Overview
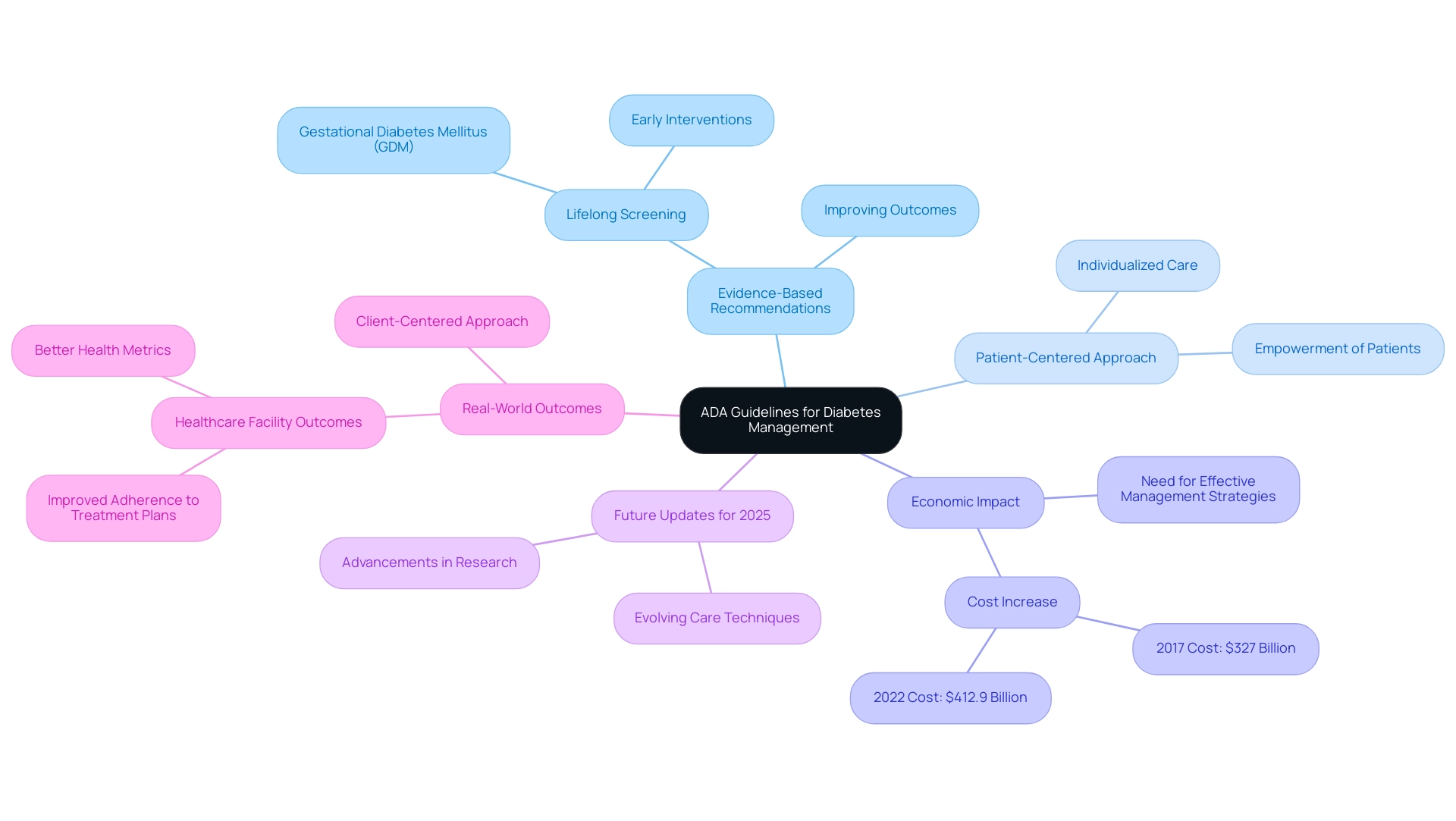
This article aims to help you understand the American Diabetes Association (ADA) guidelines for diabetes management. These guidelines play a crucial role in providing evidence-based recommendations designed to improve your health outcomes. It's important to recognize that a patient-centered approach is at the heart of these guidelines, ensuring that your needs and concerns are prioritized.
As you navigate your journey with diabetes, ongoing updates to these guidelines are essential. They reflect the latest research and advancements in care, ensuring you receive the best possible support. Moreover, integrating technology and lifestyle modifications can significantly enhance your diabetes management. Together, these elements create effective strategies that empower you to take control of your health.
Remember, you are not alone in this journey. We encourage you to explore the resources available through the ADA and connect with others who share similar experiences. By doing so, you can find the support and information you need to thrive in managing your diabetes.
Introduction
In the realm of diabetes management, the American Diabetes Association (ADA) guidelines serve as a cornerstone for healthcare professionals who are dedicated to enhancing patient outcomes through evidence-based practices. Each year, these guidelines evolve, incorporating the latest research and clinical insights to ensure that patients receive care tailored to their unique circumstances.
The 2025 updates emphasize a patient-centered approach, advocating for individualized strategies that address the complexities of diabetes, including the pressing economic burden it imposes on the healthcare system. It's understandable to feel overwhelmed by these challenges. However, with a focus on innovative technologies, lifestyle modifications, and comprehensive support, the ADA guidelines aim not only to improve glycemic control but also to empower individuals living with diabetes to lead healthier, more fulfilling lives.
As the landscape of diabetes care continues to shift, understanding these guidelines becomes essential for both patients and providers alike. Remember, you’re not alone in this journey; we are here to support you every step of the way.
Overview of the American Diabetes Association Guidelines
The guidelines provided by the ADA for diabetes management serve as an essential framework for managing this condition, offering healthcare professionals evidence-based recommendations focused on improving outcomes for individuals. Updated annually, these guidelines incorporate the latest research and clinical practices, ensuring their relevance and effectiveness in a rapidly evolving healthcare landscape. A key focus of the ADA is a patient-centered approach, which emphasizes individualized care tailored to the unique needs and circumstances of each patient.
As we look ahead to 2025, the ADA guidelines for diabetes management continue to play a crucial role in diagnosing the condition, managing blood glucose levels, and addressing the multifaceted aspects of care. For instance, the guidelines highlight the importance of lifelong screening for individuals diagnosed with gestational diabetes mellitus (GDM), enabling early interventions that can significantly impact health management.
Recent statistics reveal the increasing economic burden of diabetes in the U.S., with costs soaring to over $412.9 billion in 2022, up from $327 billion in 2017. This alarming trend underscores the necessity for effective management strategies, as outlined in the ADA guidelines, to mitigate both health and financial impacts on individuals and the healthcare system.
As Charles “Chuck” Henderson, CEO, states, "Enhancing the lives of individuals impacted by health issues related to diabetes is a key part of the ADA’s mission." The ADA provides the reliable assistance required for individuals living with diabetes and their supporters to manage the illness and thrive until we discover a cure.
At T2DSolutions, we recognize the importance of these guidelines and are dedicated to offering newly diagnosed individuals the resources and support they need. Our platform will serve as a comprehensive resource hub, providing educational materials, community support, and tools to help individuals navigate their diabetes management journey effectively.
Real-world examples illustrate the positive outcomes associated with the implementation of ADA guidelines for diabetes management. Healthcare facilities that have adopted these guidelines report improved adherence to treatment plans and better overall health metrics. The emphasis on a client-centered approach fosters a collaborative environment where individuals feel empowered to take an active role in their care.
As we examine the updates for 2025, the evolving ADA guidelines for diabetes management reflect advancements in research and care techniques. This ongoing dedication to enhancement is vital for addressing the challenges of care and ensuring that individuals receive the most effective assistance possible. By prioritizing a patient-centered approach, the ADA guidelines not only improve the care of individuals with this condition but also contribute to a better quality of life for those affected.
Remember, you’re not alone in this journey. T2DSolutions is here to support you every step of the way.
Key Updates in the 2025 ADA Diabetes Guidelines
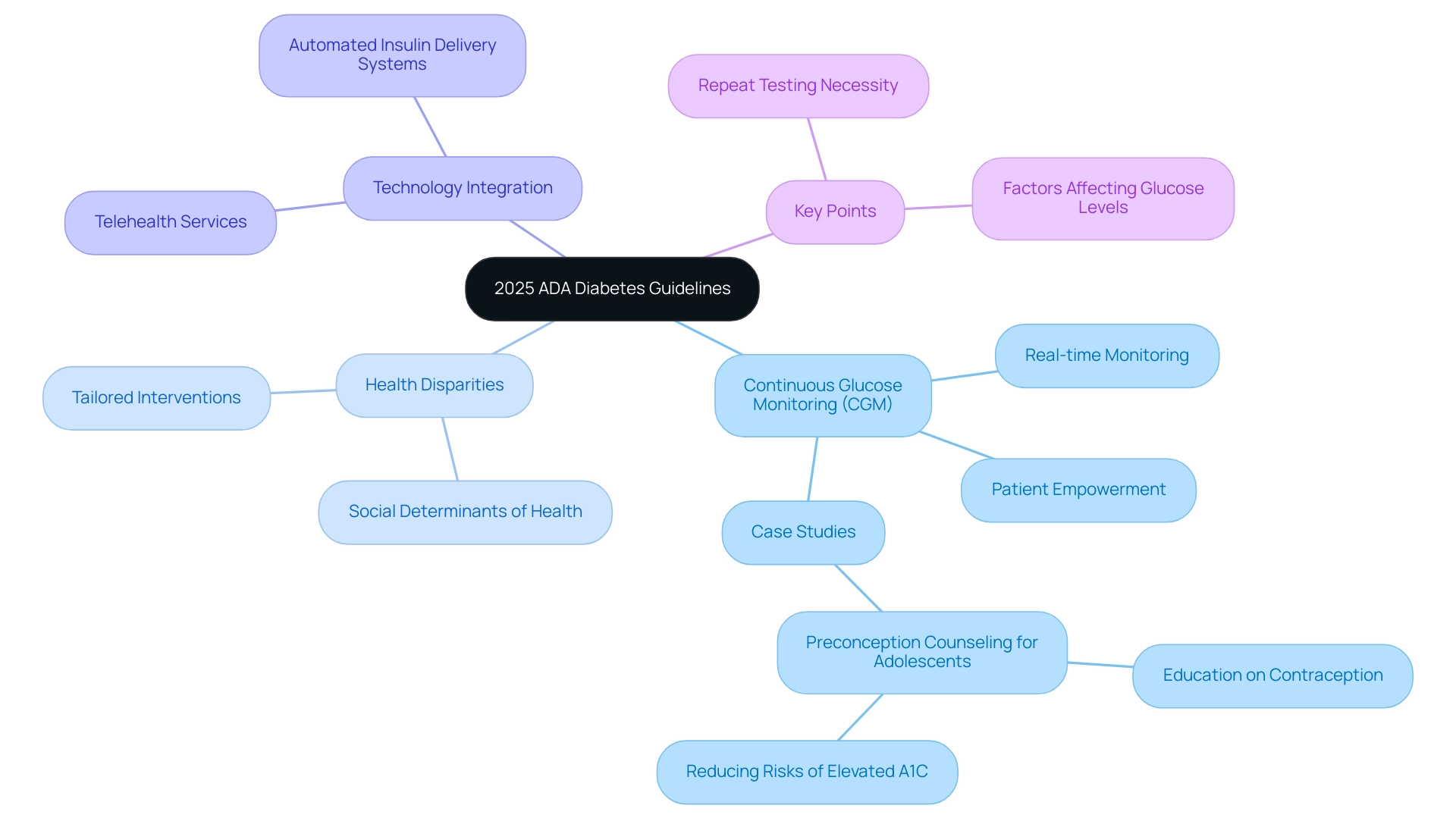
The 2025 ADA guidelines for diabetes management introduce several crucial updates aimed at improving care for individuals living with diabetes. A significant recommendation is the use of continuous glucose monitoring (CGM) for adults with Type 2 diabetes who are on glucose-lowering medications other than insulin. This approach not only assists in real-time glucose monitoring but also empowers patients to make informed choices regarding their well-being.
Statistics reveal that around 136 million Americans are living with blood sugar issues or prediabetes, highlighting the urgent need for effective control strategies. As Charles “Chuck” Henderson, CEO, states, "Enhancing the lives of individuals impacted by health issues related to diabetes is a key part of the ADA’s mission." The ADA provides the reliable assistance required for individuals managing diabetes and those supporting them, helping them to thrive until we discover a remedy.
The guidelines also emphasize the importance of addressing health disparities in diabetes care, advocating for interventions tailored to the unique social determinants affecting diverse populations. This focus on inclusivity is vital, ensuring that all individuals, regardless of their background, have access to the resources they need for effective health management.
Moreover, the integration of technology in glucose management is a key theme in the ADA guidelines. The use of automated insulin delivery systems and telehealth services has gained prominence, especially in the wake of the COVID-19 pandemic, which has reshaped healthcare delivery. These advancements reflect the ADA's commitment to improving patient outcomes through innovative and inclusive care strategies.
A crucial element of blood sugar control emphasized in the ADA guidelines is the necessity for repeated testing when results conflict, as various factors can influence glucose levels. Real-world applications of CGM have shown promising results in managing Type 2 diabetes. For instance, case studies highlight the positive impact of CGM on patient adherence to treatment plans and overall glycemic control.
One significant case study involves preconception guidance for teenagers with blood sugar issues, emphasizing the importance of education on contraception and preconception counseling to prevent unplanned pregnancies and related risks. Experts note that incorporating CGM into routine care for blood sugar management not only enhances monitoring but also fosters a proactive approach to managing the condition.
In summary, the 2025 ADA guidelines for diabetes management encapsulate a forward-thinking approach, emphasizing the importance of technology, inclusivity, and tailored interventions to improve health outcomes for all individuals living with diabetes. You're not alone in this journey; we are here to support you every step of the way.
Pharmacologic Management Strategies for Type 2 Diabetes
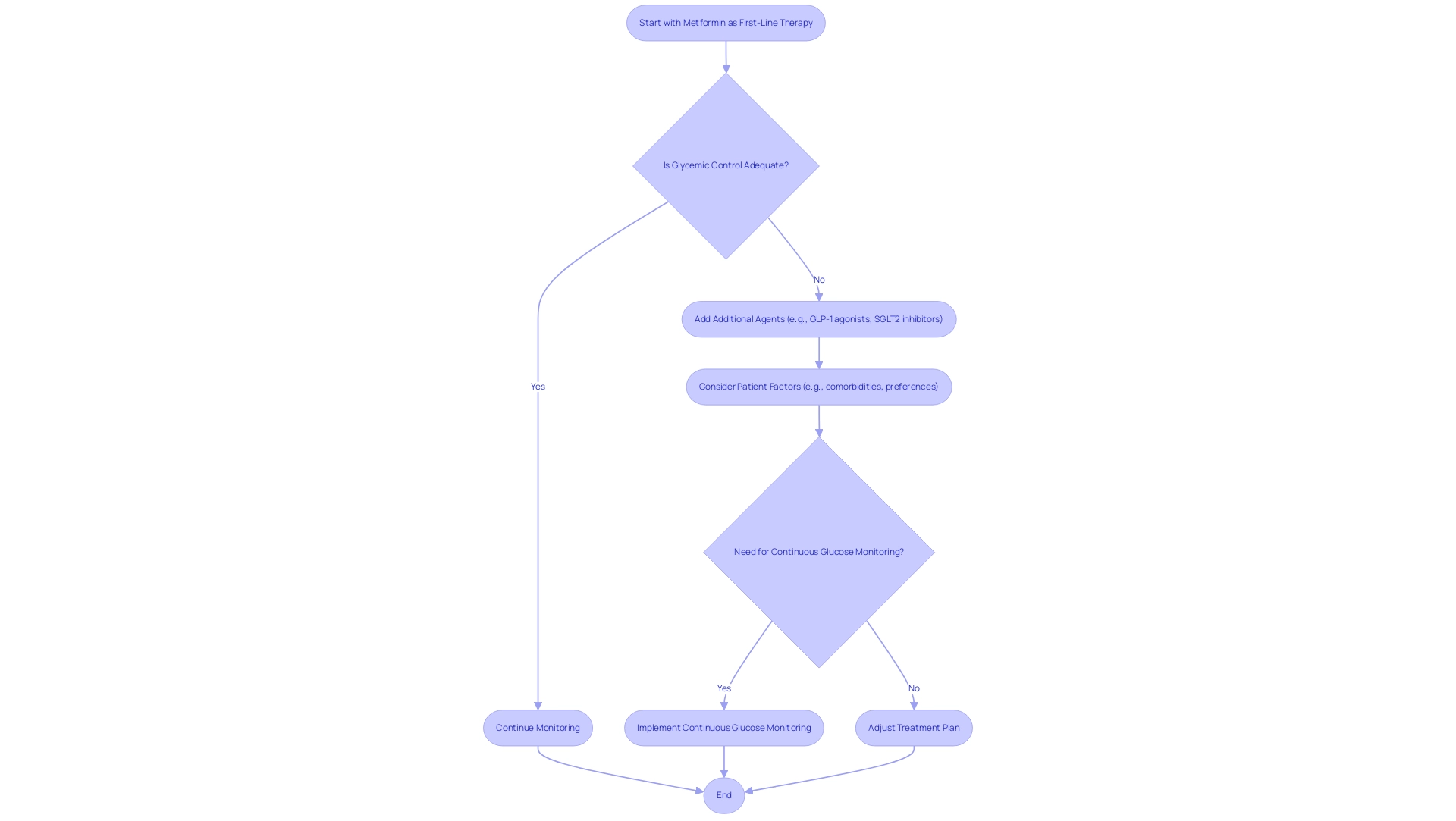
Pharmacologic treatment of Type 2 diabetes is essential for effective diabetes care, as highlighted by the ADA guidelines for diabetes management in 2025. These guidelines encourage a stepwise approach to medication oversight, starting with metformin as the first-line therapy. Metformin has consistently shown its effectiveness in lowering blood glucose levels and is well-regarded for its safety profile.
For those who find that metformin alone does not provide adequate glycemic control, the guidelines suggest adding other agents, such as GLP-1 receptor agonists or SGLT2 inhibitors. These medications not only help with glycemic control but also offer significant benefits in weight management and cardiovascular health, addressing the multifaceted challenges faced by individuals with diabetes.
The ADA guidelines emphasize the importance of tailoring treatment plans to individual needs, taking into account personal preferences, existing comorbidities, and potential side effects. This personalized approach is vital, as it empowers individuals to engage actively in their care. Regular monitoring and reassessment of medication efficacy and safety are critical components of this strategy, ensuring that treatment remains effective and minimizes the risk of complications.
Real-world examples illustrate the effectiveness of metformin as a first-line therapy. Many individuals have successfully controlled their condition with metformin, often achieving significant improvements in their blood glucose levels and overall well-being. Moreover, the DECLARE-TIMI 58 study highlights the importance of cardiovascular factors in managing diabetes-related conditions, revealing that the rate of cardiovascular mortality or hospitalization for heart failure was 4.9% for individuals on dapagliflozin, compared to 5.8% for those on placebo.
The ADA recommends that patients at high risk for cardiovascular events receive primary preventive therapy with low-dose, enteric-coated aspirin, underscoring the necessity for comprehensive cardiovascular care.
Additionally, the guidelines suggest considering continuous glucose monitoring (CGM) for adults with Type 2 Diabetes who are using non-insulin glucose-lowering agents. This can enhance glycemic control and provide valuable insights into blood sugar patterns.
The case study titled 'Complications of Diabetes Mellitus' underscores that this condition can lead to acute and chronic complications, including cardiovascular disease, retinopathy, nephropathy, and neuropathy. Education on controlling blood glucose levels is essential to prevent these complications, emphasizing the importance of effective care.
Moreover, pramlintide acetate, an amylin analog that mimics endogenous amylin effects, is emerging as an additional pharmacologic option that delays gastric emptying and modulates appetite, further diversifying the treatment landscape.
In summary, the 2025 ADA guidelines for diabetes management provide a comprehensive framework for pharmacologic treatment of Type 2 diabetes, emphasizing a stepwise approach that begins with metformin and incorporates additional therapies as needed. This strategy not only enhances glycemic control but also addresses broader health concerns, ultimately improving the quality of life for individuals managing blood sugar issues. At T2DSolutions, we are dedicated to supporting newly diagnosed patients by offering valuable resources and education to help you navigate your health management journey.
Subscribe to our updates to stay informed about new content and tools available to assist you.
Lifestyle Modifications: Diet and Exercise Recommendations
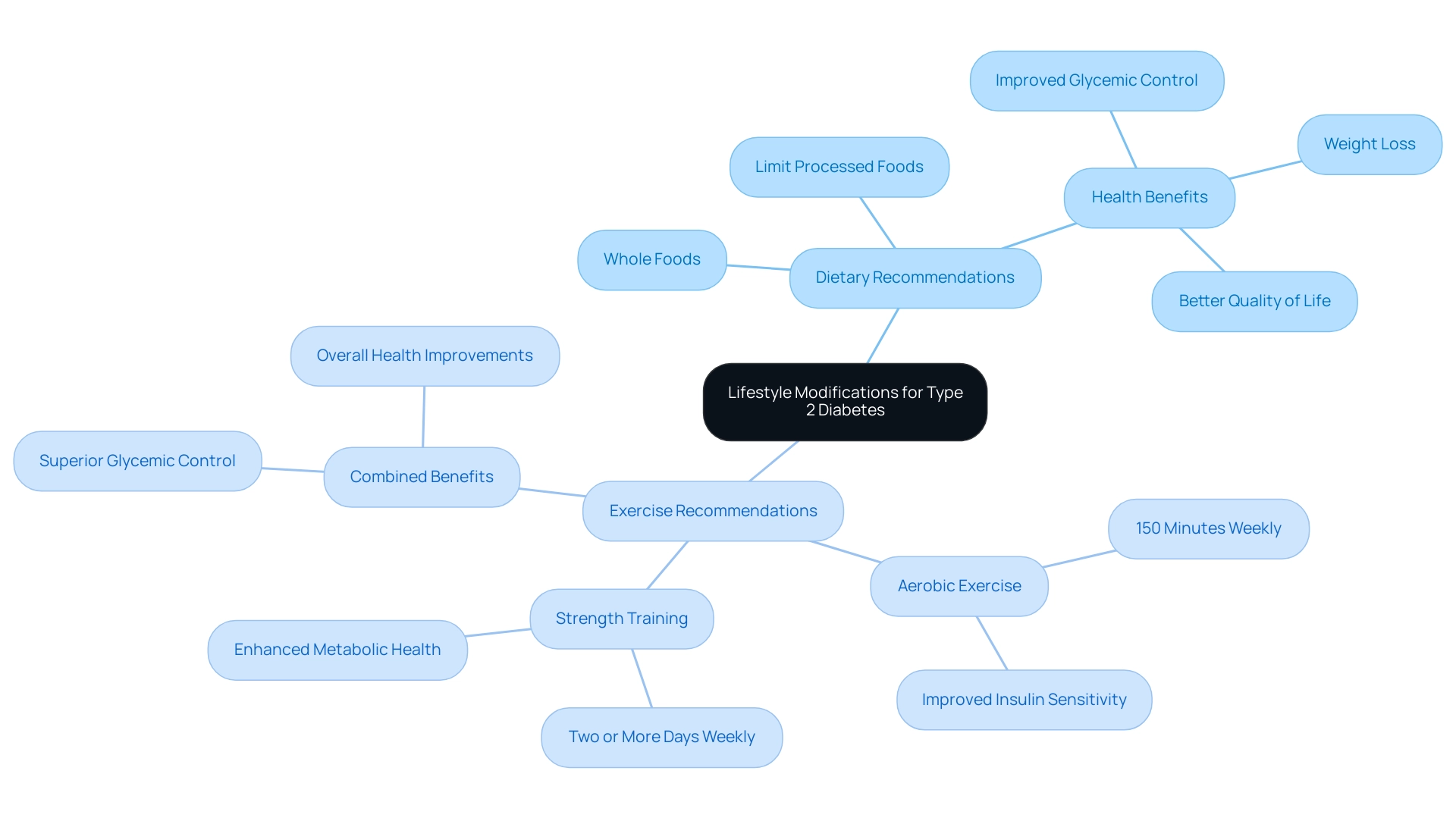
Lifestyle modifications are essential for effectively managing Type 2 diabetes, as highlighted by the ADA guidelines for diabetes management. These guidelines advocate for a balanced diet that emphasizes whole foods, including a variety of fruits, vegetables, whole grains, lean proteins, and healthy fats. By limiting processed foods, added sugars, and saturated fats, you can significantly enhance your glycemic control and overall well-being.
In addition to dietary changes, the ADA guidelines recommend engaging in regular physical activity. Aim for at least 150 minutes of moderate-intensity aerobic exercise each week, supplemented with strength training on two or more days. This combination has been shown to enhance insulin sensitivity and metabolic well-being. It’s important to know that combining aerobic and resistance workouts can yield superior results in glycemic control compared to either approach alone.
This information is especially significant, as resistance exercise has been demonstrated to enhance strength, insulin sensitivity, and metabolic health.
Statistics show that 80.6% of adults with this condition also encounter elevated blood pressure or are receiving treatment for hypertension. This highlights the importance of lifestyle changes in managing not only diabetes but also related medical issues. Real-world examples reveal that individuals who follow these dietary and exercise recommendations often experience weight loss, improved cardiovascular fitness, and a better quality of life.
The effect of these lifestyle changes on blood sugar control is profound. Case studies illustrate that patients who implement these modifications see significant improvements in their blood glucose levels and overall health. Experts consistently emphasize that adopting a holistic approach to diet and exercise is crucial for effectively managing blood sugar levels. This aligns with the ADA guidelines for diabetes management and reinforces the commitment to empowering you with the knowledge and resources you need to thrive.
As Charles 'Chuck' Henderson, CEO of the ADA, states, "Enhancing the lives of individuals affected by this condition is a key part of the ADA’s mission." The ADA offers trusted support for individuals living with diabetes and those caring for them, helping you manage the disease and thrive until a cure is found.
In this context, T2DSolutions aims to serve as a comprehensive resource hub for individuals managing Type 2 diabetes. By providing educational materials, community support, and practical tools, T2D Solutions is dedicated to helping you implement these lifestyle modifications effectively. Additionally, the World Health Assembly has endorsed five global coverage targets for managing blood sugar conditions to be achieved by 2030, emphasizing the need for strengthened prevention and control.
Remember, you’re not alone in this journey. We are here to support you every step of the way.
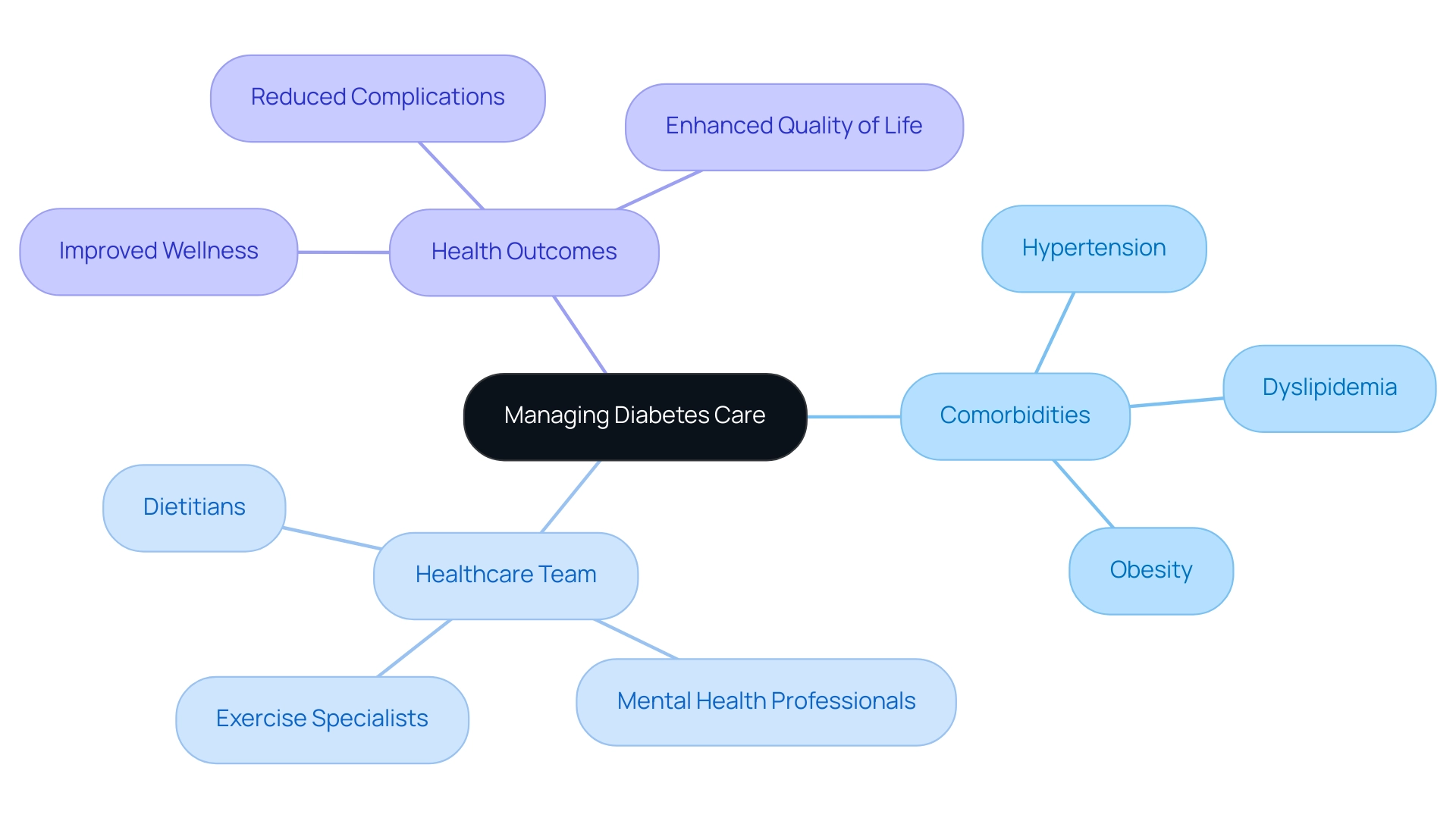
Managing Comorbidities: A Holistic Approach to Diabetes Care
Managing comorbidities is crucial for individuals with blood sugar issues, as many patients face additional health challenges such as:
- Hypertension
- Dyslipidemia
- Obesity
The 2025 ADA guidelines for diabetes management emphasize the necessity of a comprehensive strategy for managing diabetes-related care. This approach advocates for regular screening and proactive oversight of associated conditions. By integrating care, we not only enhance glycemic control but also reduce the risk of complications associated with the condition.
T2DSolutions serves as a valuable resource center for newly diagnosed individuals, offering education and support for managing diabetes and its comorbidities. It's important for healthcare providers to collaborate with multidisciplinary teams, which may include:
- Dietitians
- Mental health professionals
- Exercise specialists
This teamwork addresses the diverse aspects of a patient's wellness, ensuring that all conditions are managed concurrently, ultimately leading to improved health outcomes.
For instance, a recent case study highlighted the deintensification of treatment in older adults. It revealed that simplifying treatment plans can significantly reduce the burden of management while maintaining effective glycemic control. This approach is particularly important, as overtreatment can lead to increased risks of hypoglycemia and other complications.
Furthermore, the occurrence of comorbidities among individuals with high blood sugar in 2025 is remarkable. Cardiovascular conditions and mental health disorders are major factors in rising healthcare expenses. In fact, diabetes-related comorbidities significantly increase healthcare costs across all settings. By prioritizing the screening for hypertension and dyslipidemia, healthcare providers can identify and address these issues early, ultimately enhancing the overall well-being of individuals with this condition.
As Erin Byrne, MPH, highlights, "A comprehensive method for handling health conditions is crucial for enhancing individual results and quality of life." This thorough method not only encourages improved wellness results but also enhances a superior quality of life for patients, in line with the ADA guidelines for diabetes management. T2DSolutions is dedicated to supporting this vision by offering resources and education customized to the needs of those managing blood sugar conditions and their comorbidities.
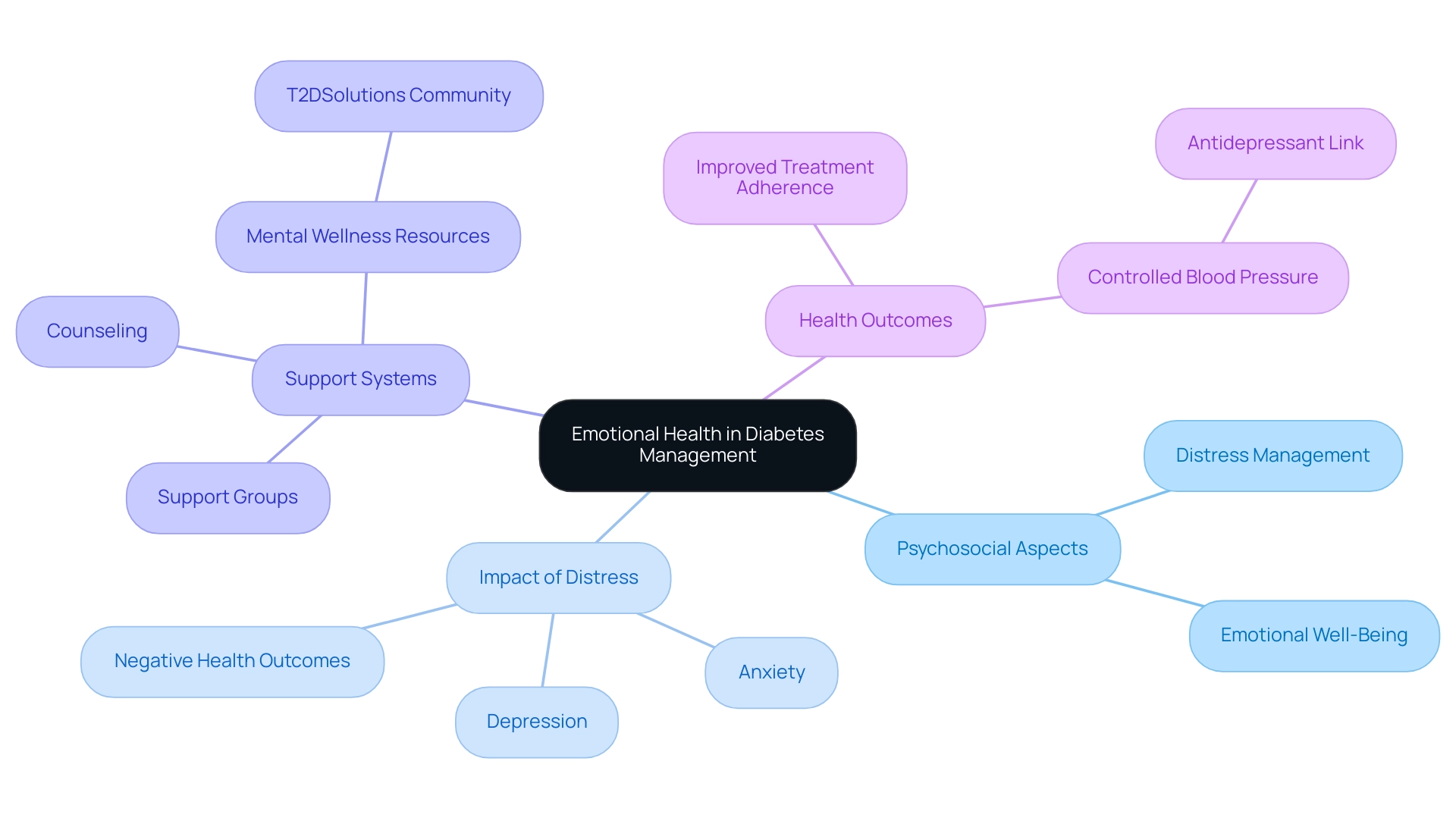
Psychosocial Support and Emotional Health in Diabetes Management
The psychosocial aspects of controlling blood sugar levels are crucial for achieving optimal wellness. It's important to recognize the role of emotional well-being, as highlighted in the ADA guidelines for diabetes management. Distress related to blood sugar management, along with feelings of depression and anxiety, can significantly affect a patient's ability to manage their condition effectively. Studies indicate that individuals grappling with emotional challenges alongside blood sugar issues face a heightened risk of negative outcomes. Therefore, it's essential for healthcare professionals to incorporate psychosocial evaluations into standard care.
While distress related to blood sugar often cannot be managed solely with medication, specialists emphasize the benefits of enhancing treatment to alleviate stress. Counseling and support groups can be incredibly advantageous. Healthcare professionals are encouraged to provide resources for mental wellness support, which might include referrals to mental wellness specialists, access to support groups, or community resources that foster connection and resilience. For instance, T2DSolutions exemplifies this approach by creating a supportive community where individuals can share their experiences and connect with others facing similar challenges.
T2DSolutions offers educational materials, workshops, and access to expert insights, all aimed at improving health outcomes by emphasizing the shared journey of managing this condition. By prioritizing emotional well-being, healthcare providers can enhance treatment adherence and improve the overall quality of life for those navigating this path. The link between emotional health and physical well-being is critical; statistics show that taking antidepressants is linked to a 95% increase in the likelihood of achieving controlled blood pressure among individuals with the condition.
As we approach World Diabetes Day on November 14, it's vital to acknowledge the ongoing significance of these matters in the realm of blood sugar control and emotional well-being. Remember, you're not alone in this journey. We are here to support you every step of the way, and the importance of psychosocial assistance in managing this health issue cannot be overstated. It plays a vital role in addressing the emotional challenges that accompany this chronic condition.
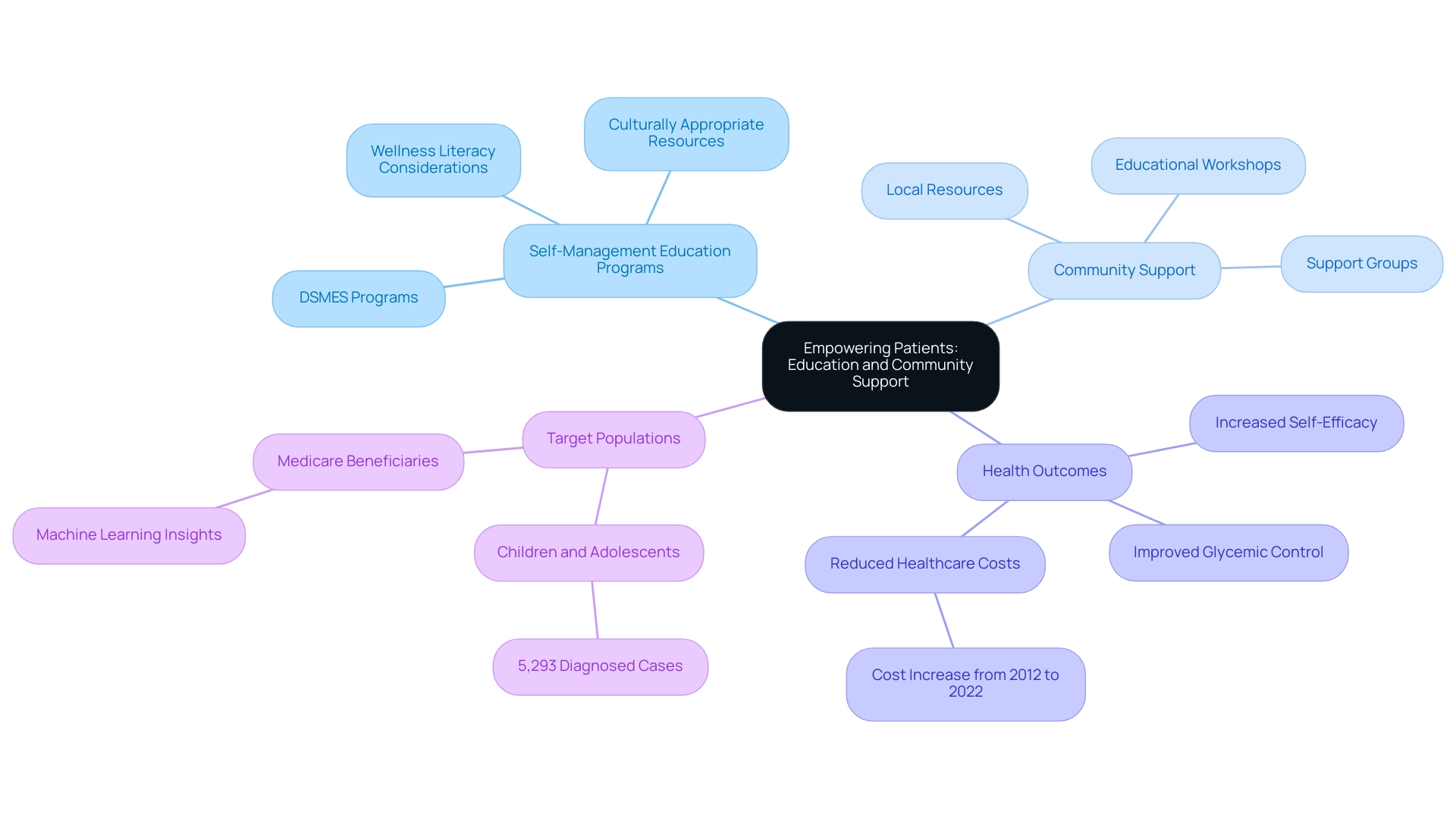
Empowering Patients: Education and Community Support
Enabling individuals through education and community assistance is essential for effectively managing diabetes. At T2DSolutions, we are dedicated to providing comprehensive self-management education and support (DSMES) programs that align with the ADA guidelines for diabetes management set for 2025. These programs are thoughtfully designed to equip individuals, particularly those who are newly diagnosed, with the vital knowledge and skills necessary for managing their condition effectively.
We understand that everyone’s journey is unique, which is why T2DSolutions will customize these programs to meet the diverse needs of individuals. This includes offering culturally appropriate resources and considering varying levels of wellness literacy.
Community support plays a crucial role in improving diabetes management outcomes. It fosters a sense of connection and solidarity among those living with diabetes. T2DSolutions will connect patients with local resources, support groups, and educational workshops, enhancing patient engagement and encouraging positive wellness behaviors. Research shows that effective DSMES programs can lead to improved health outcomes, with studies indicating that participants experience better glycemic control and reduced healthcare costs.
It's important to note that excess medical expenses related to diabetes rose from $10,179 in 2012 to $12,022 in 2022. This highlights the significant financial implications of having effective education and support programs in place.
Real-world examples illustrate how community support can positively impact diabetes management. For instance, local support groups facilitated by T2Solutions have demonstrated improvements in participants' self-efficacy and motivation, which in turn leads to better adherence to treatment plans. Additionally, expert insights reveal that community engagement not only provides emotional support but also facilitates access to essential resources, such as nutritional guidance and exercise programs.
The American Diabetes Association Professional Practice Committee has been actively involved in developing and disseminating ADA guidelines for diabetes management for over 35 years. This underscores the importance of organized support in navigating this condition.
The significance of self-management education and support in this area cannot be overstated. By empowering patients through education, they become better equipped to navigate their health journey, make informed decisions, and ultimately enhance their quality of life. T2Solutions' commitment to advancing DSMES programs in 2025 reflects a growing recognition of the need for personalized, community-oriented approaches to managing blood sugar conditions, ensuring that individuals receive the support they need to thrive.
With 5,293 children and adolescents aged 10 to 19 years diagnosed with type 2 diabetes, there is an urgent need for effective education and support programs tailored to younger populations. The case study titled 'Machine Learning Approaches for DSME Prediction' demonstrates how machine learning techniques are being used to enhance understanding of DSME engagement, identifying key variables that influence participation and advocating for personalized implementation strategies. You're not alone in this journey, and we are here to support you every step of the way.
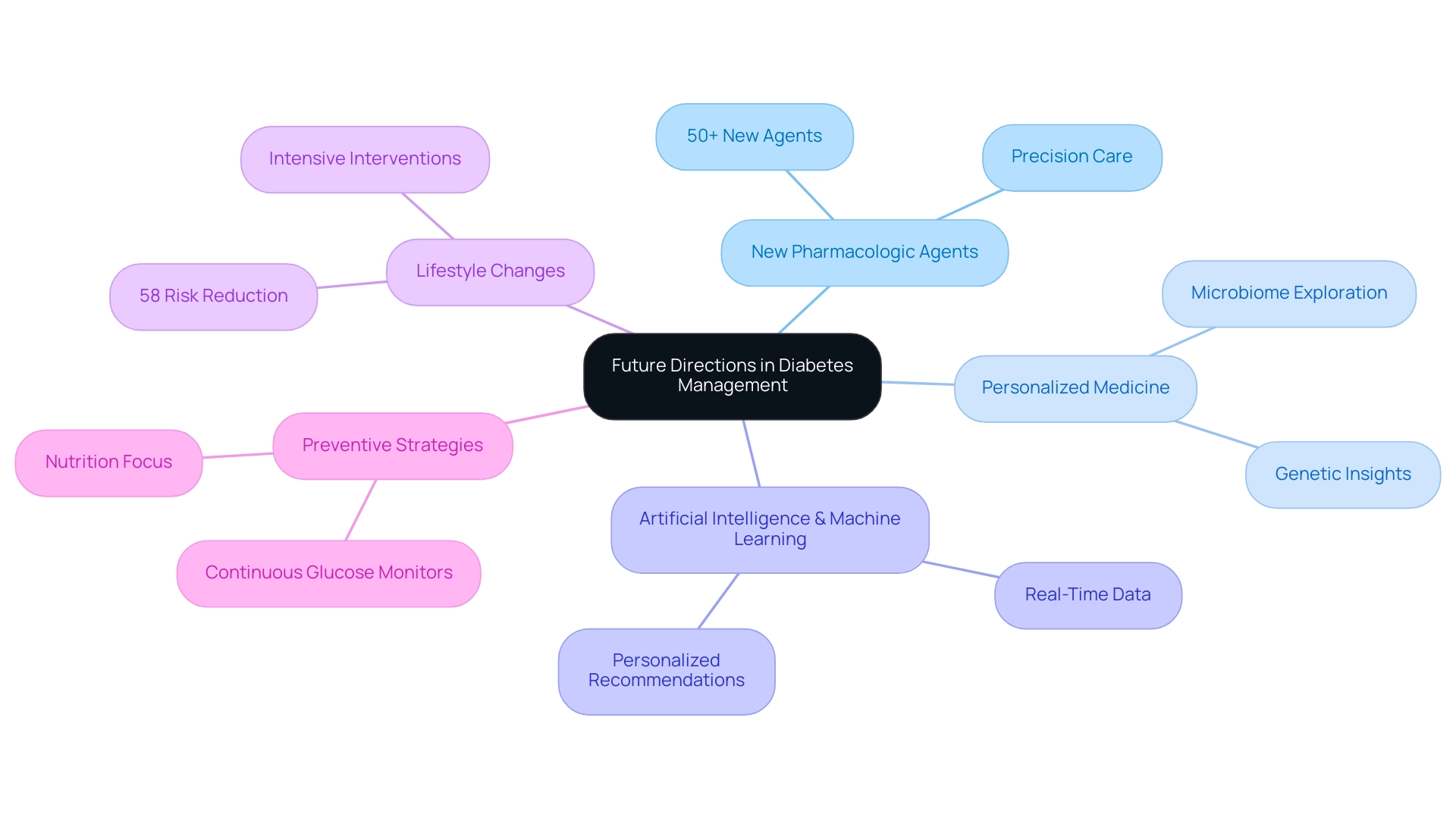
Future Directions in Diabetes Management and Research
The future of blood sugar management is poised for transformative advancements, driven by ongoing research and innovative technologies. It's an exciting time, with over 50 new pharmacologic agents expected to enter the treatment landscape. This could significantly enhance the precision and effectiveness of care, which is something we all hope for. Furthermore, the exploration of the microbiome, genetics, and personalized medicine is gaining momentum, promising to reshape treatment paradigms and tailor interventions to meet individual needs.
The integration of artificial intelligence and machine learning into diabetes management tools is anticipated to further improve outcomes for individuals. These technologies can provide real-time data and personalized recommendations, empowering healthcare providers to make informed decisions that align with each patient's unique circumstances. The American Diabetes Association's 2025 Standards of Care, which align with the ADA guidelines for diabetes management, emphasize the importance of continuous glucose monitors and nutrition. This reflects a meaningful shift towards comprehensive care strategies that leverage technology for better health outcomes.
It's heartening to note that the CDC National Center for Health Statistics tracks trends related to complications, revealing declines in visual impairment and amputations. This underscores the positive impact of these advancements on our community.
Moreover, intensive lifestyle changes have demonstrated a remarkable ability to reduce the likelihood of developing type 2 health issues by 58% in overweight or obese adults with prediabetes. This highlights the crucial role of preventive strategies in managing health conditions. As healthcare professionals navigate this evolving landscape, staying informed about emerging therapies and trends will be essential to delivering optimal care. As Dr. Mansur Shomali observes, "In the future, we may acknowledge that medications are essential to enable us to pursue modern lifestyles without elevating our risk of metabolic disorders." This emphasizes the importance of adapting treatment strategies to our current living conditions, considering new therapies and digital wellness tools.
In summary, the convergence of innovative therapies, digital health tools, and a focus on personalized care is set to redefine diabetes management. This ensures that healthcare providers are equipped to meet the diverse needs of their patients effectively. Remember, you're not alone in this journey; we are here to support you every step of the way.
Conclusion
The 2025 American Diabetes Association guidelines mark a significant step forward in diabetes management, focusing on a patient-centered approach that caters to individual needs. By incorporating the latest research and innovative technologies, these guidelines strive to enhance glycemic control and overall health outcomes, ensuring that you feel supported every step of the way.
Key updates highlight the importance of continuous glucose monitoring and address health disparities, underscoring the need for holistic care that also considers comorbidities. The pharmacologic management strategy begins with metformin, allowing for additional medications to further improve glycemic control while keeping cardiovascular health in mind.
Lifestyle changes, such as adopting a balanced diet and engaging in regular exercise, are vital components of effective diabetes management. These modifications contribute not only to better health outcomes but also to an improved quality of life. The guidelines emphasize the significance of psychosocial support and education, recognizing that your emotional well-being is crucial for successful diabetes management.
Overall, the 2025 ADA guidelines serve as a valuable resource for both healthcare providers and patients. By embracing innovative strategies and fostering collaboration, these guidelines aim to enhance clinical outcomes and improve the quality of life for those living with diabetes. Remember, you're not alone in this journey; this commitment to personalized care and ongoing research ensures you receive the necessary support to navigate your diabetes journey effectively, paving the way for a healthier future.
As you explore these guidelines, know that we are here to support you every step of the way. Seek out resources, connect with your healthcare team, and take comfort in the community that surrounds you.
Frequently Asked Questions
What is the purpose of the ADA guidelines for diabetes management?
The ADA guidelines provide an essential framework for managing diabetes, offering evidence-based recommendations aimed at improving outcomes for individuals with the condition.
How often are the ADA guidelines updated?
The ADA guidelines are updated annually to incorporate the latest research and clinical practices, ensuring their relevance and effectiveness.
What is a key focus of the ADA guidelines?
A key focus of the ADA guidelines is a patient-centered approach, emphasizing individualized care tailored to the unique needs and circumstances of each patient.
What role do the ADA guidelines play in diabetes care as we approach 2025?
The ADA guidelines continue to be crucial in diagnosing diabetes, managing blood glucose levels, and addressing the multifaceted aspects of care.
Why is lifelong screening for gestational diabetes mellitus (GDM) important according to the guidelines?
Lifelong screening for GDM is important as it enables early interventions that can significantly impact health management.
What is the economic burden of diabetes in the U.S. as of 2022?
The economic burden of diabetes in the U.S. soared to over $412.9 billion in 2022, highlighting the need for effective management strategies.
How does the ADA support individuals living with diabetes?
The ADA provides reliable assistance to individuals and their supporters to help manage diabetes and improve their quality of life.
What updates do the 2025 ADA guidelines introduce for Type 2 diabetes management?
The 2025 guidelines recommend the use of continuous glucose monitoring (CGM) for adults with Type 2 diabetes who are on glucose-lowering medications other than insulin.
What is the significance of addressing health disparities in diabetes care according to the guidelines?
Addressing health disparities is vital to ensure that all individuals, regardless of their background, have access to resources for effective health management.
How has technology been integrated into diabetes management as per the ADA guidelines?
The guidelines highlight the use of automated insulin delivery systems and telehealth services, reflecting a commitment to improving patient outcomes through innovative care strategies.
What is emphasized regarding blood sugar control in the ADA guidelines?
The guidelines emphasize the necessity for repeated testing when glucose results conflict, as various factors can influence glucose levels.
Can you provide an example of the positive impact of continuous glucose monitoring (CGM)?
Case studies have shown that CGM can improve patient adherence to treatment plans and overall glycemic control, particularly in managing Type 2 diabetes.
What is the importance of preconception counseling for teenagers with blood sugar issues?
Preconception counseling is crucial to prevent unplanned pregnancies and related risks, emphasizing the need for education on contraception.
What overall approach do the 2025 ADA guidelines reflect in diabetes management?
The guidelines reflect a forward-thinking approach that emphasizes technology, inclusivity, and tailored interventions to improve health outcomes for individuals living with diabetes.
