Overview
The article titled "Understanding ADA Diabetes Management Guidelines: A Caring Overview" aims to provide a compassionate overview of the American Diabetes Association's (ADA) updated guidelines for diabetes management. It emphasizes the importance of personalized care and the integration of technology, which can be crucial for individuals navigating their diabetes journey.
Key elements of the 2025 recommendations are detailed, highlighting the significance of individualized treatment plans. Continuous glucose monitoring plays a vital role, as does the necessity for psychosocial support. These components are all designed to improve health outcomes for individuals with diabetes.
It's understandable to feel overwhelmed by these guidelines, but remember, you're not alone in this journey. The ADA's approach is about supporting you every step of the way, ensuring that your unique needs are met with care and understanding.
Introduction
In the constantly changing world of diabetes management, the American Diabetes Association (ADA) is dedicated to refining its guidelines. This commitment ensures that healthcare providers have access to the most effective strategies for patient care. The updates for 2025 highlight a patient-centered approach, integrating the latest research and technological advancements to enhance treatment outcomes.
It's essential to recognize the vital role of continuous glucose monitoring and the importance of psychosocial support. These guidelines aim not only to improve individual health but also to address the broader disparities in diabetes care. This article explores the key components of the ADA's latest recommendations, illustrating how they can transform the lives of those living with diabetes.
You're not alone in this journey. We are here to support you every step of the way, empowering both patients and healthcare professionals in their collaborative quest for better health. Together, we can navigate this path, ensuring that everyone receives the care and understanding they deserve.
Overview of ADA Diabetes Management Guidelines
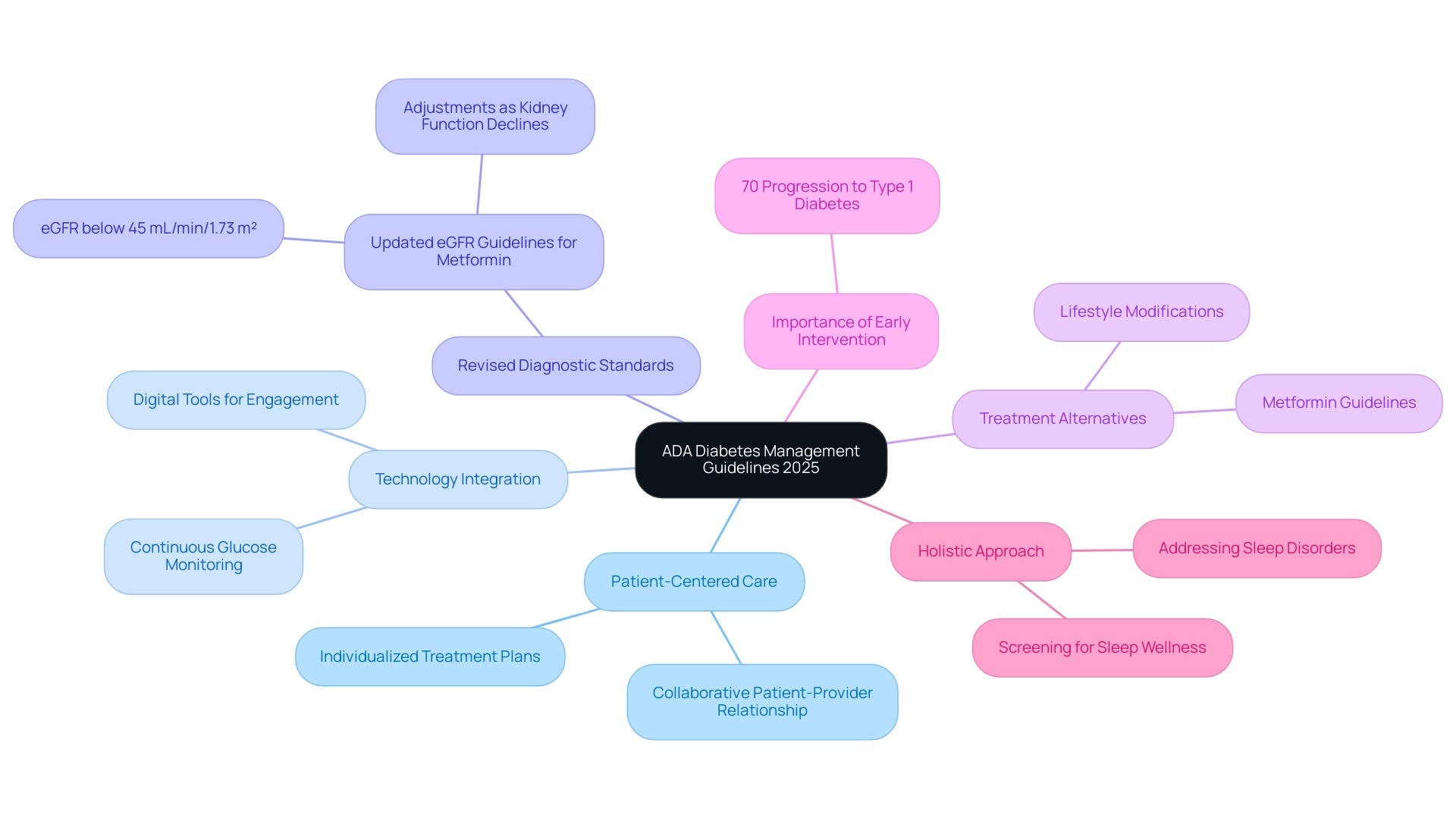
The ADA diabetes management guidelines provide a vital framework for healthcare providers, enabling them to deliver effective and personalized care to individuals living with diabetes. Updated annually, these recommendations reflect the most current research and clinical practices, ensuring they remain both relevant and evidence-based. The 2025 recommendations place a strong emphasis on a patient-centered approach, prioritizing individualized care tailored to the unique needs and circumstances of each patient.
Essential elements of the 2025 recommendations consist of revised diagnostic standards and treatment alternatives that correspond with the newest progress in blood sugar control. For instance, Metformin, a cornerstone medication for Type 2 Diabetes, should not be initiated in individuals with an estimated glomerular filtration rate (eGFR) below 45 mL/min/1.73 m², and adjustments must be made as kidney function declines. This highlights the importance of regular monitoring and individualized treatment plans, ensuring that each patient's journey is met with understanding and care.
The integration of technology in ADA diabetes management guidelines is another significant focus of the 2025 guidelines. Healthcare providers are encouraged to utilize digital tools and continuous glucose monitoring systems to enhance engagement and improve glycemic control. This approach not only empowers patients but also fosters a collaborative relationship between patients and their healthcare teams, reminding you that you are not alone in this journey.
Recent statistics highlight the urgency of effective diabetes control; approximately 70% of children who develop more than two autoantibodies will progress to Type 1 Diabetes within ten years. This statistic underscores the necessity for early intervention and proactive strategies, reinforcing the importance of seeking support early on.
Real-world examples of patient-centered care demonstrate the successful application of these principles. A significant case study on hypertension control in young individuals with Type 1 Diabetes highlights the importance of regular blood pressure assessments and personalized treatment objectives, directly aligning with the ADA recommendations. By focusing on lifestyle modifications and pharmacological interventions, healthcare providers can significantly improve cardiovascular health outcomes in this population, showing that personalized care truly makes a difference.
Additionally, the 2025 recommendations promote thorough screening for sleep wellness in individuals with blood sugar issues, acknowledging the effect of sleep disorders on general health and management of blood sugar levels. This holistic approach is essential for addressing the multifaceted challenges faced by patients, ensuring that every aspect of health is considered.
Expert views on the ADA diabetes management guidelines highlight their importance in enhancing health management results. Charles “Chuck” Henderson, CEO, states, "Enhancing the lives of individuals affected by this condition is a key part of the ADA’s mission." The ADA diabetes management guidelines provide the reliable assistance required for individuals living with the condition and those supporting them to handle the illness and flourish until a remedy is discovered. Healthcare experts acknowledge that these guidelines not only offer reliable assistance for individuals dealing with the illness but also enable caregivers to manage the condition effectively.
By promoting a cooperative atmosphere, the ADA diabetes management guidelines aim to improve the quality of life for everyone affected by this condition.
At T2DSolutions, we are committed to supporting newly diagnosed patients by providing tailored resources and education that adhere to the ADA diabetes management guidelines. As a new resource center for education and community support regarding blood sugar conditions, T2 Solutions aims to empower individuals with the knowledge and tools necessary to navigate their healthcare effectively. Remember, we are here to support you every step of the way.
Classification of Diabetes: Types and Implications
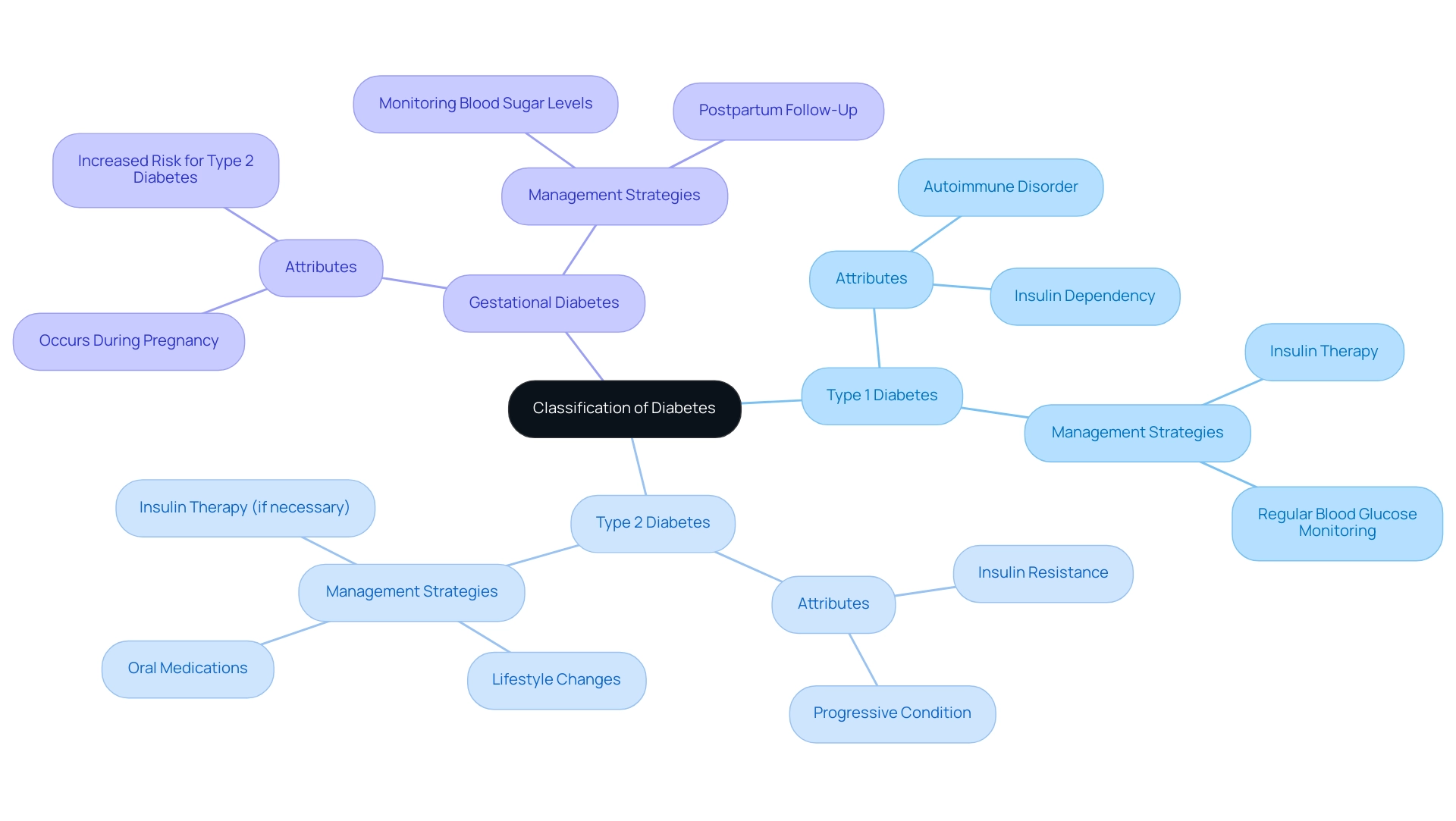
Diabetes is a condition that can take on several distinct forms, primarily Type 1, Type 2, and gestational types, each with its own unique attributes and handling implications. Type 1 is an autoimmune disorder where the pancreas struggles to produce insulin, making lifelong insulin therapy essential for effective management. On the other hand, Type 2 diabetes mellitus, which accounts for about 90-95% of all cases, is characterized by insulin resistance.
This condition can often be managed through lifestyle changes, such as adopting a healthier diet and incorporating regular exercise, alongside oral medications or insulin therapy when necessary.
Gestational diabetes occurs during pregnancy and typically resolves after childbirth. However, it significantly increases the risk of developing Type 2 diabetes later in life. Recent statistics show a concerning rise in gestational glucose intolerance, with the percentage of mothers diagnosed increasing from 6.0% in 2016 to 8.3% in 2021, as noted by Joyce A. Martin. This trend underscores the importance of monitoring and managing blood sugar levels during and after pregnancy.
The diabetes management guidelines from the American Diabetes Association (ADA) emphasize the necessity for personalized management strategies tailored to each type of diabetes. For instance, individuals with Type 1 diabetes require a comprehensive approach that includes regular blood glucose monitoring and insulin administration. Conversely, those with Type 2 diabetes may find success through a combination of lifestyle changes and pharmacological interventions, reflecting the progressive nature of the condition.
Understanding the classification of diabetes is crucial for effective treatment. The implications of these classifications extend beyond immediate management; they influence long-term health outcomes. For example, the age-adjusted prevalence of undiagnosed diabetes-related conditions has remained steady at 4.2% from 2017 to March 2020 and from August 2021 to August 2023. This highlights the necessity for ongoing monitoring and awareness of its prevalence among U.S. adults.
Notably, the prevalence of undiagnosed diabetes-related conditions varies significantly with weight status, increasing from 1.6% in individuals with normal weight to 7.9% in those classified as obese.
Real-life examples illustrate how classification impacts treatment strategies. For instance, a patient with Type 1 diabetes may require a different approach compared to a patient with Type 2, who might initially manage their condition through lifestyle changes before considering medication. Understanding these differences is vital for healthcare providers to deliver effective, personalized care.
The methodology of the National Health and Nutrition Examination Survey, which involved interviews and health examinations conducted in mobile centers, provides valuable context regarding the data collection methods used to evaluate trends in blood sugar disorder prevalence over time. This case study highlights the significance of precise data gathering in understanding trends related to diabetes.
In summary, the categorization of diabetes types is not merely theoretical; it carries substantial consequences for management approaches and health outcomes. The ADA diabetes management guidelines serve as an essential resource for healthcare professionals, ensuring that individuals receive the most suitable care based on their specific condition. Remember, you're not alone in this journey—we are here to support you every step of the way.
Diagnostic Testing and Criteria for Diabetes Management
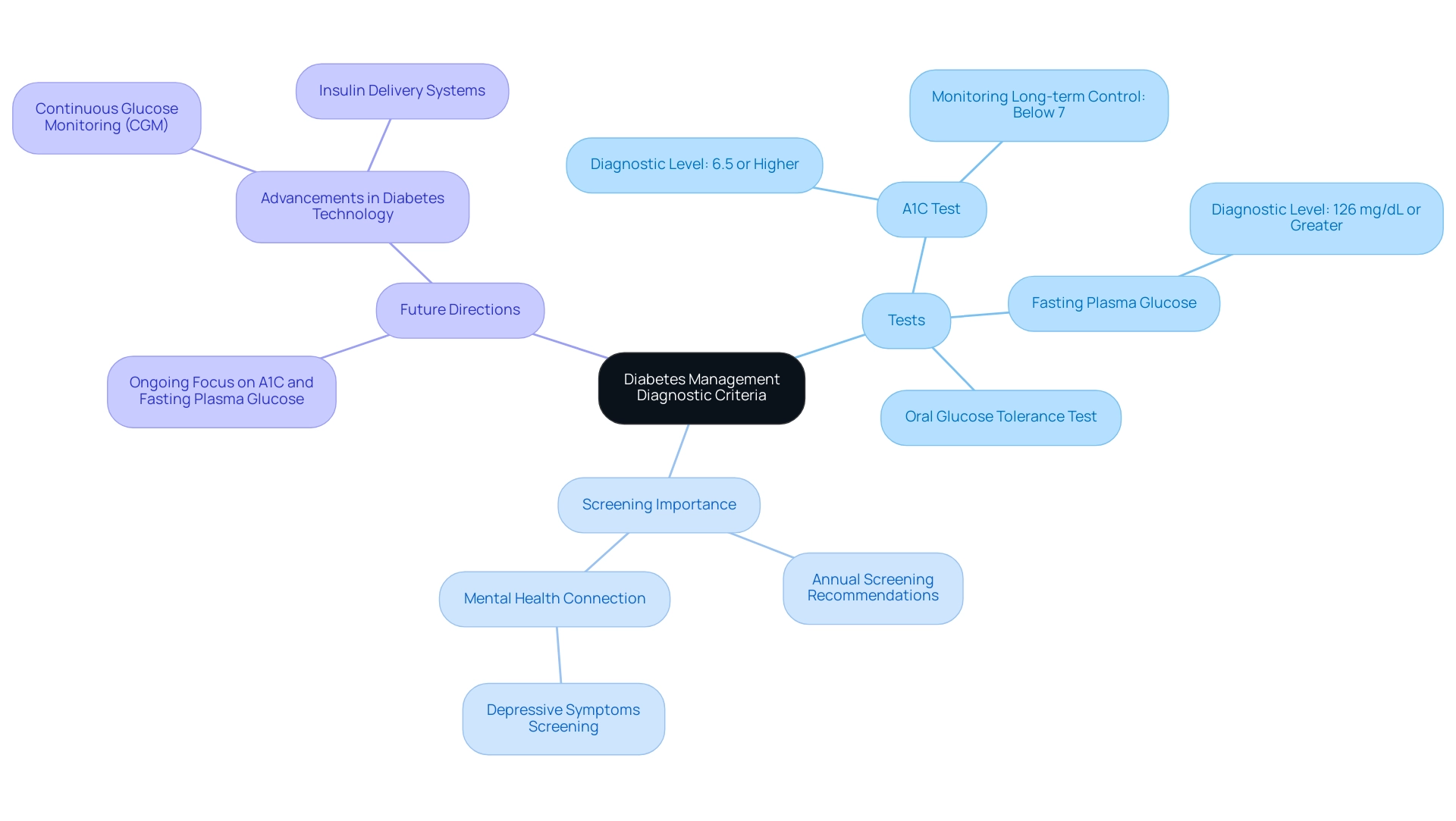
The ADA guidelines establish essential diagnostic criteria for blood sugar conditions, focusing on the A1C test, fasting plasma glucose, and oral glucose tolerance tests. An A1C level of 6.5% or higher is indicative of the condition, while fasting plasma glucose levels of 126 mg/dL or greater confirm the diagnosis. Regular screening is crucial, especially for individuals at risk, including those with obesity or a family history of blood sugar issues. This proactive approach allows for early detection and intervention, which can make a significant difference.
The importance of the A1C test cannot be overstated; it not only aids in diagnosing the condition but also serves as a key metric for monitoring long-term glucose control. Research shows that maintaining an A1C level below 7% can significantly reduce the risk of diabetes-related complications. Additionally, the ADA recommends annual screening for depressive symptoms in all individuals with this condition, recognizing the vital connection between mental health and effective management.
Conducting at least annual screenings for depressive symptoms is essential to ensure comprehensive care for those living with this condition. You're not alone in this journey, and these screenings can provide valuable insights for better overall health.
Looking ahead to 2025, the ADA's diagnostic criteria will continue to emphasize the importance of both the A1C test and fasting plasma glucose in identifying the condition. The ADA diabetes management guidelines are designed to offer clinicians, patients, and researchers a clear framework for managing blood sugar conditions. As Charles “Chuck” Henderson, CEO, stated, "Enhancing the lives of individuals impacted by this condition is a key part of the ADA’s mission."
The ADA provides the reliable assistance needed for individuals living with this condition and those supporting them. Together, we can manage the illness and strive for a brighter future until a cure is discovered.
For instance, a case study on blood sugar management technology highlights the role of continuous glucose monitoring (CGM) and insulin delivery systems. Advocating for their early initiation tailored to individual needs ensures that patients and caregivers receive the necessary training and support to utilize these technologies effectively, ultimately enhancing the management of the condition.
Real-world examples illustrate the effectiveness of A1C testing in managing blood sugar conditions. Endocrinologists emphasize that accurate A1C testing is crucial for diagnosing the condition and guiding treatment decisions. As the ADA continues to refine its guidelines, the focus remains on empowering individuals with the knowledge and resources needed to manage their condition effectively. Remember, we are here to support you every step of the way, fostering a proactive approach to health and well-being.
Treatment Approaches for Type 1 and Type 2 Diabetes
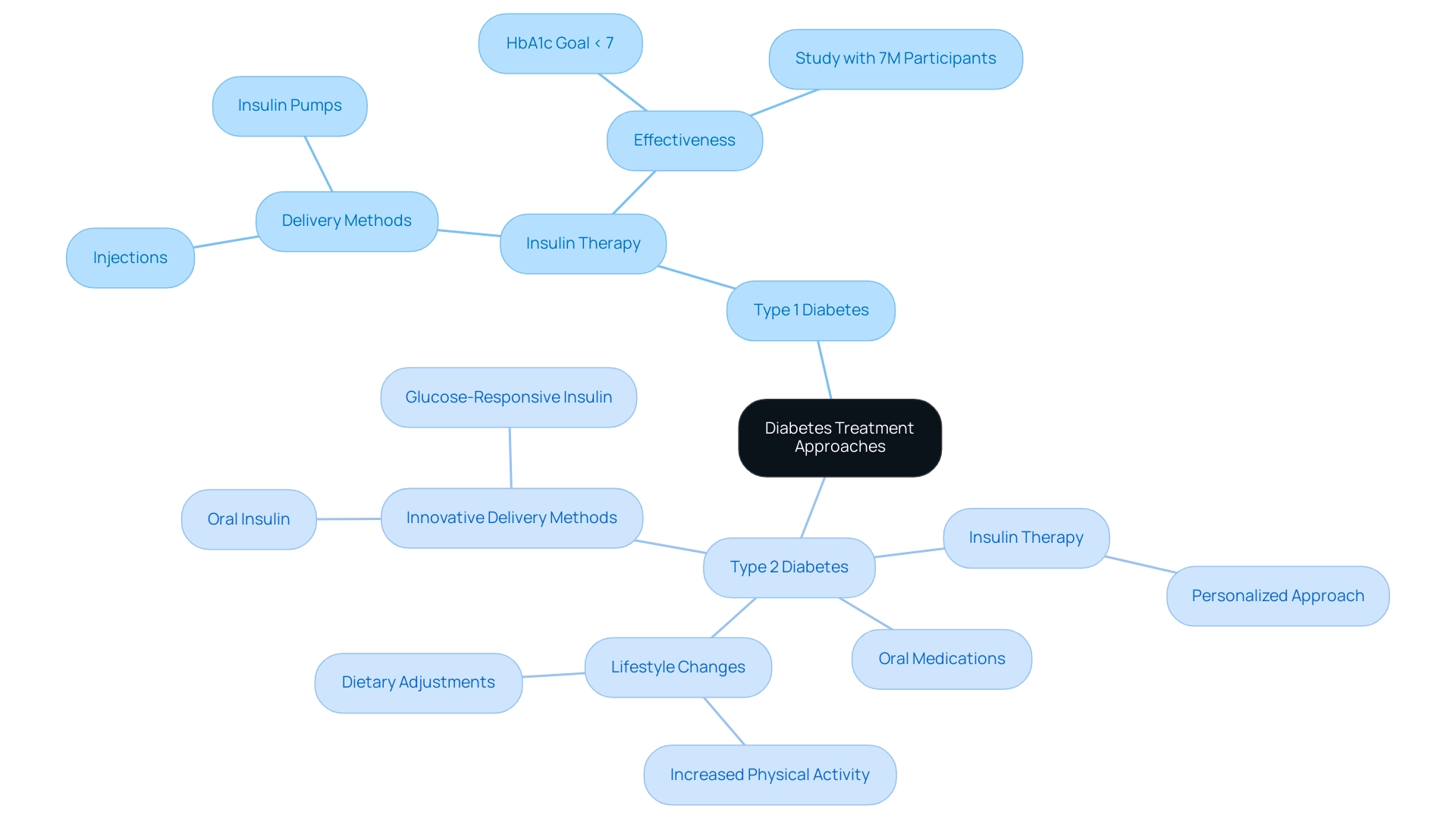
Treatment methods for diabetes can feel overwhelming, especially when considering the differences between Type 1 and Type 2. For those living with Type 1, insulin therapy is essential. This involves various delivery methods, such as injections and insulin pumps, to help maintain glycemic control. Recent studies show that insulin therapy can be quite effective, with many patients reaching an HbA1c goal of less than 7%, as recommended by the ADA for most nonpregnant adults. This highlights the vital role of insulin in effectively managing Type 1 diabetes.
A significant study involving over 7 million participants underscores the effectiveness of insulin therapy in achieving these important targets. On the other hand, managing Type 2 diabetes often begins with lifestyle changes, including dietary adjustments and increased physical activity. These foundational strategies are crucial, as they can lead to notable improvements in blood glucose levels and overall health.
As the condition progresses, individuals may find they need oral medications or insulin therapy tailored to their specific needs. The ADA diabetes management guidelines advocate for a personalized approach to treatment, considering individual preferences, existing health conditions, and the risk of diabetes-related complications. Lea Smircic-Duvnjak, a consultant in this field, emphasizes the importance of customizing blood sugar management strategies to fit individual circumstances.
Current trends in Type 2 treatment highlight the significance of insulin-to-carbohydrate ratios and correction factors. These are essential for calculating insulin doses based on carbohydrate intake and current glucose levels. Moreover, ongoing research into innovative insulin delivery methods, such as oral administration and glucose-responsive insulins, shows promise in enhancing safety and convenience. A case study on these novel delivery methods suggests that early findings indicate they may offer pharmacokinetic and pharmacodynamic profiles comparable to traditional subcutaneous insulin, potentially reducing the risk of hypoglycemic events.
Real-world examples reflect the positive impact of lifestyle modifications on Type 2 diabetes control. Patients who embrace a balanced diet and regular exercise often share their experiences of improved blood sugar control and overall well-being. These lifestyle adjustments not only help in managing blood sugar levels but also contribute to a better quality of life.
In conclusion, the ADA diabetes management guidelines for 2023 and 2024 stress the importance of individualized treatment plans that cater to each person's unique situation. By incorporating insights from specialists and the latest research findings, healthcare professionals can offer customized approaches that enhance the management of both Type 1 and Type 2 diabetes, ultimately empowering individuals to take charge of their health. Remember, you're not alone in this journey; support and resources are available to help you every step of the way.
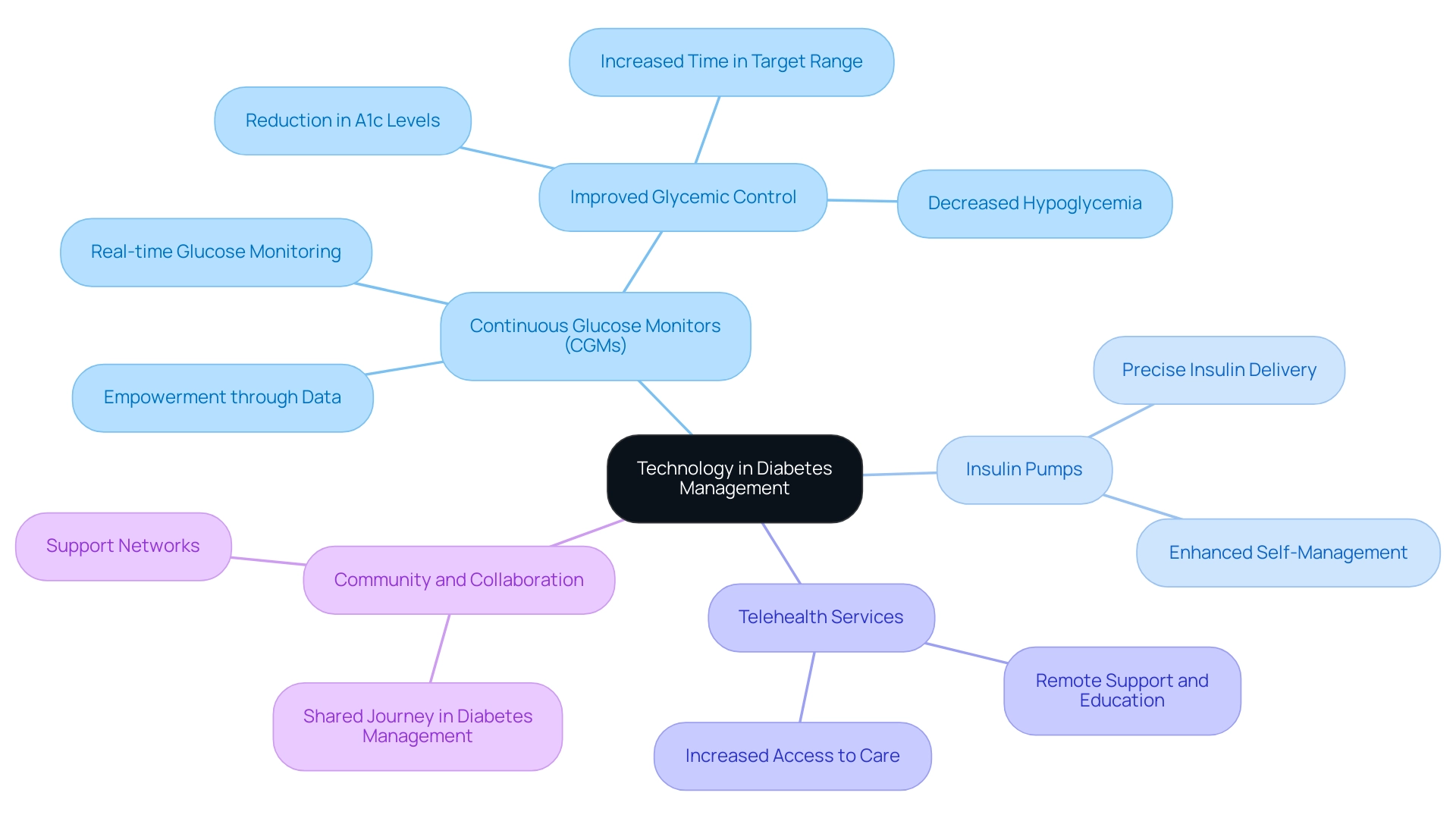
The Role of Technology in Diabetes Management
The landscape of managing this condition has been significantly reshaped by technological advancements, leading to more efficient and effective care strategies. Continuous glucose monitors (CGMs) are at the forefront of this transformation, providing real-time glucose readings that empower individuals to make informed choices about their diet and insulin administration. Research indicates that the implementation of CGMs has resulted in notable improvements in glycemic control, with studies showing reductions in A1c levels and increased time spent within target glucose ranges.
For instance, a study titled 'Impact of Continuous Glucose Monitors on Glycemic Control' evaluated the effectiveness of CGMs among patients with type 2 who were not using insulin or were on basal insulin only. The findings revealed significant improvements in glycemic control, highlighting the potential of CGMs to address health disparities in the treatment of this condition by providing critical data that can lead to better health outcomes.
Insulin pumps also play a crucial role in enhancing the management of this condition by delivering precise doses of insulin, which helps maintain optimal glycemic control. The ADA diabetes management guidelines strongly advocate for the incorporation of these technologies into care, emphasizing their significance in encouraging individual self-management and involvement. Experts emphasize that the use of CGMs enables individuals to manage their condition more effectively, reducing dependence on medications and minimizing side effects linked to conventional treatment approaches.
As Ovalle noted, "You tell people, ‘Wear this and try to keep it in the lines’ and they figure it out — without a drug or the further cost of another medication and side effects and visits."
Moreover, the rise of telehealth services has expanded access to care for individuals with blood sugar issues, enabling patients to receive timely support and education from healthcare professionals remotely. This comprehensive approach to blood sugar control, which integrates technology with community assistance, highlights that overseeing this condition is a shared journey. By leveraging these advancements, individuals can enhance their quality of life and achieve better health outcomes.
The emphasis on community and teamwork is crucial, as it corresponds with 2 Solutions mission to empower individuals and families in their health journey. You're not alone in this journey, and we are here to support you every step of the way.
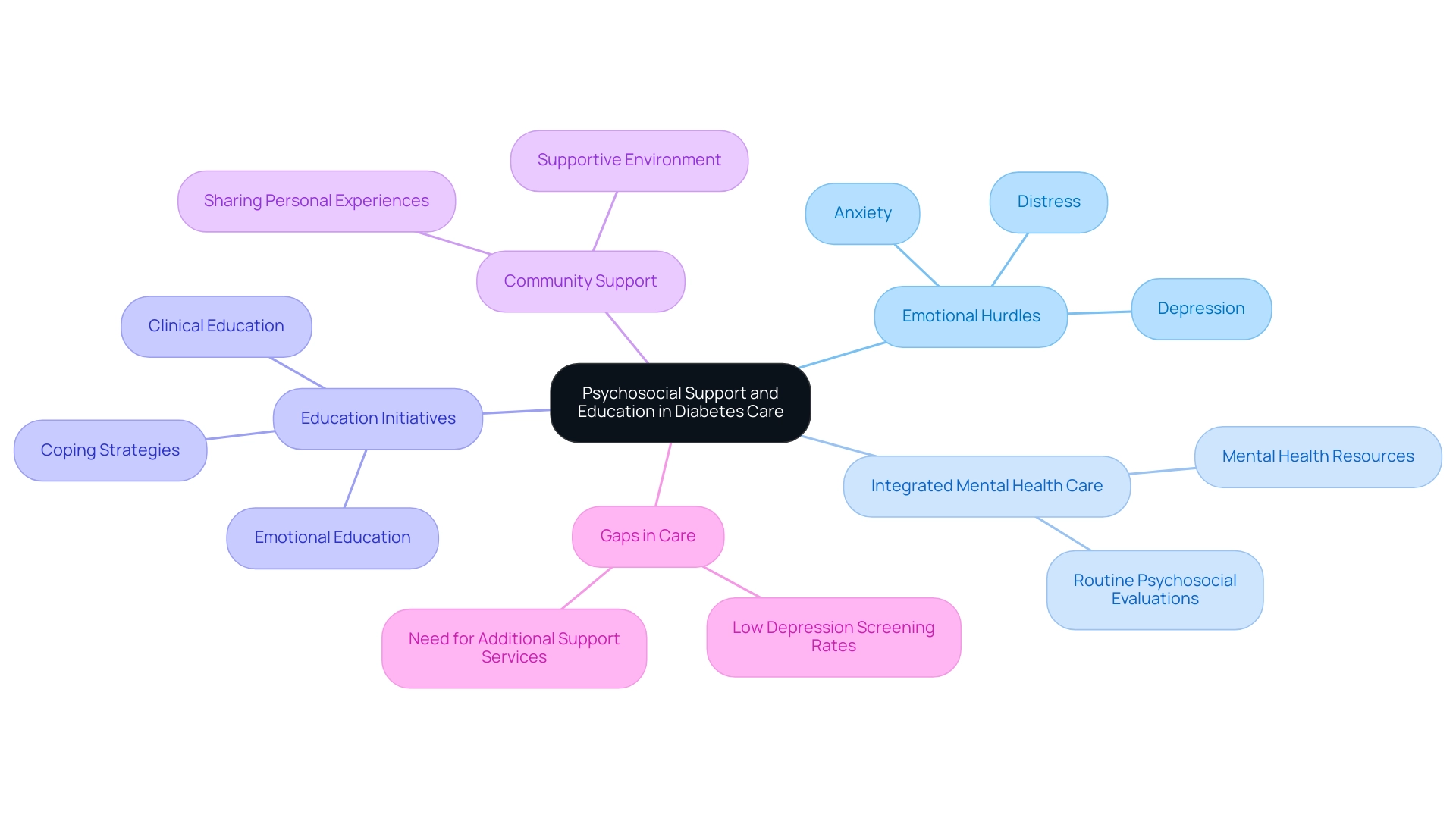
Psychosocial Support and Education in Diabetes Care
The ADA diabetes management guidelines highlight the essential role of psychosocial support in managing this condition. It's understandable that patients frequently encounter emotional hurdles such as distress, anxiety, and depression, which can significantly hinder their ability to effectively manage their condition. Research indicates that individuals with diabetes are 20% more likely to experience anxiety compared to those without it, emphasizing the urgent need for integrated mental health care.
In response, the guidelines advocate for routine psychosocial evaluations and the inclusion of mental health resources into care protocols. Education initiatives that address both clinical and emotional aspects of diabetes are essential in empowering individuals. T2DSolutions exemplifies this by offering comprehensive resources that equip individuals with coping strategies to enhance their overall well-being and resilience. Community initiatives that encourage sharing personal experiences foster a supportive environment, which has been shown to improve health outcomes through collective knowledge and encouragement.
This emphasis on creating a nurturing community is fundamental to T2D Solutions' mission, as it fosters resilience and hope among individuals coping with diabetes.
Furthermore, the ADA diabetes management guidelines for 2023 and 2024 emphasize the significance of mental health assessments. Research indicates that only half of healthcare providers utilize depression screening tools for individuals with type 2 diabetes, highlighting a gap in care. This gap underscores the need for a proactive approach to mental health, as positive screenings for depression or related distress indicate a clear necessity for additional support services.
As Barbara J. Anderson from Baylor College of Medicine states, "From economic, public health, and humanitarian perspectives, identifying and addressing the mental health comorbidities among individuals with diabetes-related conditions should be a priority." Expert insights from mental health specialists reinforce this perspective, advocating for the prioritization of identifying and addressing mental health comorbidities among individuals with blood sugar issues. By integrating psychosocial support into the management of metabolic disorders, healthcare providers can significantly enhance the quality of care and improve patient outcomes, aligning with the holistic approach championed by T2D Solutions. You're not alone in this journey; we are here to support you every step of the way.
Recent Updates to ADA Guidelines: What You Need to Know
The 2025 ADA diabetes management guidelines introduce several significant updates that reflect the evolving nature of managing blood sugar conditions. A key recommendation is the use of continuous glucose monitoring (CGM) for adults with Type 2 diabetes who are on non-insulin glucose-lowering agents. This advancement allows for more precise tracking of glucose levels, enabling both patients and healthcare providers to make informed decisions about treatment adjustments in real-time.
Research indicates that CGM can lead to improved glycemic control and reduced hypoglycemic events, ultimately enhancing the quality of life for individuals managing Type 2 diabetes. You're not alone in this journey; many have found that these tools help them feel more in control.
Moreover, the guidelines emphasize the critical need to address health disparities in managing blood sugar conditions. They promote fair access to resources and support, acknowledging that socioeconomic factors can greatly influence the management of diabetes. As Charles “Chuck” Henderson, CEO of the ADA, stated, "Enhancing the lives of individuals impacted by this condition is a key part of the ADA’s mission."
By promoting strategies that ensure all patients receive the necessary tools and education, the ADA aims to improve health outcomes across diverse populations. It’s essential to remember that support is available, and the community is here for you.
In practice, the implementation of these guidelines is supported by case studies highlighting the diagnostic challenges in pediatric endocrinology. For instance, distinguishing between Type 1 and Type 2 diabetes in children can be particularly complex due to overlapping symptoms and the increasing prevalence of obesity. Accurate diagnosis is essential, as it directly influences educational approaches and nutritional advice tailored to each patient's needs. This case study demonstrates the significance of the principles in ensuring effective management from an early age.
Additionally, the recommendations suggest that blood pressure be assessed at each regular appointment for youth, with special focus on those displaying elevated blood pressure. This proactive approach is crucial, as hypertension is a common comorbidity in blood sugar disorders that can exacerbate health complications. It’s understandable to feel overwhelmed, but taking these steps can make a significant difference.
Overall, the 2025 ADA diabetes management guidelines equip healthcare providers with the latest evidence-based practices, ensuring they are well-prepared to enhance individual outcomes and promote a more inclusive approach to managing blood sugar. T2DSolutions aims to serve as a comprehensive resource hub for newly diagnosed patients, providing access to educational materials and community support that align with these guidelines. The ADA's Standards of Care in Diabetes—2025 serves as a vital resource for clinicians, researchers, and policymakers to enhance diabetes care. Remember, you are not alone, and we are here to support you every step of the way.

Conclusion
The 2025 updates to the American Diabetes Association (ADA) guidelines mark a significant step forward in diabetes management, focusing on a patient-centered approach that prioritizes individualized care. Key elements, such as the integration of continuous glucose monitoring and the importance of psychosocial support, are designed to empower both patients and healthcare providers. These guidelines not only aim to improve clinical outcomes but also strive to address health disparities, ensuring that everyone has access to the resources needed for effective diabetes management.
By nurturing a collaborative relationship between patients and their healthcare teams, the ADA guidelines seek to enhance the quality of life for those living with diabetes. The emphasis on regular monitoring, personalized treatment plans, and the incorporation of technology reflects a commitment to providing comprehensive care tailored to each patient's unique needs. Furthermore, recognizing the role of mental health in diabetes management underscores the holistic approach essential for effective care.
As diabetes management continues to evolve, the ADA guidelines serve as a vital resource for healthcare professionals, equipping them with the latest evidence-based practices. By implementing these recommendations, we can establish a more inclusive and effective diabetes care framework, ultimately leading to better health outcomes for individuals affected by diabetes. Embracing these advancements in care is crucial in the journey toward improved diabetes management and support for all patients. Remember, you're not alone in this journey; we are here to support you every step of the way.
Frequently Asked Questions
What is the purpose of the ADA diabetes management guidelines?
The ADA diabetes management guidelines provide a framework for healthcare providers to deliver effective and personalized care to individuals living with diabetes, ensuring that recommendations are based on the latest research and clinical practices.
How often are the ADA diabetes management guidelines updated?
The ADA diabetes management guidelines are updated annually to reflect the most current research and clinical practices.
What is emphasized in the 2025 recommendations of the ADA guidelines?
The 2025 recommendations emphasize a patient-centered approach, prioritizing individualized care tailored to each patient's unique needs and circumstances.
What are some key elements included in the 2025 recommendations?
Key elements include revised diagnostic standards, treatment alternatives based on recent advancements in blood sugar control, and the importance of regular monitoring and individualized treatment plans.
What specific guidance is provided regarding Metformin in the 2025 guidelines?
Metformin should not be initiated in individuals with an estimated glomerular filtration rate (eGFR) below 45 mL/min/1.73 m², and adjustments must be made as kidney function declines.
How is technology integrated into the ADA diabetes management guidelines?
The guidelines encourage healthcare providers to use digital tools and continuous glucose monitoring systems to enhance patient engagement and improve glycemic control.
What recent statistics highlight the importance of diabetes management?
Approximately 70% of children who develop more than two autoantibodies will progress to Type 1 Diabetes within ten years, emphasizing the need for early intervention and proactive strategies.
Can you provide an example of patient-centered care in diabetes management?
A case study on hypertension control in young individuals with Type 1 Diabetes shows that regular blood pressure assessments and personalized treatment objectives can significantly improve cardiovascular health outcomes.
What additional screening is promoted in the 2025 recommendations?
The guidelines promote thorough screening for sleep wellness, recognizing the impact of sleep disorders on overall health and blood sugar management.
What is the ADA's mission according to healthcare experts?
The ADA's mission focuses on enhancing the lives of individuals affected by diabetes, providing reliable assistance for managing the condition effectively.
How does T2DSolutions support newly diagnosed patients?
T2DSolutions offers tailored resources and education that align with the ADA diabetes management guidelines, empowering individuals to navigate their healthcare effectively.
