Overview:
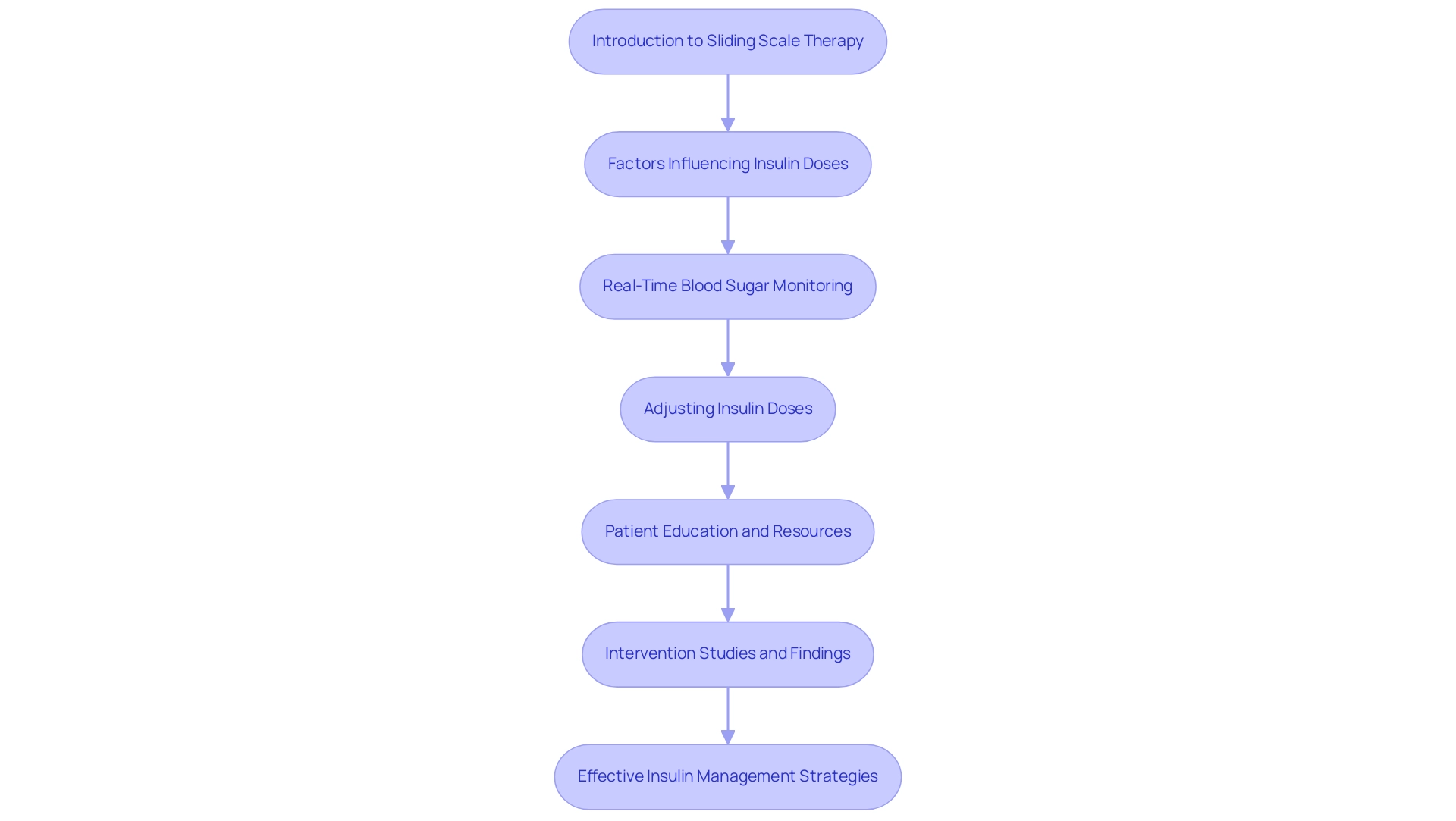
The main focus of the article is to provide an in-depth understanding of lispro sliding scale therapy for insulin management, emphasizing its importance for effective blood sugar control in patients. The article supports this by detailing how individualized dosing based on real-time blood glucose readings, along with education and collaboration with healthcare providers, enhances diabetes management and improves patient outcomes.
Introduction
In the realm of diabetes management, sliding scale therapy has emerged as a vital strategy for optimizing insulin administration based on real-time blood glucose levels. This approach not only accommodates the daily fluctuations experienced by patients but also emphasizes the importance of individualized care tailored to each person's unique health profile.
As research continues to underscore the significance of effective insulin management, understanding the principles and practices surrounding sliding scale therapy becomes essential for both patients and healthcare providers. This article delves into the intricacies of sliding scale therapy, offering insights into its implementation, the role of insulin lispro, best practices for blood glucose monitoring, and strategies for recognizing and managing hypoglycemia.
By fostering collaboration between patients and healthcare professionals, the pathway to effective diabetes management is illuminated, ensuring that individuals are equipped with the knowledge and tools necessary to navigate their condition confidently.
Introduction to Sliding Scale Therapy for Insulin Management
The lispro sliding scale therapy signifies a dynamic method of hormone administration, enabling the modification of doses based on real-time blood sugar levels. This approach is especially advantageous for individuals who manage their fluctuating glucose levels during the day with a lispro sliding scale. By utilizing a lispro sliding scale that aligns specific blood sugar readings with corresponding insulin doses, individuals can improve their management of the condition.
This individualized approach recognizes the necessity to consider various factors, including diet, physical activity, and overall health status. T2DSolutions provides resources that enable individuals to comprehend and apply sliding scale therapy effectively, ensuring they possess the tools required for successful management of their condition. Notably, by the end of 2018, there were ten intervention studies focused on blood sugar management in long-term care facilities, emphasizing the growing body of research supporting lispro sliding scale therapy.
Moreover, recent intervention studies in diabetes care have emphasized that elevated admission blood sugar (BG) levels are associated with greater chances of inadequate glycemic control, highlighting the significance of efficient management in this group. As noted by Dr. Guillermo E. Umpierrez, a leading expert in the field,
- "We propose that an individualized approach to inpatient glycemic management is imperative, and cautious use of SSI may be a viable option for certain patients with mild hyperglycemia and admission BG <180 mg/dL."
T2DSolutions also offers educational resources that clarify how to interpret blood glucose levels and modify medication doses accordingly.
Furthermore, a study named 'Characteristics of Patients Who Remained on Continuous SSI by Admission Blood Glucose Concentration' showed that individuals with lower admission BG levels were generally older and had lower HbA1c levels, further suggesting the necessity for customized treatment plans. Lastly, the pilot inpatient management program for blood sugar implemented by Ketz JM et al., published in Clinical Diabetes, highlights recent advancements in glycemic control, reinforcing the relevance of the lispro sliding scale therapy. Comprehending lispro sliding scale therapy is essential for both individuals and healthcare providers, as it establishes the foundation for effective insulin management strategies in managing blood sugar.
T2DSolutions is dedicated to assisting patients through education and community involvement, ensuring they are well-prepared to manage their condition effectively.
Utilizing Insulin Lispro in Sliding Scale Therapy: Dosage and Guidelines
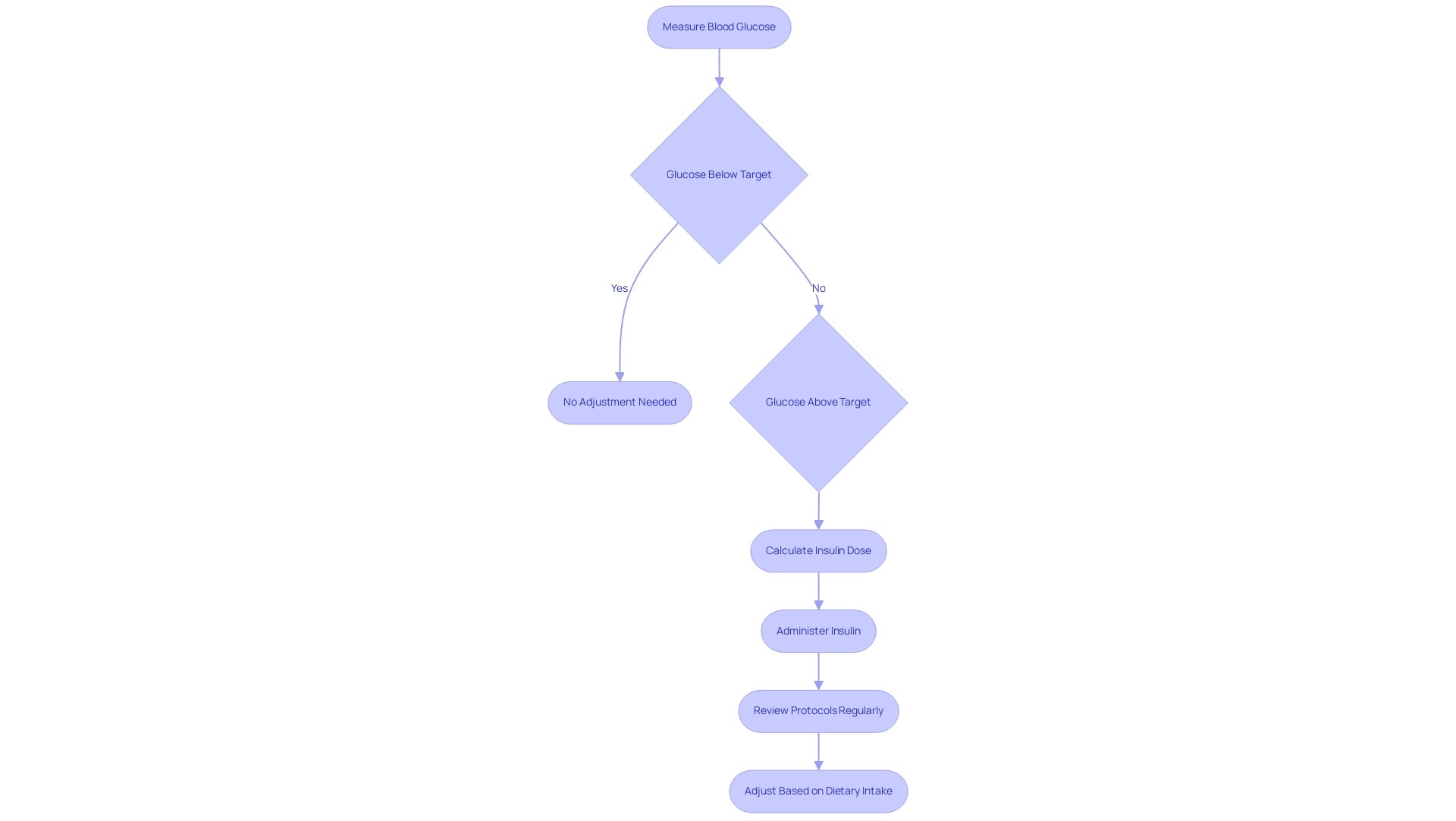
Insulin lispro is recognized for its rapid action, making it a preferred choice in diabetes management using a lispro sliding scale. This hormone formulation is marked by a rapid onset and a brief duration of effect, enabling accurate modifications based on current blood sugar levels. Standard practices typically involve measuring blood glucose before meals, with guidelines suggesting the use of a lispro sliding scale that prescribes 1 unit of lispro for every 50 mg/dL above a designated target level.
Significantly, individuals with preexisting diabetes may gain advantages from receiving 40% of their total daily dose (TDD) as basal medication subcutaneously, which supports effective management strategies. However, these guidelines must be tailored to the individual, taking into account daily variations in caloric intake and personal glucose sensitivity. It is crucial that patients are informed on how to identify their blood sugar patterns and the suitable timing for hormone administration.
Furthermore, healthcare providers should conduct regular reviews of lispro sliding scale protocols to accommodate daily adjustments in hormone doses, ensuring optimal glycemic control. For example, the case study titled 'Adjustment of Hormone Doses' emphasizes how hormone doses may need to be modified daily based on blood sugar testing outcomes and caloric consumption, reinforcing the significance of individualized care. According to D'Souza S., advancements in therapies involving rapid-acting formulations like lispro underscore the importance of personalized care in diabetes management.
These advancements illustrate that regular modifications based on blood sugar testing can significantly improve the efficacy of hormone therapy, as fasting sugar levels act as a vital indicator of basal hormone adequacy. Additionally, it is imperative for patients using pump devices to understand that malfunctions can lead to serious complications, including hyperglycemia and ketoacidosis, necessitating rapid management and alternative administration training.
Monitoring Blood Glucose Levels: Best Practices
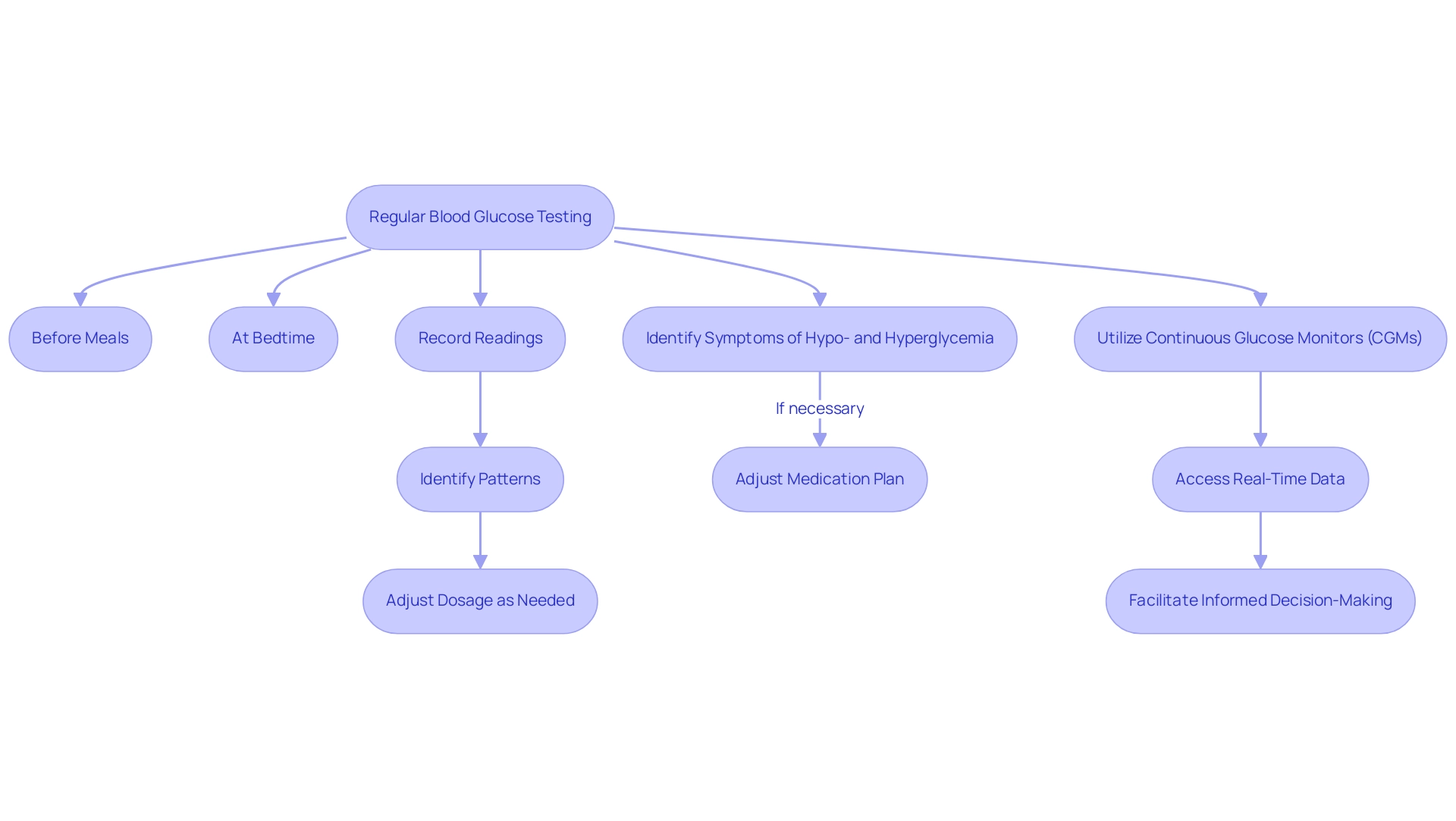
Effective blood glucose monitoring is essential for the successful implementation of lispro sliding scale therapy. Patients are advised to regularly test their blood sugar levels, particularly before meals and at bedtime. Maintaining a thorough record of these readings is essential, as it aids in recognizing patterns that can guide necessary modifications to dosage.
Identifying the symptoms of hypo- and hyperglycemia is equally crucial, as these conditions may require prompt adjustments to the medication plan. Continuous glucose monitors (CGMs) offer a valuable tool in this regard, providing real-time data that enhances the ability to manage glucose levels effectively. This technology not only simplifies the monitoring process but also facilitates informed decision-making by both patients and their healthcare teams regarding insulin administration.
Recent developments in CGM technology have further improved its utility, making it an indispensable resource in diabetes management. As highlighted in the AGP Report, blood sugar monitoring (BGM) serves as a critical component for healthcare providers to review readings and optimize treatment strategies, ultimately aiming to maintain levels within the target range. Clinicians should be aware that a clinically correct treatment decision could be made if the rate of change in blood sugar levels is falling ≥4 mg/dL/min.
Furthermore, as noted by Lanning Tanenbaum Wong Hood KK, barriers to continuous sugar monitoring persist, and addressing these barriers is crucial for effective diabetes management. The visualization of CGM data, as demonstrated in case studies, illustrates how various graphical representations can enhance understanding of glucose fluctuations and support clinical decision-making.
Recognizing and Managing Hypoglycemia
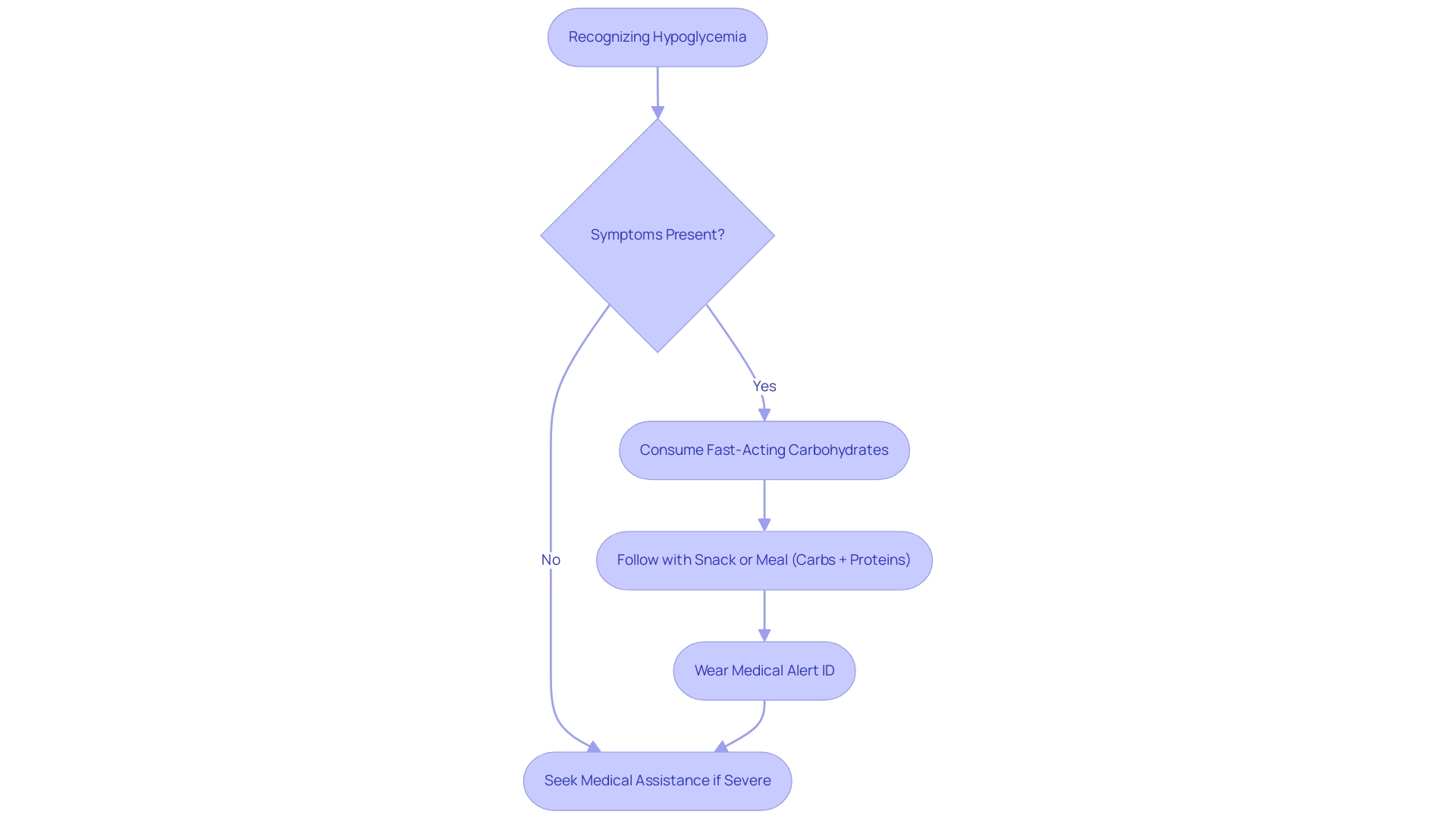
At T2DSolutions, we acknowledge that hypoglycemia, or low blood sugar, presents a significant risk for individuals utilizing the lispro sliding scale therapy. It is imperative for individuals recently diagnosed to identify early symptoms, which may manifest as:
- Shakiness
- Sweating
- Confusion
- Irritability
In instances where hypoglycemia is suspected, immediate action is crucial; individuals should consume fast-acting carbohydrates, such as glucose tablets or fruit juice, to swiftly elevate their blood glucose levels.
Following this initial intervention, it is advisable to have a subsequent snack or meal containing both carbohydrates and proteins to stabilize blood sugar levels effectively. Furthermore, education on the critical nature of wearing medical alert identification can prove beneficial. This guarantees that in the event of severe hypoglycemia—especially when individuals may be unable to communicate their condition—they receive appropriate and timely medical assistance.
Notably, the NICE-SUGAR trial showed a concerning incidence of hypoglycemia in intensive treatment settings, with rates reported at 6.8% compared to just 0.5% in less intensive approaches. This statistic highlights the necessity for individuals to be well-informed and prepared to effectively manage low blood sugar by utilizing the lispro sliding scale. As highlighted in recent guidelines, clinical judgment plays a pivotal role in achieving glycemic goals, particularly for those with mild hyperglycemia.
Additionally, a case study by Gunst et al. demonstrated no difference in mortality related to hypoglycemia management in an ICU setting, further emphasizing the importance of tailored approaches in treatment. At T2DSolutions, we strive to provide individuals with the information and techniques they require to effectively control their blood sugar levels and navigate their health journey.
We are dedicated to offering educational materials and community assistance to guarantee that those recently diagnosed have access to the tools essential for effective management of their condition.
Collaborating with Healthcare Providers: A Team Approach
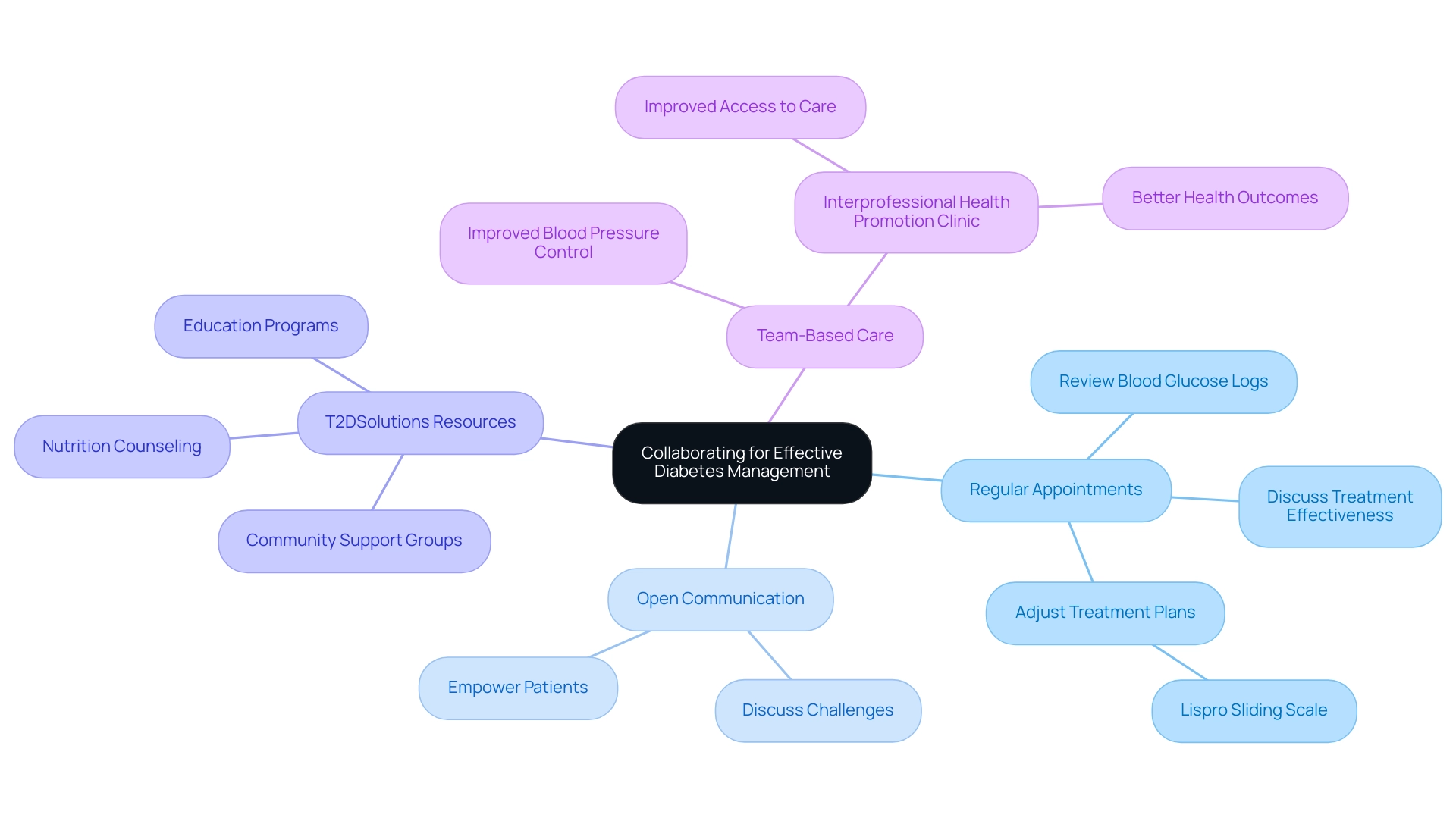
Launching T2DSolutions as a new resource hub for Type 2 and Type 3 blood sugar management is crucial for newly diagnosed patients. Effective diabetes management necessitates viewing healthcare providers as essential partners in the treatment process. Regular appointments play a pivotal role, facilitating the review of blood glucose logs and discussions regarding the effectiveness of treatment plans involving the lispro sliding scale, which may lead to necessary adjustments.
Open communication is a cornerstone of this relationship; individuals should feel empowered to discuss any challenges they encounter with their insulin regimen or necessary lifestyle changes. T2DSolutions aims to provide valuable resources, including nutrition counseling, education programs, and access to community support groups, to enhance this collaborative approach. This partnership not only tailors treatment plans to meet individual needs but also fosters improved health outcomes.
Alberta Becenti, MPH, emphasizes the importance of such collaboration, stating,
The available evidence shows that for individuals with blood sugar issues, TBC enhances their blood glucose, BP, and lipid levels.
Furthermore, a systematic review from the Community Guide indicates that team-based care notably improves blood pressure control, reinforcing the argument for collaboration in managing diabetes-related conditions. The innovative model of the Interprofessional Health Promotion Clinic exemplifies this collaborative approach, showcasing improved access to care for individuals and potentially better health outcomes for those involved.
Additionally, there is a growing need for further research to define guidelines on which patient-reported outcome measures should be adopted in the management of diabetes-related conditions. By prioritizing communication with healthcare teams, T2DSolutions empowers patients to enhance their quality of life and effectively navigate the complexities of diabetes management. We encourage you to subscribe for updates and explore the resources available on T2DSolutions once launched, ensuring you have the support you need.
Conclusion
Sliding scale therapy stands as a cornerstone in effective diabetes management, offering a personalized approach that adapts insulin administration to real-time blood glucose levels. This method not only addresses daily fluctuations in glucose concentrations but also emphasizes the importance of individualized care, taking into account factors such as diet, physical activity, and overall health status. The insights provided throughout this article highlight the significance of understanding and implementing sliding scale therapy, particularly in conjunction with rapid-acting insulins like insulin lispro.
Key practices such as:
- Regular blood glucose monitoring
- Timely recognition of hypoglycemia
are essential for optimizing the effectiveness of this therapeutic approach. Continuous glucose monitors (CGMs) and educational resources play crucial roles in enabling patients and healthcare providers to make informed decisions regarding insulin adjustments, thereby enhancing glycemic control. Furthermore, fostering collaboration between patients and healthcare teams is vital for tailoring treatment plans and improving health outcomes.
In summary, sliding scale therapy represents a proactive strategy in diabetes management that empowers patients to take charge of their health. By embracing the principles outlined in this article, individuals can navigate their diabetes journey with confidence, ensuring they are well-equipped to manage their condition effectively. The commitment to education, community support, and open communication with healthcare providers will ultimately pave the way for improved diabetes care and better quality of life.



