Introduction
Managing diabetes effectively requires a nuanced understanding of various metrics, with A1C levels serving as a critical focal point. A1C, or glycated hemoglobin, provides valuable insights into average blood glucose levels over the past two to three months, making it indispensable for evaluating long-term glucose control.
As the prevalence of diabetes continues to rise, particularly type 2 diabetes, the need for effective monitoring and management strategies has never been more pressing. This article delves into the significance of A1C testing, its interpretation, the impact of lifestyle changes, and the importance of collaboration with healthcare teams.
By exploring these facets, individuals can better navigate their diabetes management journey and make informed decisions to improve their health outcomes.
Understanding A1C: The Key to Diabetes Management
A1C, or glycated hemoglobin, is an essential blood test that shows the A1C chart to blood glucose levels, indicating average blood sugar levels over the past 2 to 3 months. This measurement is expressed as a percentage on the A1C chart to blood glucose, where elevated values indicate suboptimal control of blood glucose. Type 2 accounts for 90–95% of all cases, highlighting the widespread need for effective monitoring.
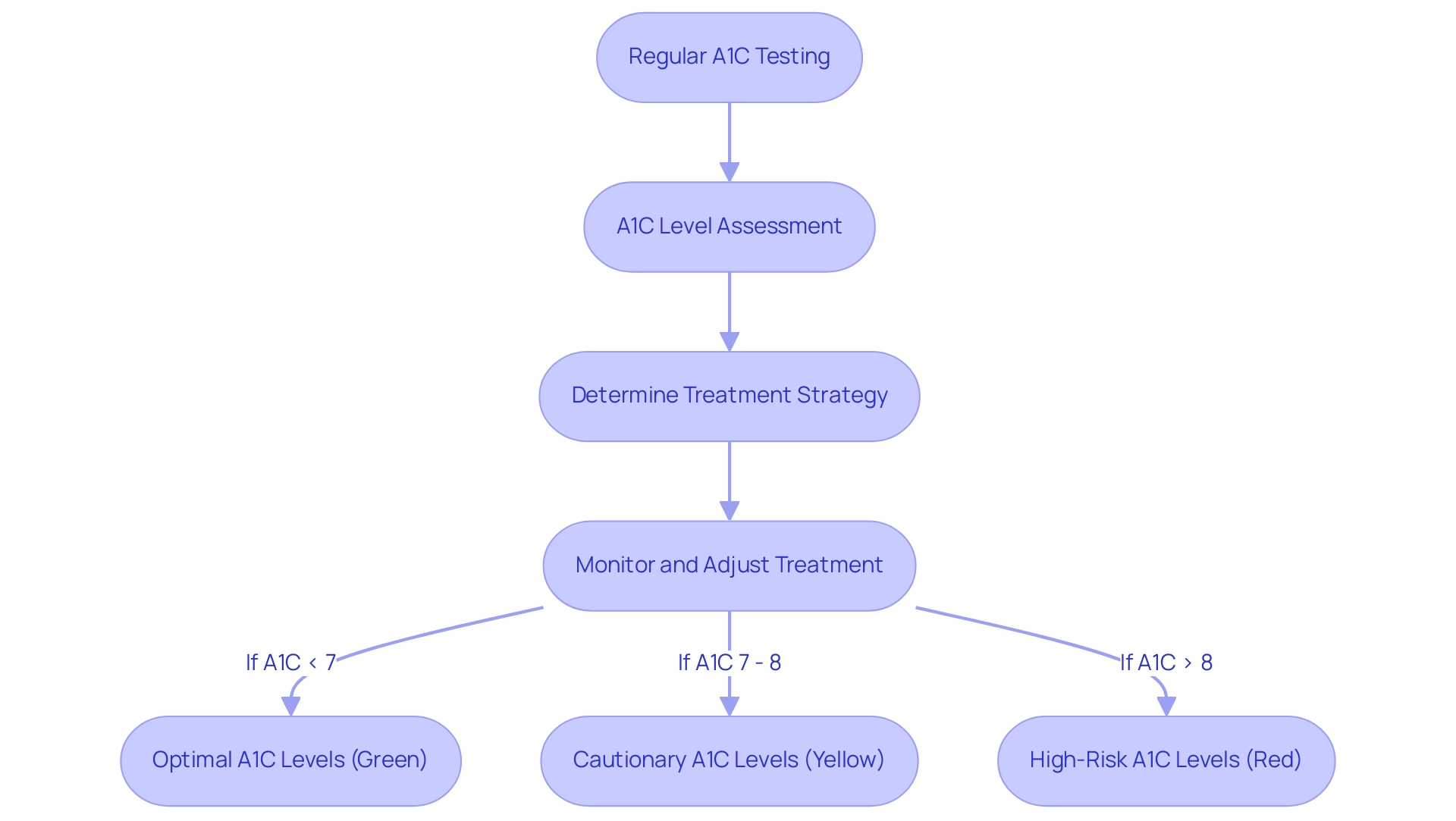
For the majority of adults managing this condition, an A1C level of less than 7% is generally recommended to mitigate the risk of complications related to it. Comprehending and tracking your A1C chart to blood glucose is crucial, as it enables the assessment of the effectiveness of your health control plan and allows for necessary modifications. Regular A1C testing is paramount; it empowers healthcare providers to assess long-term sugar control effectively using the A1C chart to blood glucose and determine if treatment strategies require modification.
T2DSolutions is here to assist recently diagnosed individuals by offering extensive resources, such as educational materials and community forums, customized to your health journey. Additionally, T2DSolutions offers tools and guides to help patients monitor and understand their A1C levels, which includes access to the A1C chart to blood glucose for necessary information and support. Moreover, distinct diagnostic standards will recognize diverse levels of maternal hyperglycemia and maternal/fetal risk, which highlights the significance of using the A1C chart to blood glucose in evaluating sugar levels and management approaches, especially for individuals with a background of gestational hyperglycemia.
Regular testing for prediabetes or blood sugar issues is recommended at least every three years for such individuals. Furthermore, sugar testing, while advantageous due to its low cost and wide availability, has disadvantages such as high diurnal variation and potential inaccuracies due to factors like recent physical activity or improper sample handling. These factors can result in inaccurately low or high sugar levels, affecting the trustworthiness of blood sugar diagnosis and, as a result, the accuracy of the A1C chart to blood glucose.
Notably, in 2024, the age-adjusted prevalence of diagnosed conditions has significantly increased, underscoring the importance of vigilant monitoring and management using the A1C chart to blood glucose levels.
Interpreting the A1C Chart: What Your Results Mean for Blood Glucose Control
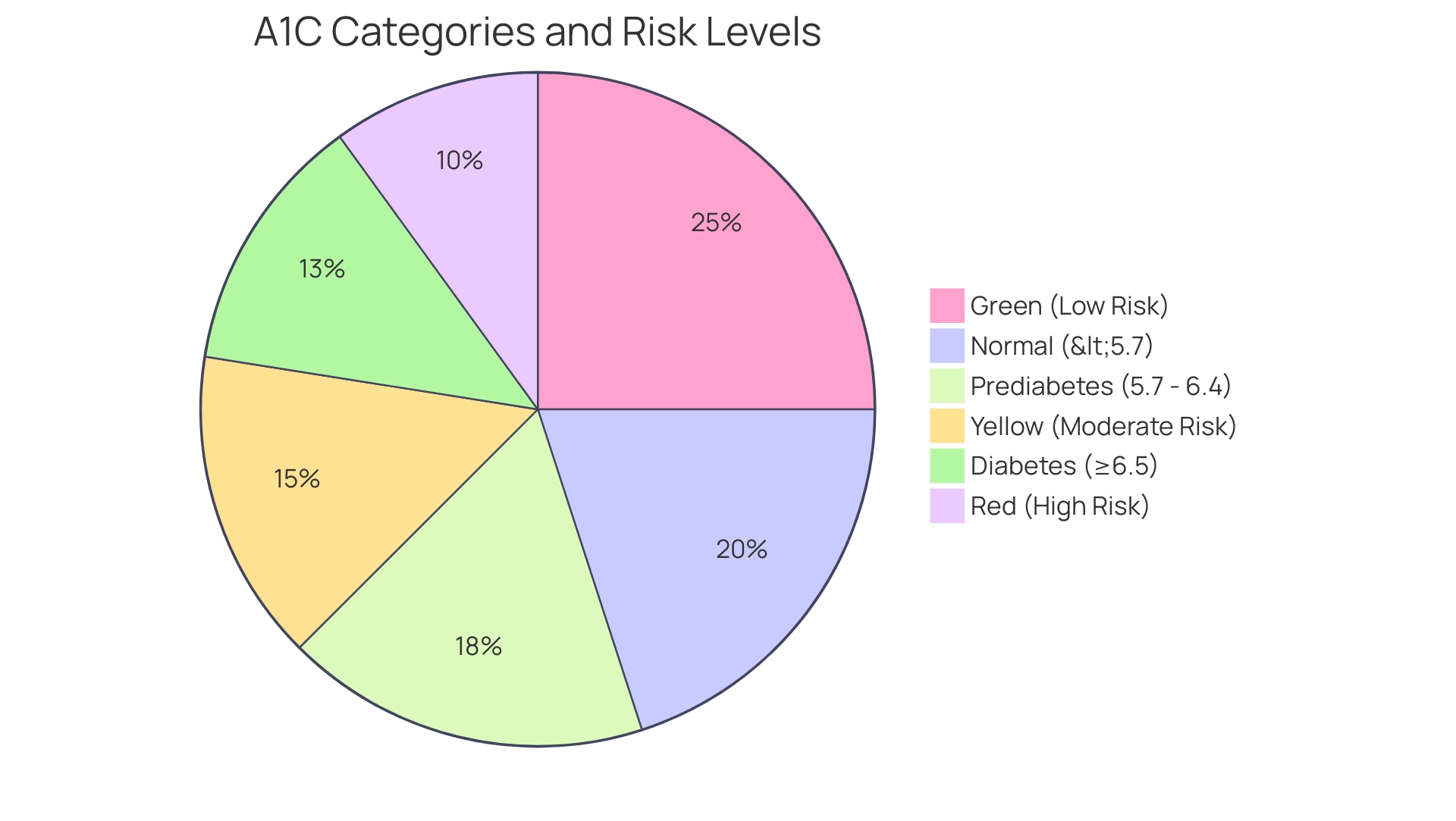
The A1C chart categorizes results into separate ranges, each indicating different levels of blood sugar control. Specifically, an A1C level below 5.7% is categorized as normal, while values between 5.7% and 6.4% indicate prediabetes. A diagnosis of diabetes is confirmed with an A1C of 6.5% or higher.
Understanding these categories is crucial when interpreting your A1C results; it is essential to correlate the A1C chart to blood glucose for a comprehensive view of your glycemic control. For instance, an A1C of 7% generally relates to an average blood sugar level of roughly 154 mg/dL. Regular monitoring of both the A1C chart to blood glucose and daily glucose levels facilitates informed adjustments to your diet and exercise regimen.
This collaborative approach with your healthcare team is vital in achieving optimal management of blood sugar. Notably, the importance of considering time in range, as highlighted in the case study 'The Fallacy of Average in Glycemic Control,' underscores that relying solely on the A1C chart to blood glucose can be misleading, emphasizing the need for a multifaceted approach to managing blood sugar. Additionally, the traffic light chart categorizes risk levels:
- Green indicates low risk with no action required
- Yellow indicates moderate risk requiring consultation with a healthcare professional
- Red indicates high risk also requiring consultation
Furthermore, current research shows that time in range is associated with less hypoglycemia fear and higher technology acceptance in adults with well-controlled Type 1. As Sandeep Sharma states, 'Comprehending the subtleties of A1C and blood glucose levels is crucial for effective control of the condition.' This emphasizes the essential aspect of incorporating different metrics for a thorough health control strategy.
As T2DSolutions launches, it will offer educational resources and community support to assist newly diagnosed patients in navigating these complexities, ensuring they have access to the tools and information required for effective health oversight.
The Role of Lifestyle Changes in Managing A1C Levels
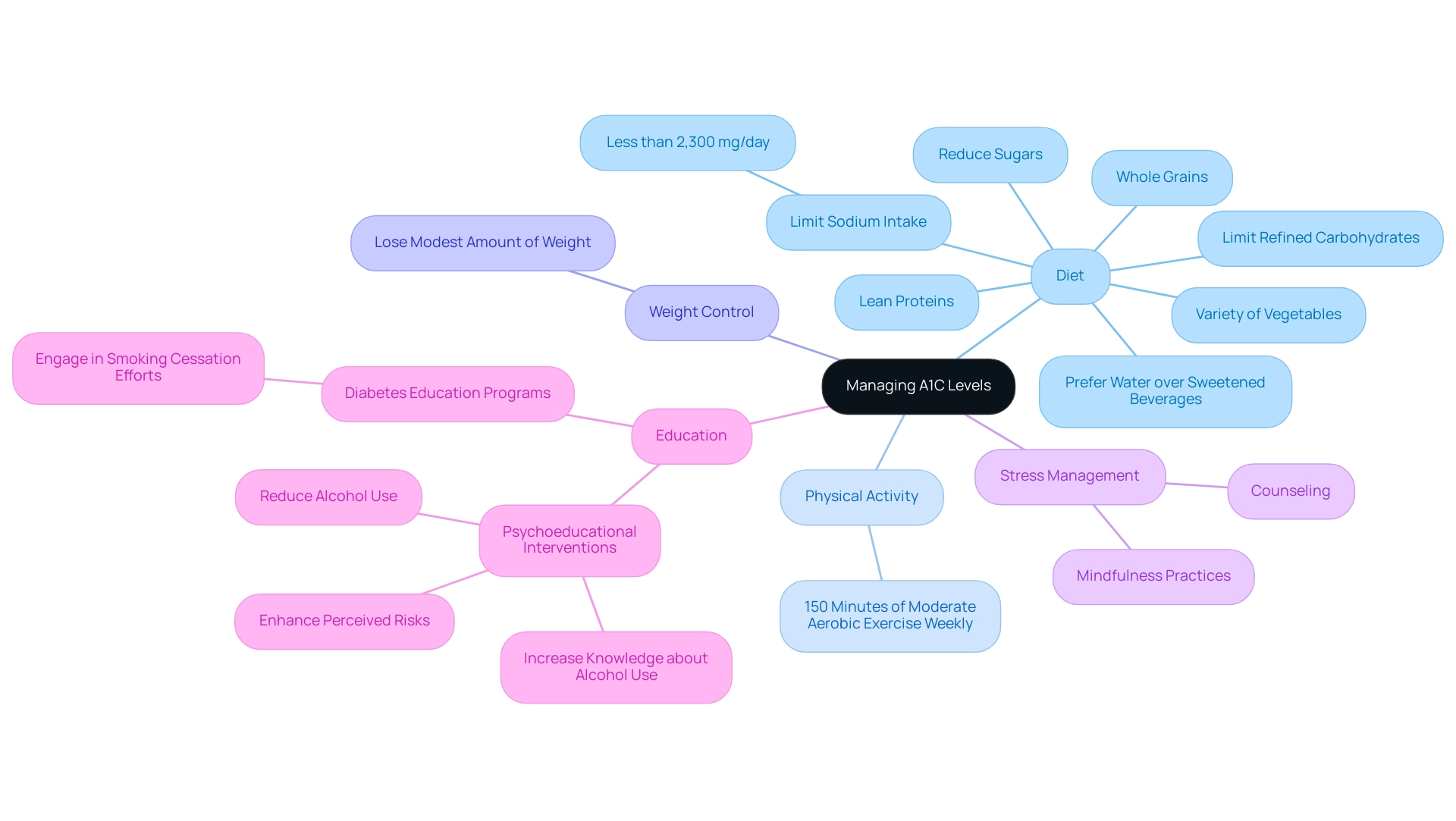
Managing A1C levels effectively hinges on strategic lifestyle modifications, a journey that T2DSolutions supports through comprehensive resources and community engagement. A balanced diet is essential, emphasizing whole grains, a variety of vegetables, and lean proteins, while also reducing the intake of sugars and refined carbohydrates. Recent statistics reveal a significant decreasing trend in the occurrence of the condition after 2008, with an incidence of 8.4 per 1,000 adults, underscoring the importance of lifestyle changes in handling the illness.
Consistent physical activity is a fundamental aspect of effective diabetes oversight; the American Diabetes Association suggests striving for a minimum of 150 minutes of moderate aerobic exercise weekly, which can result in considerable enhancements in blood sugar control. Furthermore, weight control is critical—losing even a modest amount of weight can result in meaningful reductions in A1C levels. Stress management techniques, such as mindfulness practices or counseling, can also play a vital role in influencing blood glucose levels.
Educational interventions are essential; as noted, 'there is growing evidence for psychoeducational interventions that may increase knowledge about alcohol use and related health issues, may enhance perceived risks, and may reduce alcohol use among young individuals with type 1 condition.' Additionally, individuals with high blood sugar should limit sodium intake to less than 2,300 mg/day and prefer water over sweetened beverages, as recommended in recent case studies. The importance of these lifestyle changes is further highlighted by studies showing that education programs not only enhance knowledge but also encourage healthier decision-making among patients.
By committing to these lifestyle adjustments, individuals can achieve substantial improvements in their A1C results and overall health outcomes, which can be tracked using the A1C chart to blood glucose, supported by the resources and community at T2 Solutions. Stay tuned for our upcoming resources as T2 Solutions is committed to providing comprehensive support and education for managing Type 2 and Type 3 Diabetes.
Regular Monitoring: How Often Should You Check Your A1C?
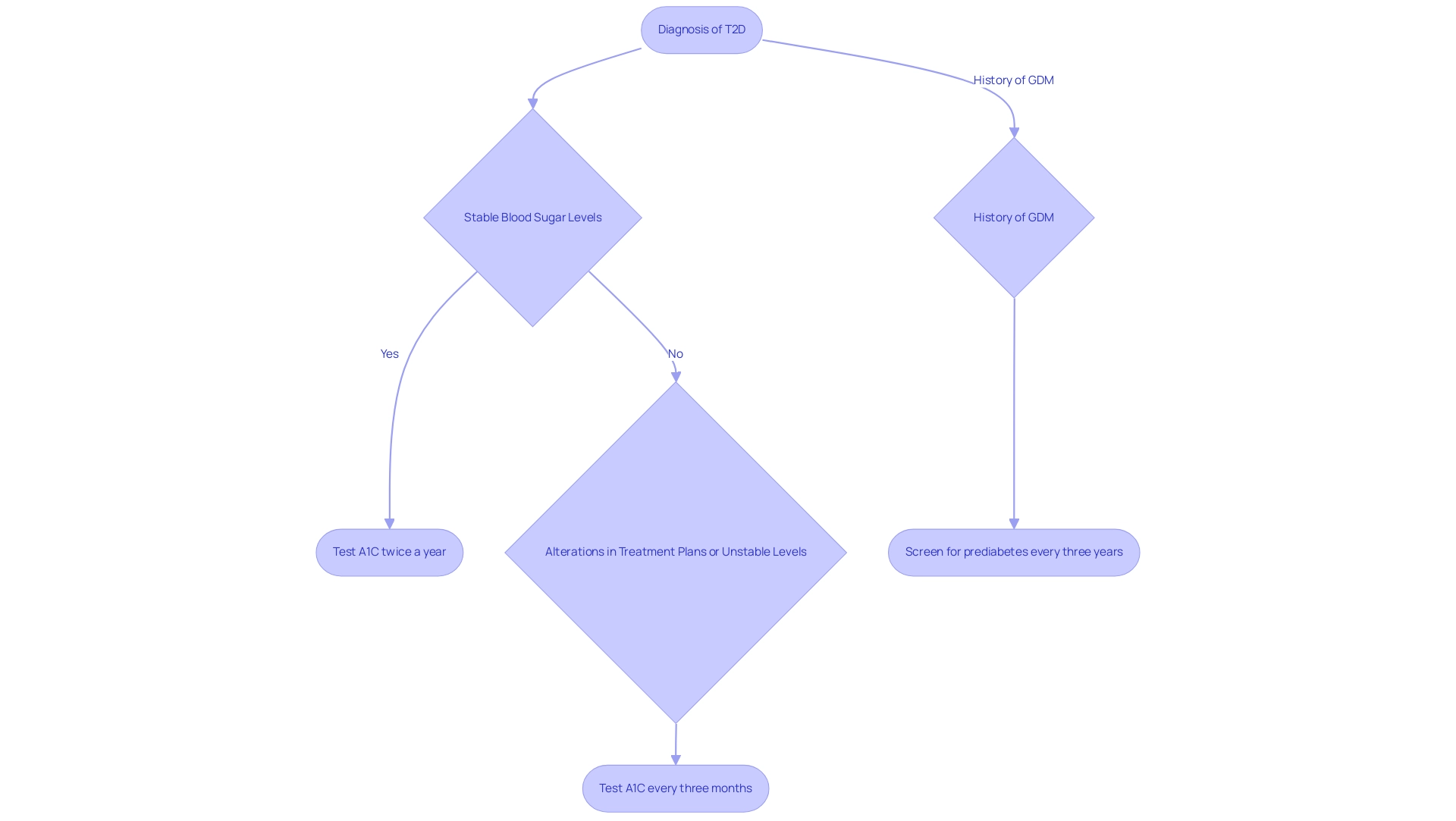
As part of T2D Solutions, a new resource hub dedicated to education and support for managing blood sugar levels, understanding the recommended frequency of A1C testing is vital for newly diagnosed patients. The frequency of A1C testing varies based on individual circumstances and treatment goals. According to the latest guidelines from the American Diabetes Association Professional Practice Committee, individuals with the condition should undergo A1C testing at least twice a year if they consistently meet treatment targets and maintain stable blood sugar levels.
Conversely, if there are alterations in treatment plans or if blood sugar levels fail to meet established goals, testing is advised every three months. This ongoing oversight is essential, as it allows healthcare providers and patients to assess the effectiveness of the condition control strategy, resulting in prompt actions for enhancing blood glucose regulation. Moreover, individuals with a history of gestational diabetes mellitus (GDM) should undergo lifelong screening for prediabetes or elevated blood sugar levels at least every three years, as recommended by the American Diabetes Association.
Moreover, data indicate important consequences for the treatment of blood sugar conditions; in a study of 1,150 dental patients over 40 years old in India, roughly 20.7% were diagnosed with prediabetes, and 14.6% fulfilled the criteria for elevated blood sugar. Such statistics underscore the importance of using an A1C chart to blood glucose as a preventive measure. Furthermore, it is essential to consider that data are lacking on the effects of treating maternal hyperglycemia during pregnancy on offspring's risk for obesity and metabolic disorders, indicating a need for further clinical studies.
Consistent compliance with these testing guidelines is crucial for optimal care, ensuring that individuals receive the necessary evaluations and modifications to their treatment plans. T2D Solutions will provide additional resources and support to help you understand and manage your condition effectively.
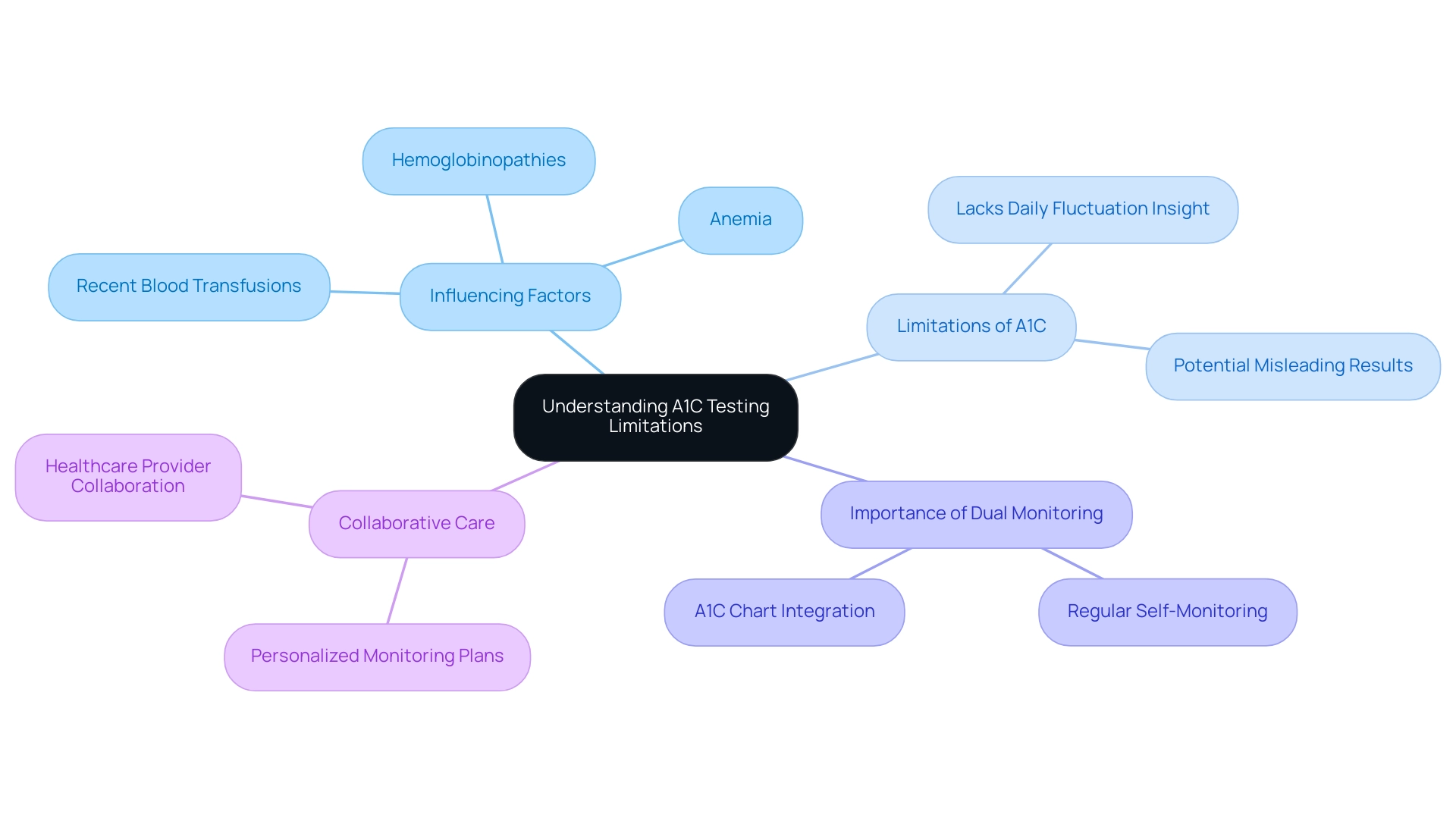
Understanding the Limitations of A1C Testing
At T2DSolutions, we recognize that the A1C chart to blood glucose testing remains a cornerstone in diabetes management, but it is crucial for patients to understand its limitations. The HbA1c percentage, which indicates the average sugar level in a patient's body over the past 90 days, is essential for generating an A1C chart to blood glucose. However, A1C results can be influenced by factors such as:
- Anemia
- Hemoglobinopathies
- Recent blood transfusions
These factors may affect the accuracy of the A1C chart to blood glucose readings, potentially leading to misleading results.
Moreover, the A1C test, which is represented in the A1C chart to blood glucose, does not provide insights into daily sugar fluctuations or acute glycemic events. Research by Balintescu A. emphasizes the importance of recognizing these nuances in the context of managing blood sugar levels. To achieve comprehensive diabetes control, patients should incorporate regular self-monitoring of blood sugar alongside using an A1C chart to blood glucose.
This dual approach allows for a more accurate assessment of their glycemic status. T2DSolutions will provide resources and assistance to help patients comprehend how to effectively monitor their blood sugar levels. Additionally, point-of-care (POC) A1C testing provides rapid results within 3–15 minutes and can be performed at the site of care, increasing accessibility for populations with limited healthcare access.
Collaborating closely with healthcare providers is essential in creating a personalized monitoring plan that integrates both daily glucose checks and the A1C chart to blood glucose measurements. Furthermore, it is important to note that metformin and glyburide should not be used as first-line agents for treating hyperglycemia in pregnancy, which adds another layer of consideration for patients managing their condition. T2DSolutions aims to be a comprehensive resource for patients navigating these complexities.
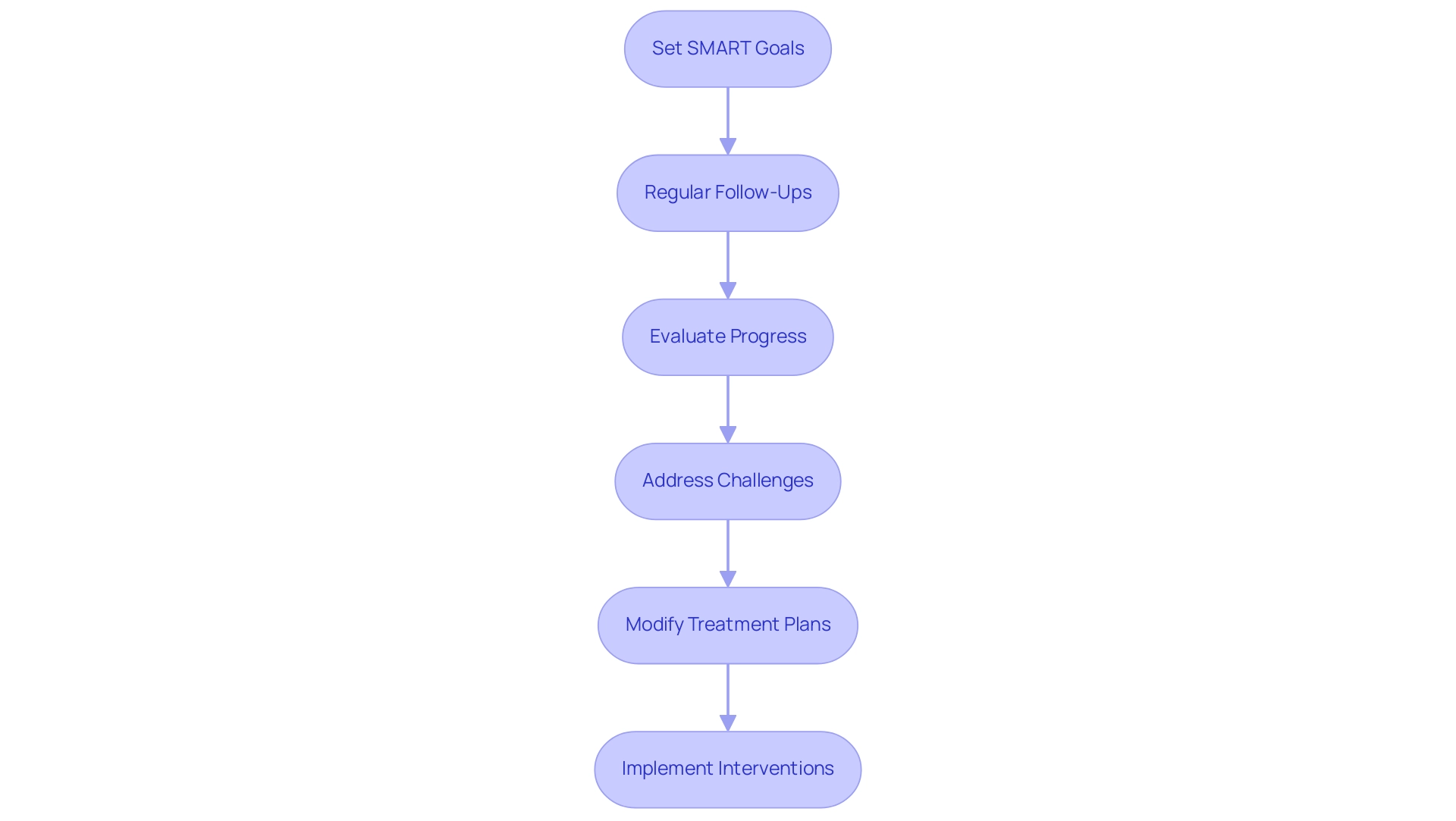
Collaborating with Your Healthcare Team: Setting Goals for A1C Management
Effective oversight of A1C levels relies on a strong partnership between patients and their healthcare teams, utilizing an A1C chart to blood glucose. Establishing specific, measurable, achievable, relevant, and time-bound (SMART) goals is a powerful strategy that can significantly boost motivation and accountability. For example, a patient might aim to reach a specific A1C target within six months or commit to a minimum of three physical activity sessions each week.
Regular follow-up appointments serve as critical touchpoints to evaluate progress, address any challenges, and modify treatment plans as needed. Evidence indicates that perceived provider optimism positively impacts patients' coping skills, with a significant coefficient of β = .48, highlighting the importance of a supportive healthcare team in promoting effective health care. By nurturing this cooperative atmosphere, patients and healthcare providers can create sustainable strategies that result in better control of blood sugar and improved health results.
Furthermore, interventions such as food prescription programs are considered promising to address food insecurity by integrating community resources directly into primary care settings, supporting patients in underserved areas. Insights from case studies, such as the effect of the patient-doctor relationship on pediatric care for the illness, further emphasize that a strong patient-provider relationship is crucial for effective handling of the condition, particularly for newly diagnosed individuals. As the landscape of diabetes care evolves, embracing these collaborative approaches will be essential for achieving optimal A1C management and utilizing an A1C chart to blood glucose for overall well-being.
Additionally, T2DSolutions is committed to supporting newly diagnosed patients by offering a comprehensive resource hub that includes educational materials, access to community support groups, and connections to healthcare professionals. This ensures that you have the tools and information needed on your journey to better health.
Conclusion
A1C testing plays a pivotal role in the effective management of diabetes, providing essential insights into long-term blood glucose levels. Understanding A1C metrics, including the implications of various results, is crucial for individuals navigating their diabetes management journey. Regular testing not only helps in monitoring progress but also facilitates timely adjustments to treatment plans, ensuring optimal glucose control and reducing the risk of complications.
Lifestyle modifications, such as maintaining a balanced diet and engaging in regular physical activity, are fundamental in achieving desirable A1C levels. The evidence underscores that even modest changes can yield significant improvements in health outcomes. Additionally, the importance of collaboration with healthcare teams cannot be overstated; a supportive relationship fosters accountability and encourages patients to set and achieve realistic health goals.
While A1C testing is invaluable, it is essential to recognize its limitations and complement it with daily glucose monitoring for a more comprehensive understanding of one’s glycemic status. As the prevalence of diabetes continues to rise, the integration of education, lifestyle changes, and healthcare collaboration becomes increasingly vital. By embracing these strategies, individuals can empower themselves to take control of their diabetes management and enhance their overall health and well-being.



