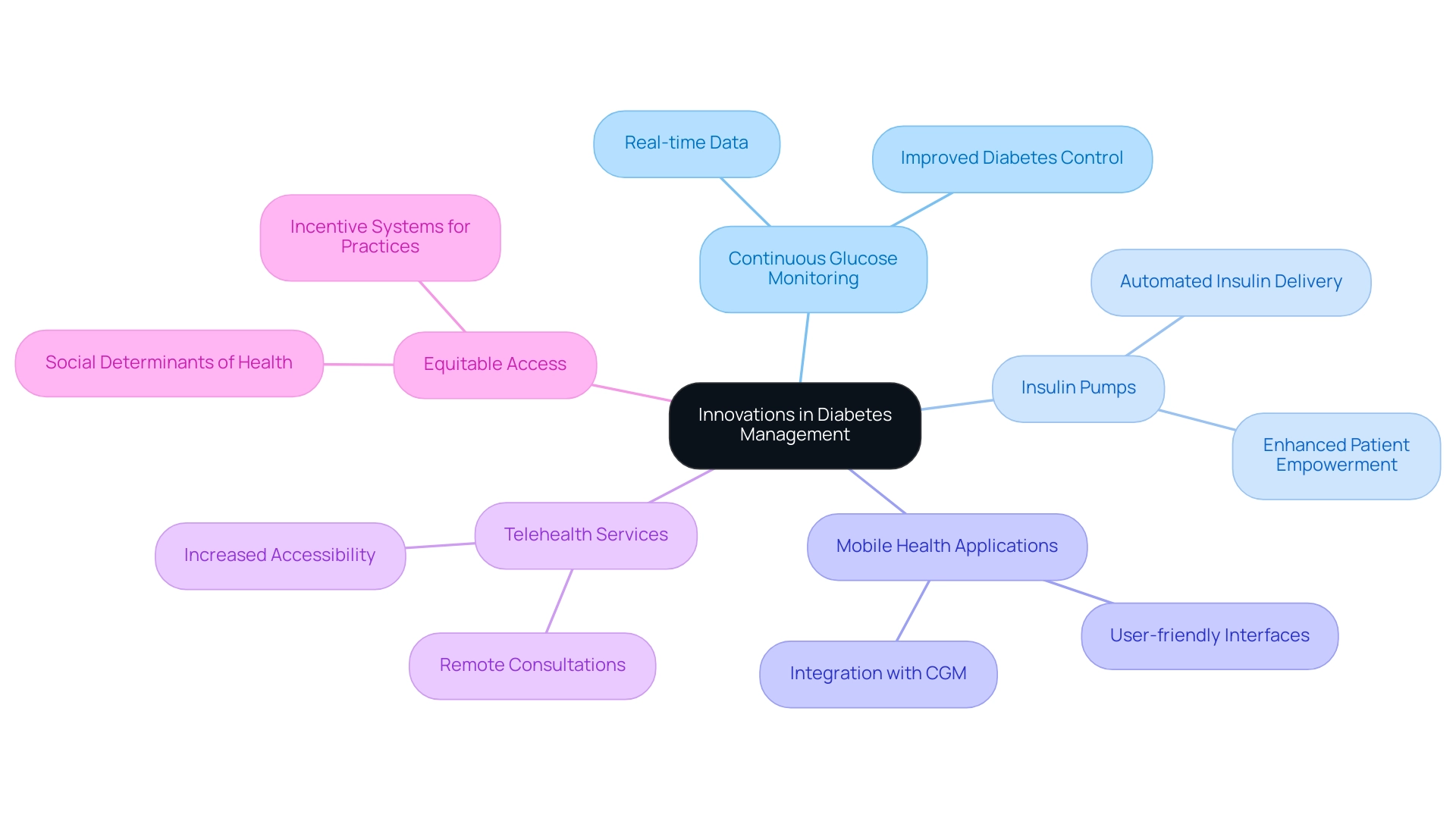
Leveraging Technology: Innovations in Diabetes Management According to ADA Guidelines
The integration of advanced technology in the treatment of blood sugar conditions is strongly advocated by the ADA clinical guidelines, which particularly emphasize the transformative role of continuous glucose monitoring (CGM) systems. At T2DSolutions, we are thrilled to assist newly diagnosed individuals by offering them a comprehensive resource center focused on Type 2 and Type 3 health education and community support. Our platform features interactive tools, educational resources, and access to expert consultations to empower individuals in their health management journey.
Studies have shown that individuals with Type 1 diabetes, ranging from one year old to 65, have experienced significant benefits from these technologies, highlighting their effectiveness in improving diabetes control. Innovations such as insulin pumps and mobile health applications empower individuals by providing real-time insights into their blood glucose levels. This immediate access to data enables individuals to make informed decisions regarding their diet, exercise, and medication management.
Moreover, telehealth services have emerged as an essential resource, enabling patients to connect with healthcare providers from the comfort of their homes for consultations and assistance. However, current health policies and practices do not sufficiently assist equitable access to these blood sugar management technologies, particularly for underserved populations. At T2DSolutions, addressing social determinants of health is crucial for alleviating barriers faced by these groups in adopting new care paradigms.
Incentive systems for practices that support underserved populations, along with comparable billing for social determinants of health screening, are essential for promoting equitable access to technologies for controlling blood sugar. As healthcare technology advances, utilizing these tools not only encourages individual empowerment but also opens doors for enhanced care outcomes. Recent studies indicate that integrating technology into blood sugar control aligns with user expectations and is significant in contemporary healthcare practices as outlined by ADA clinical guidelines.
We encourage newly diagnosed patients to subscribe to T2D Solutions for the latest updates, resources, and community support as they navigate their health journey.
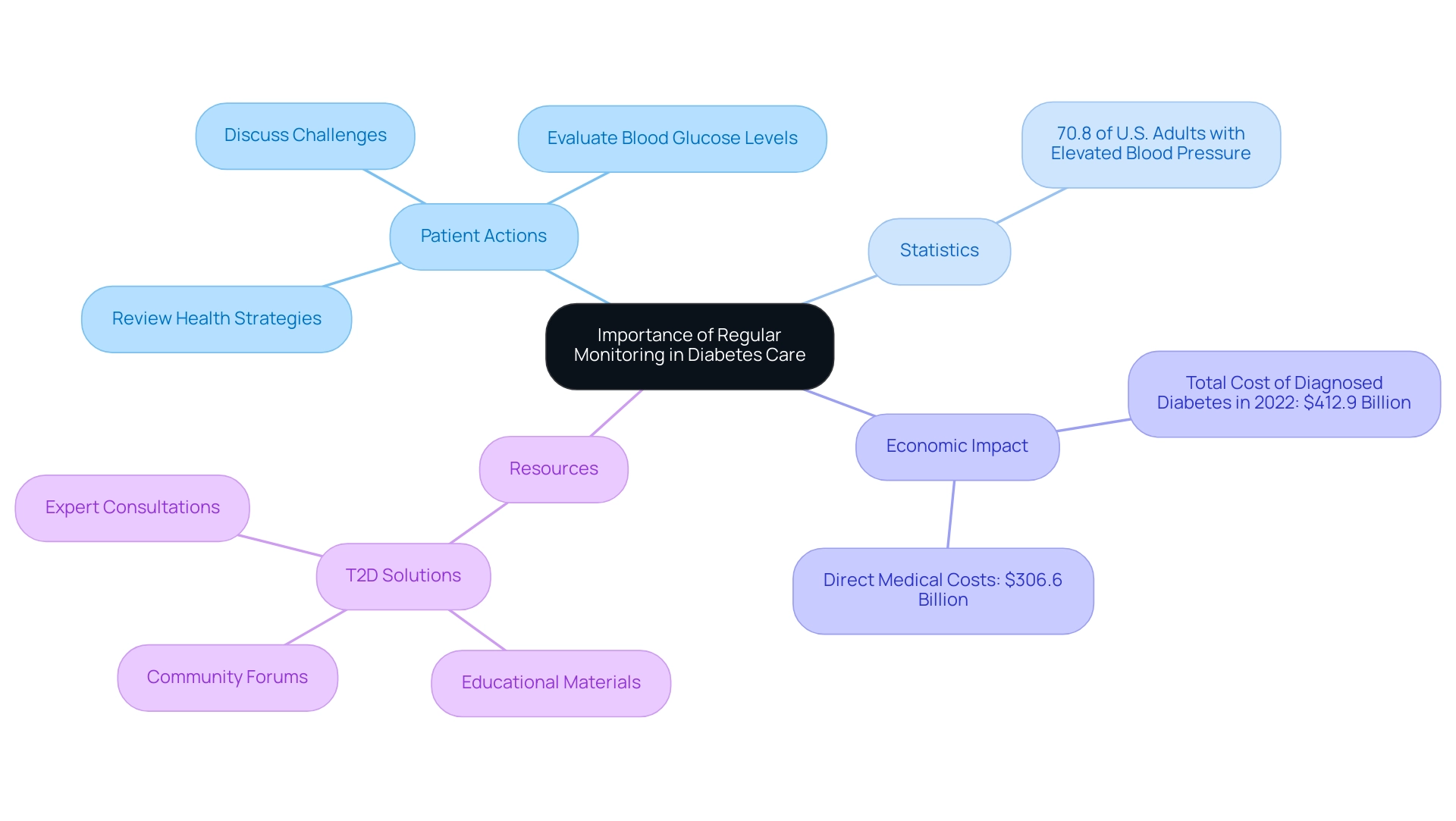
The Importance of Regular Monitoring and Follow-Ups in Diabetes Care
Regular monitoring and follow-ups are critical elements of effective care for blood sugar management, as emphasized by the ADA clinical guidelines. Patients are encouraged to keep regular appointments with their healthcare providers to:
- Review their health strategies
- Evaluate blood glucose levels
- Discuss any challenges they face
These consultations serve as a crucial platform for modifying treatment plans and addressing emerging health issues.
Notably, recent statistics reveal that 70.8% of U.S. adults diagnosed with a blood sugar condition had elevated blood pressure, highlighting the importance of routine checks. Furthermore, consistent monitoring of HbA1c levels, blood pressure, and cholesterol not only aids in the timely identification of potential complications but also facilitates early interventions. The economic effects of handling diabetes are substantial, with the total projected expense of diagnosed conditions in the U.S. in 2022 hitting $412.9 billion, highlighting the significance of regular monitoring in possibly lowering these expenses.
Additionally, conditions like impaired glucose tolerance (IGT) and impaired fasting glycaemia (IFG) serve as critical risk factors for developing type 2, making regular follow-ups essential. With the introduction of T2D Solutions, a new resource center aimed at offering education and community assistance for type 2 and type 3 conditions, individuals now have access to extensive resources such as:
- Educational materials
- Community forums
- Expert consultations
to improve their management and overall health results. T2DSolutions will also offer tools and assistance for regular monitoring, aiding individuals in tracking their progress and remaining connected with healthcare professionals.
Global efforts, including the World Health Organization's response to this health issue through ADA clinical guidelines and initiatives, further emphasize the need for effective monitoring and follow-up strategies. By prioritizing regular follow-ups, along with the assistance from T2DSolutions, newly diagnosed individuals can significantly enhance their condition oversight.
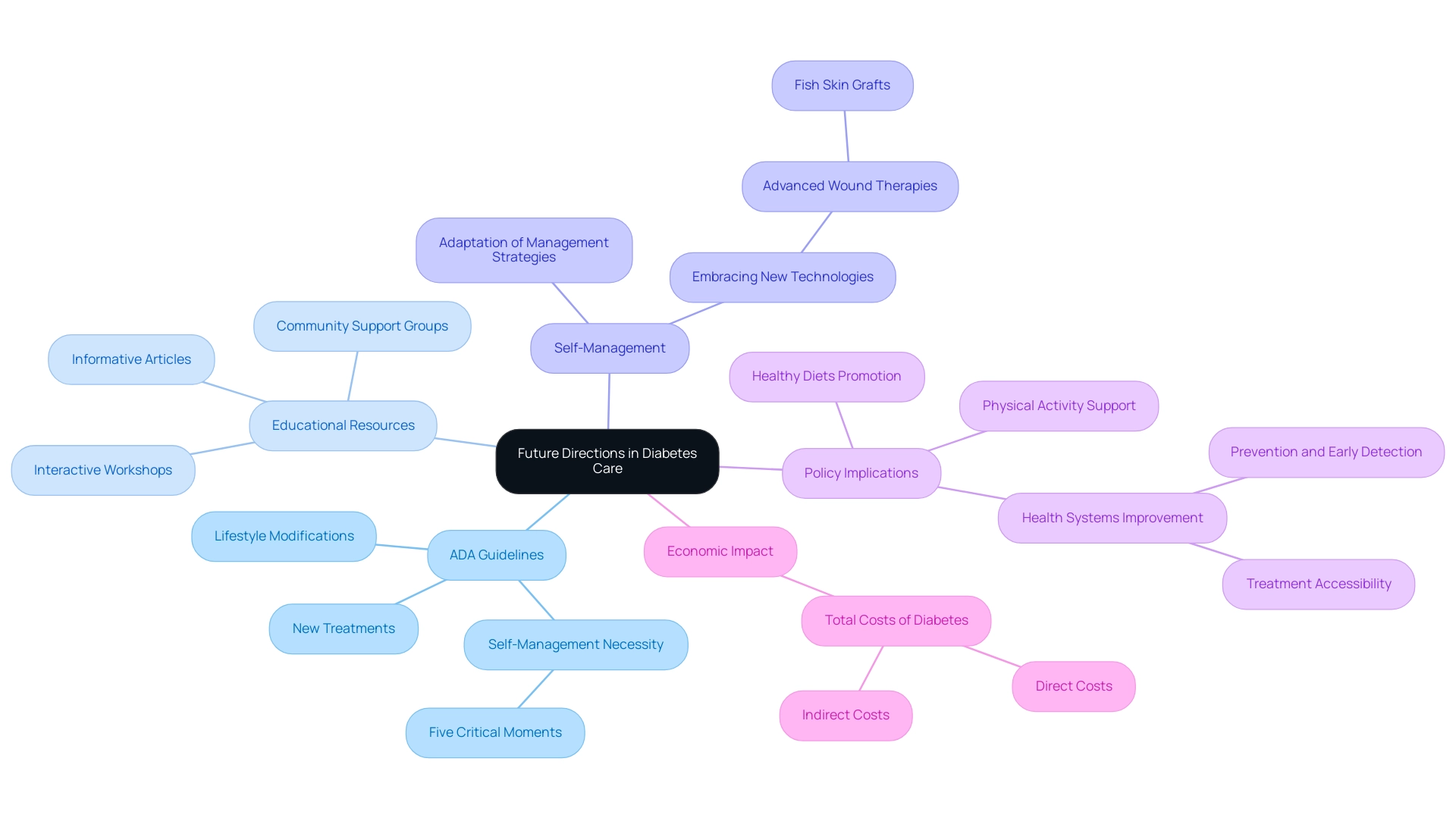
Future Directions in Diabetes Care: Staying Informed with ADA Guidelines
As the terrain of blood sugar management progresses, it becomes increasingly vital for individuals to remain informed about future paths and current studies. The ADA clinical guidelines emphasize the necessity for individuals to engage with the latest discoveries and progress in blood sugar regulation, which include new treatments, technologies, and lifestyle modifications. Significantly, the new guidance highlights assessing the necessity for self-management and education regarding chronic conditions at five critical moments throughout an individual's journey, reinforcing the importance of proactive involvement in their care.
T2DSolutions is a recently established resource center focused on enhancing diabetes care for individuals with Type 2 and Type 3 diabetes. This hub provides various educational resources, including:
- Informative articles
- Interactive workshops
- Community support groups aimed at helping individuals stay informed about best practices
By actively engaging with these resources, patients can adapt their management strategies, embrace new technologies such as advanced wound therapies—including recent additions like fish skin grafts—and ultimately improve their health outcomes.
Dr. Tedros Adhanom Ghebreyesus, the WHO Director-General, has emphasized, 'To bring the global epidemic of diabetes-related conditions under control, countries must urgently take action.' This begins with implementing policies that promote healthy diets and physical activity, and, most importantly, health systems that provide prevention, early detection, and treatment. This quote emphasizes the urgency for thorough policies in managing metabolic disorders, which corresponds with T2DSolutions’ mission to offer timely and pertinent assistance for individuals. Additionally, the financial effect of blood sugar conditions is considerable, with overall expenses projected at $413 billion in 2022, highlighting the wider consequences of effective care and the essential role of individual education.
This commitment to education and adaptation, exemplified by T2DSolutions, positions patients to navigate their diabetes management more effectively.
Conclusion
The American Diabetes Association (ADA) clinical guidelines serve as a vital framework for diabetes care, emphasizing the importance of personalized treatment plans, patient education, and adherence to evidence-based practices. By understanding and implementing these guidelines, patients can significantly improve their health outcomes and engage in proactive self-management strategies. The recent updates to the guidelines reflect a commitment to incorporating the latest research and innovative approaches in diabetes management, ensuring that care is tailored to individual needs.
Lifestyle modifications, regular monitoring, and effective communication with healthcare providers are essential components of successful diabetes management. Resources such as T2DSolutions play a crucial role in empowering patients by providing educational materials and community support, helping them navigate their diabetes journey with confidence. As the landscape of diabetes care continues to evolve, staying informed about advancements and engaging with available resources will be paramount for patients striving for optimal health.
Ultimately, the ADA guidelines underscore that effective diabetes management is not solely about medication; it encompasses a holistic approach that includes lifestyle changes, technology integration, and ongoing education. By embracing these principles, patients can take charge of their health, reduce the economic burden of diabetes, and enhance their overall quality of life.



