Overview
The article focuses on understanding blood glucose monitoring sensors, emphasizing their significance for patients managing diabetes and the various types available, including invasive and non-invasive methods. It supports this by detailing how these sensors provide critical real-time data for effective diabetes management, highlighting advancements in technology and the importance of education and community support for patients and caregivers.
Introduction
As diabetes continues to rise at alarming rates, effective management tools have become essential for those affected by the condition. Blood glucose monitoring sensors stand at the forefront of this battle, providing real-time insights that empower patients and caregivers to make informed decisions regarding diet, exercise, and medication.
With over 10 million Americans relying on these advanced systems, particularly Continuous Glucose Monitoring (CGM), the shift from traditional fingerstick methods to more accurate and convenient technologies is evident. The urgent need for such innovations is underscored by the increasing diagnosis of type 2 diabetes among younger populations.
This article explores the various types of blood glucose monitoring technologies, their functionalities, and the critical role they play in enhancing diabetes management. By understanding these tools, patients can take proactive steps toward better health outcomes and improved quality of life.
Introduction to Blood Glucose Monitoring Sensors
Blood glucose monitoring sensors are crucial for individuals controlling their condition, as they provide real-time information that enables patients and caregivers to make knowledgeable choices regarding diet, exercise, and medication. Currently, over 10 million Americans rely on insulin and benefit from Continuous Glucose Monitoring (CGM) systems that include a blood glucose monitoring sensor, which offers improved accuracy and convenience compared to traditional fingerstick methods. Alarmingly, during the same period, 5,293 children and adolescents aged 10 to 19 years were diagnosed with type 2 diabetes, highlighting the urgent need for effective diabetes management technologies.
These advanced blood glucose monitoring sensors are designed to alert users to fluctuations in sugar levels, which is crucial for preventing both hyperglycemia and hypoglycemia. Moreover, innovative efforts such as Afon's development of a blood glucose monitoring sensor, supported by the National Institutes of Health and the University of Kentucky’s Igniting Research Collaboration Pilot Program, exemplify the ongoing advancements in this field. Comprehending how these sensors operate and their importance can empower patients on their healthcare journey, improving overall health control.
Additionally, the retail segment for blood glucose monitoring sensor systems is expanding, with companies like Omron Healthcare, Inc. planning to increase their presence in markets such as India. T2DSolutions is dedicated to offering extensive resources and community assistance for Type 2 and Type 3 blood sugar control, including educational materials, support groups, and access to the latest technology. These initiatives guarantee that newly diagnosed patients possess the knowledge and resources essential for effective self-care, positioning T2D Solutions as a crucial asset in their health journey.
Exploring Types of Blood Glucose Monitoring Technologies
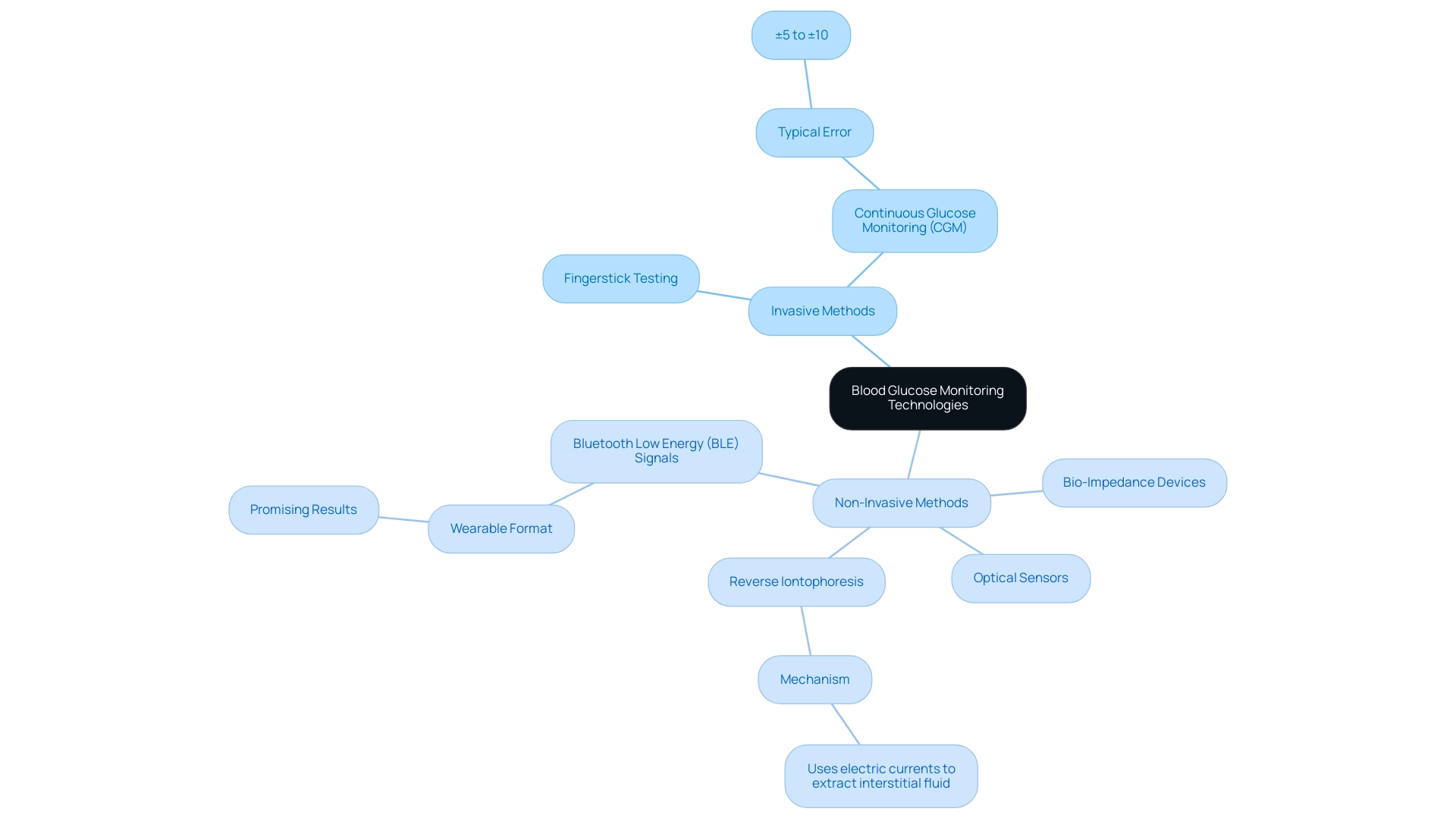
a2d Solutions, we acknowledge the significance of effective management of the condition, particularly for individuals recently diagnosed with Type 2 and Type 3. As a new resource hub dedicated to education and community support, Td Solutions aims to provide valuable insights and assistance to patients navigating their health journey. Blood glucose monitoring sensors can be classified into two main categories: invasive and non-invasive methods.
Invasive techniques, such as traditional fingerstick testing and blood glucose monitoring sensors, including Continuous Glucose Monitoring (CGM) systems, have long been the standard in diabetes management. Fingerstick testing involves using a lancet to obtain a blood sample, which is then analyzed with a glucometer for immediate sugar readings. In contrast, CGM systems utilize a blood glucose monitoring sensor that is a tiny device inserted beneath the skin to continuously monitor sugar concentrations, providing real-time information and notifications for variations in blood sugar.
The typical error for CGM models is stated at ±5% to ±10%, highlighting their precision in monitoring sugar content.
Conversely, non-invasive techniques are developing as creative substitutes that seek to assess sugar concentrations without the necessity for skin penetration. Notable technologies in this category include optical sensors and bio-impedance devices, which, while still largely in development, show promise in enhancing the accuracy and reliability of the blood glucose monitoring sensor. For example, a recent development using Bluetooth Low Energy (BLE) signals has shown promising outcomes in detecting blood sugar levels in a wearable format, indicating a possible change in how this condition can be addressed.
A review of new technologies in sugar detection, titled 'Emerging Technologies in Sugar Detection,' emphasizes mechanisms such as surface plasmon resonance and fluorescence, demonstrating their potential uses for enhancing sugar measurement precision. As noted by Faheem et al., 'the work further analyzes the results using classification-based machine learning algorithms and achieves a correlation coefficient of 97% and p-value 5.6e-6,' emphasizing the effectiveness of these emerging technologies. Additionally, reverse iontophoresis is a specific non-invasive method that uses electric currents to extract interstitial fluid for glucose measurement, which can be integrated with a blood glucose monitoring sensor to offer high accuracy and further demonstrate the potential of non-invasive technologies. The choice between invasive and non-invasive methods involves weighing their respective advantages and disadvantages.
Invasive systems are known for their high accuracy, while non-invasive technologies are still refining their accuracy but offer the appeal of convenience and reduced discomfort. Comprehending these distinctions enables patients and caregivers to choose the technology that suits their lifestyle and health objectives, ensuring a more customized and effective approach to care. We encourage newly diagnosed patients to explore T2D Solutions for more resources and community support as they embark on their diabetes management journey.
How to Use Blood Glucose Monitoring Sensors
To effectively utilize a blood glucose monitoring sensor, start by carefully inserting the sensor as per the manufacturer's guidelines, typically placed on the abdomen or arm. Following insertion, allow for an initial calibration period, which may take up to two hours, before you begin receiving sugar readings. It is essential to regularly inspect the sensor site for any signs of irritation or infection that may arise.
For optimal performance, ensure your blood glucose monitoring sensor is calibrated correctly by entering fingerstick blood sugar values when prompted. Establish a routine of using a blood glucose monitoring sensor to monitor your blood sugar levels at critical times throughout the day—particularly before meals and during physical activity—to gain insights into how various foods and activities influence your blood sugar levels. Notably, the mean post-meal blood sugar (BG) time window is restricted to 60–120 minutes post-meals, highlighting the importance of timely monitoring.
Consistently reviewing the data generated by the blood glucose monitoring sensor is crucial, as it enables you to identify trends and adjust your management plan as needed. As B.K. notes, advancements in CGM technology, supported by grants from organizations like Lifescan, enhance the accuracy and reliability of these devices.
Recent advancements, such as the Continuous Glucose-EGA (CG-EGA), provide enhanced evaluation of CGM data using a blood glucose monitoring sensor, focusing on both point accuracy and the rate of blood sugar change. A case study on the CG-EGA illustrates how this tool improves understanding of CGM performance, particularly in critical blood glucose ranges, thereby aiding in making safer and more effective treatment decisions. At T 2 Solutions, we are committed to offering extensive resources and community support for individuals managing Type 2 and Type 3 blood sugar conditions.
By integrating practical advice with educational content, we aim to empower newly diagnosed patients to make informed decisions about their health and utilize the latest technology effectively.
Interpreting Blood Glucose Data
T2DSolutions is proud to introduce itself as a comprehensive resource hub for individuals managing Type 2 and Type 3 conditions. Our goal is to offer assistance and education to recently diagnosed individuals, aiding them in navigating the challenges of their condition. Interpreting data from a blood glucose monitoring sensor is essential for effective diabetes management, as it involves understanding the established ranges of normal sugar concentrations and recognizing deviations that may require intervention.
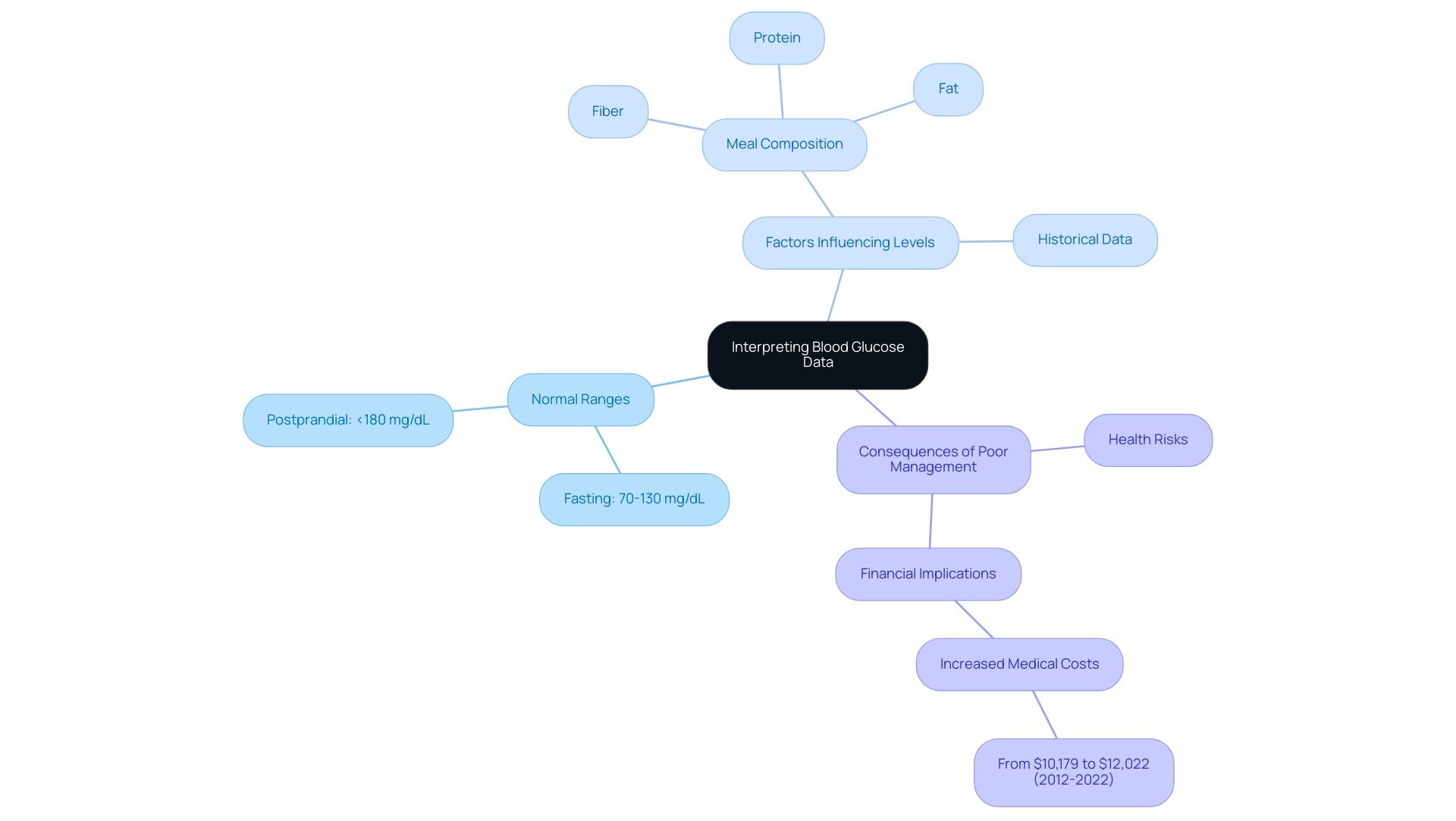
Fasting blood sugar levels are generally regarded as normal when they range between 70-130 mg/dL, while postprandial (after meal) levels must stay under 180 mg/dL. Readings that exceed these thresholds can signal the necessity for adjustments in dietary choices, exercise routines, or medication protocols. It is advantageous to use historical data gathered from blood glucose monitoring sensors to identify trends over time, such as spikes following specific meals or drops during periods of physical activity.
For instance, a case study titled 'Postprandial Sugar Response to Meals' analyzed interstitial concentrations after ingestion of different meals with identical carbohydrate amounts but varying fiber, protein, and fat content. The results indicated that meals with quicker absorption traits resulted in greater and shorter-lasting increases in sugar levels compared to those with slower absorption, emphasizing the influence of meal composition on sugar response. Additionally, with the rise in excess healthcare expenses linked to blood sugar issues from $10,179 to $12,022 between 2012 and 2022, the financial consequences of inadequate sugar control are substantial.
As Divya Gopisetty states, 'Comprehending your blood sugar information is essential not only for overseeing your health but also for avoiding the financial strains that can result from complications related to diabetes.' By understanding these fluctuations with the help of a blood glucose monitoring sensor, patients can work collaboratively with their healthcare teams to optimize treatment strategies and improve overall health outcomes. At T2DSolutions, we strive to enable patients with educational resources, community assistance, and tools like the blood glucose monitoring sensor for tracking blood sugar, ensuring that they possess the means essential for effective diabetes management.
Managing Alerts and Notifications
At a2d Solutions, we acknowledge the importance of Continuous Monitoring systems, which include a blood glucose monitoring sensor and are equipped with customizable alerts to notify users of high and low sugar concentrations. Tailoring these alerts based on individual health goals and the guidance of your healthcare provider is essential. For example, you may opt to receive notifications at 140 mg/dL for elevated sugar and at 70 mg/dL for low amounts.
Promptly responding to these alerts is crucial, as timely action can prevent serious health complications. As emphasized by the Juvenile Diabetes Research Foundation Continuous Monitoring Study Group, 'Hypoglycemia was the primary end point of one study in which patients had good glycemic control at baseline,' highlighting the significance of effective sugar management. We recommend creating a clear response strategy; for instance, consuming fast-acting carbohydrates for low readings or adjusting insulin dosages for high amounts.
Data indicates that the false alert rate can rise to 17.3% when alerts are set at 140 mg/dL, emphasizing the need for accuracy in monitoring. Furthermore, preliminary analyses suggest that the blood glucose monitoring sensor, specifically continuous glucose monitoring (CGM), may be cost-effective for Type 1 Diabetes Mellitus (T1DM) patients, making it a viable option for newly diagnosed individuals. Recent news also indicates that the use of blood glucose monitoring sensors in real-time CGM can reduce HbA1c values in adult patients with T1DM and type 2 mellitus, emphasizing the advantages of these systems.
By consistently observing these alerts, individuals can greatly enhance their capacity to uphold stable blood sugar levels and take a proactive stance on health oversight. T2DSolutions aims to support you on this journey by providing essential resources, including educational materials, community support, and access to healthcare professionals for effective diabetes management.
Maintaining Your Blood Glucose Monitoring Sensor
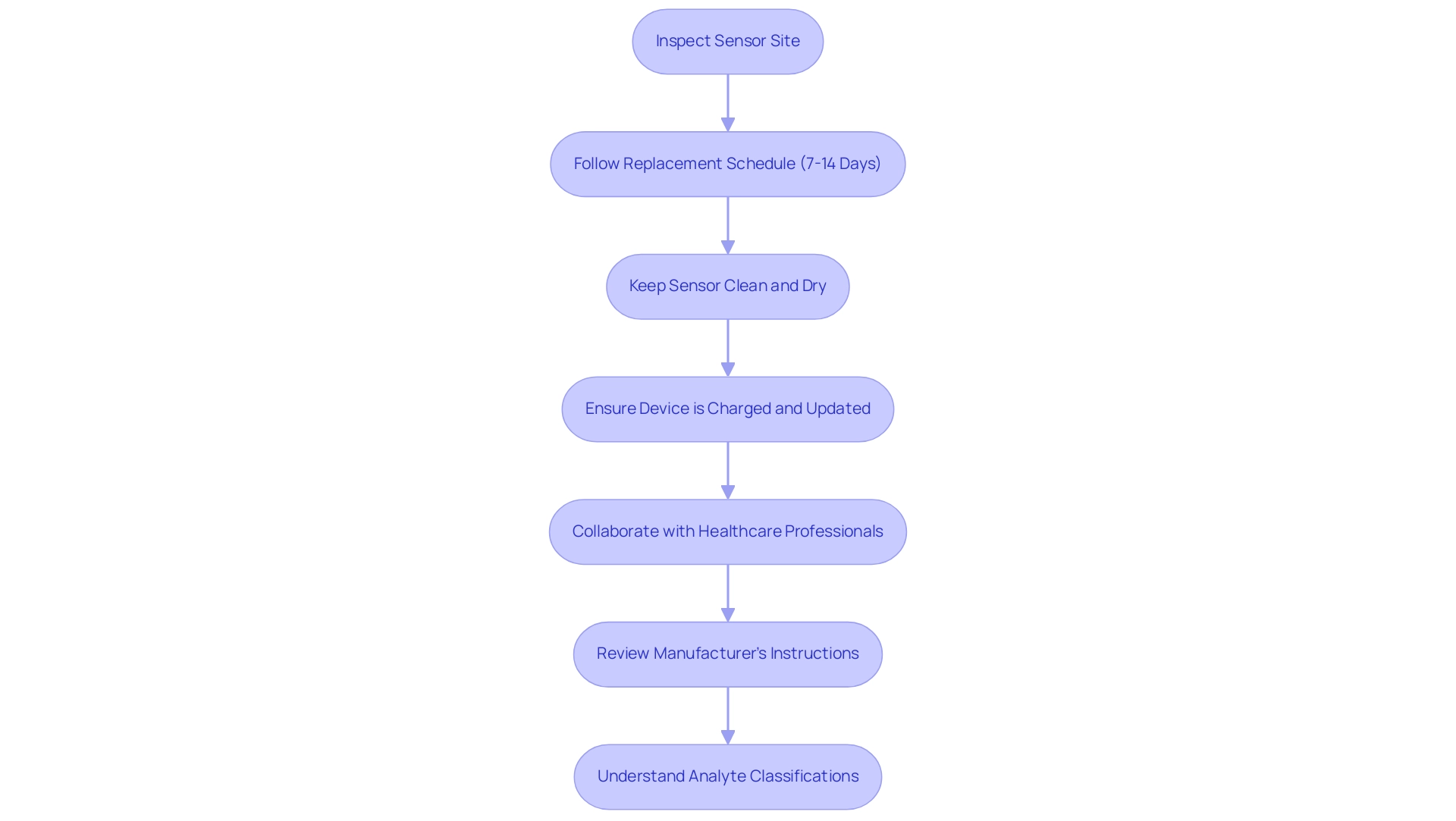
Maintaining your blood glucose monitoring sensor is crucial for ensuring reliable performance and accurate readings. Regularly inspect the blood glucose monitoring sensor site for any signs of irritation or infection, and follow the manufacturer's advice for replacing the blood glucose monitoring sensor, which usually takes place every 7 to 14 days for continuous monitoring (CGM) sensors. To maintain the functionality of the blood glucose monitoring sensor, it is essential to keep it clean and free from moisture and debris.
Furthermore, ensure that the device transmitting the data—such as a smartphone or receiver—is fully charged and equipped with the latest software updates. As emphasized by Mathew TK, implementing a systematic process to manage altered blood sugar readings requires input and active collaboration with the client as a consumer, endocrinologists, diabetes nurse educators, pharmacists, clinical nurse specialists, dieticians, and data analysts. This collaborative method emphasizes the significance of routinely examining the manufacturer's instructions for care and maintenance to enhance the functionality of your blood glucose monitoring sensor.
Furthermore, grasping the classification of analytes—such as description, use and rationale, preanalytical considerations, analytical methods, and interpretation—can improve your control of blood sugar levels. A relevant case study, titled 'Handling Out-of-Range Specimens,' illustrates that specimens with HbA results outside the reference interval should be verified through repeat testing to rule out potential complications. By adhering to these practices, not only can you guarantee precise readings from the blood glucose monitoring sensor, but you also prolong the lifespan of the blood glucose monitoring sensor, which can retain up to 90 days of data.
T2 Solutions will provide resources and community support to help newly diagnosed patients navigate these practices effectively, ensuring they have the tools and guidance needed for optimal glucose management.
Conclusion
The advancements in blood glucose monitoring technologies are revolutionizing diabetes management, empowering patients to take control of their health. Continuous Glucose Monitoring (CGM) systems stand out for their ability to provide real-time data, allowing individuals to make informed decisions regarding their diet, exercise, and medication. As diabetes diagnoses, particularly in younger populations, continue to rise, the importance of these technologies cannot be overstated.
Understanding the different types of monitoring methods—both invasive and non-invasive—enables patients to choose the most suitable option for their lifestyle. While invasive methods like CGMs offer high accuracy, non-invasive technologies are emerging as promising alternatives that reduce discomfort. This variety ensures that patients can find tools that align with their personal health management goals.
Utilizing these technologies effectively requires not only proper usage and maintenance but also a keen understanding of the data they produce. By interpreting blood glucose readings and responding to alerts, patients can prevent complications and improve their overall health outcomes. The collaborative approach advocated by T2DSolutions emphasizes the need for a supportive network, equipping individuals with the education and resources necessary to navigate their diabetes management journey successfully.
In conclusion, as diabetes management continues to evolve, embracing these innovative monitoring technologies is essential. By leveraging accurate data and community support, individuals can take proactive steps towards better health, ultimately enhancing their quality of life.
Frequently Asked Questions
Why are blood glucose monitoring sensors important for individuals managing diabetes?
Blood glucose monitoring sensors provide real-time information that helps patients and caregivers make informed decisions regarding diet, exercise, and medication, which is crucial for effective diabetes management.
How many Americans currently benefit from Continuous Glucose Monitoring (CGM) systems?
Over 10 million Americans rely on insulin and benefit from Continuous Glucose Monitoring (CGM) systems.
What recent statistics highlight the need for diabetes management technologies?
Recently, 5,293 children and adolescents aged 10 to 19 years were diagnosed with type 2 diabetes, emphasizing the urgent need for effective diabetes management technologies.
How do advanced blood glucose monitoring sensors help users?
These sensors alert users to fluctuations in sugar levels, which is essential for preventing hyperglycemia (high blood sugar) and hypoglycemia (low blood sugar).
What are some examples of advancements in blood glucose monitoring sensor technology?
Afon's development of a blood glucose monitoring sensor, supported by the National Institutes of Health and the University of Kentucky’s Igniting Research Collaboration Pilot Program, exemplifies ongoing advancements in this field.
What types of blood glucose monitoring methods exist?
Blood glucose monitoring methods can be classified into two main categories: invasive methods (like traditional fingerstick testing and CGM systems) and non-invasive methods (like optical sensors and bio-impedance devices).
What is the difference between invasive and non-invasive blood glucose monitoring methods?
Invasive methods involve skin penetration to obtain blood samples for testing, while non-invasive methods aim to assess sugar concentrations without skin penetration, offering convenience and reduced discomfort.
What is the typical error range for Continuous Glucose Monitoring (CGM) models?
The typical error for CGM models is stated at ±5% to ±10%, indicating their precision in monitoring blood sugar levels.
What emerging technologies are being developed for non-invasive blood glucose monitoring?
Technologies such as optical sensors, bio-impedance devices, and Bluetooth Low Energy (BLE) signal detection are being developed to enhance the accuracy and reliability of non-invasive glucose monitoring.
How can T2D Solutions assist newly diagnosed patients?
T2D Solutions offers extensive resources and community support for Type 2 and Type 3 blood sugar control, including educational materials, support groups, and access to the latest technology, helping patients manage their condition effectively.



