Overview
The article focuses on the American Diabetes Association hypertension guidelines, emphasizing their importance in managing high blood pressure among individuals with diabetes. It highlights the necessity for regular monitoring, lifestyle modifications, and pharmacological interventions, supported by research showing that effective treatment strategies can significantly reduce complications and improve cardiovascular health outcomes.
Introduction
The rising prevalence of diabetes and hypertension poses significant challenges to public health, with both conditions frequently coexisting and exacerbating each other's effects.
Diabetes, characterized by uncontrolled blood sugar levels, and hypertension, marked by elevated blood pressure, are both linked to serious complications such as cardiovascular diseases and kidney failure.
Recent statistics indicate a troubling increase in diagnosed diabetes, highlighting the urgency for effective management strategies.
This article delves into the foundational aspects of these conditions, the interplay between them, and the latest guidelines for their management.
By understanding the critical relationship between diabetes and hypertension, individuals can better navigate their health journeys, utilizing available resources to implement informed lifestyle changes and treatment plans.
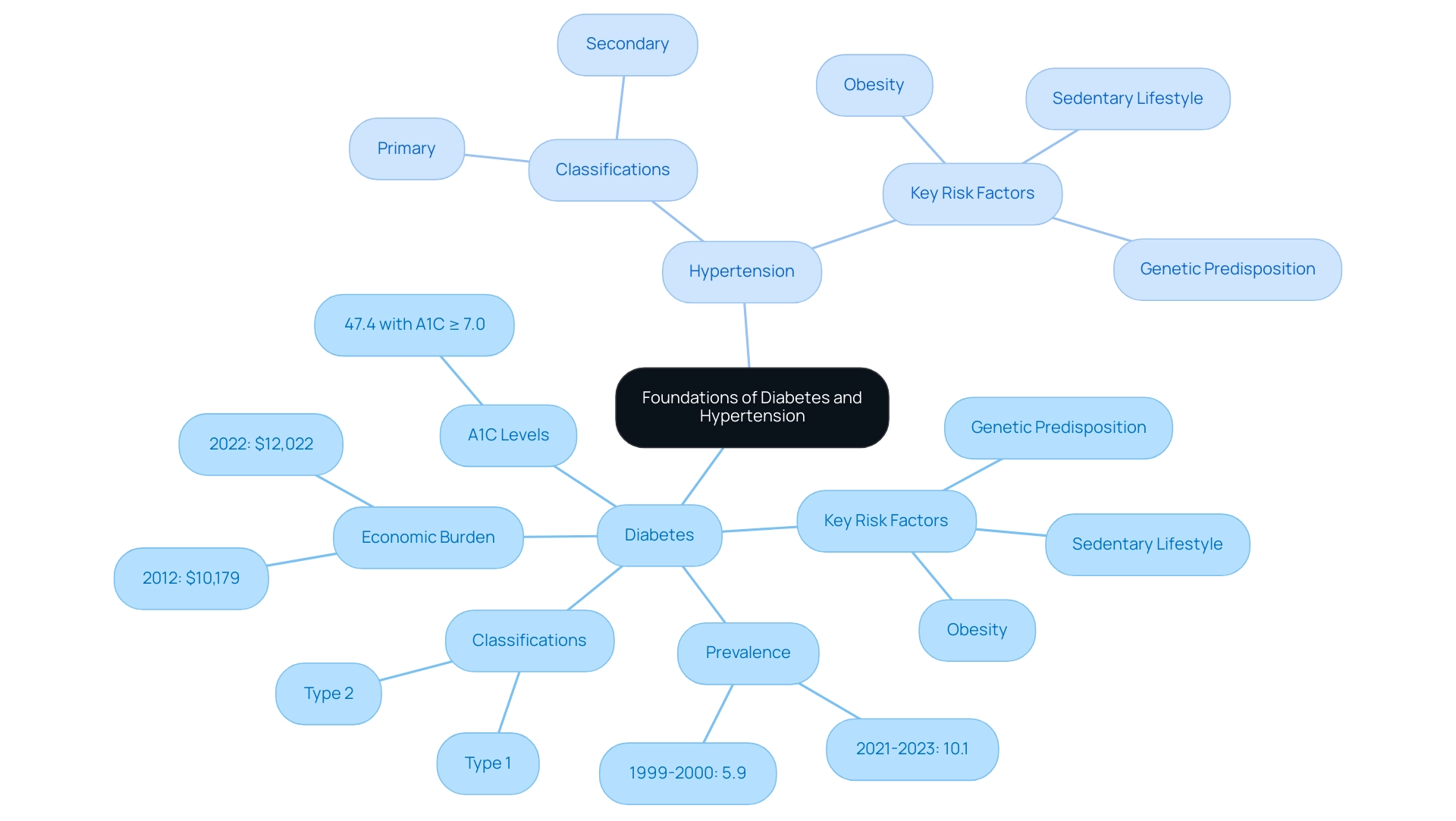
Foundations of Diabetes and Hypertension: Understanding the Basics
Diabetes is a chronic condition characterized by elevated sugar levels resulting from the body's inability to produce or utilize insulin effectively. In parallel, high blood pressure, commonly referred to as such, is characterized by a consistent elevation in the force of blood against arterial walls. Both elevated blood sugar levels and hypertension are prevalent in the American population, often coexisting and significantly increasing the risk of cardiovascular diseases, as highlighted by the American Diabetes Association hypertension guidelines.
According to the National Center for Health Statistics, the age-adjusted prevalence of diagnosed conditions related to blood sugar rose from 5.9% in 1999–2000 to 10.1% in August 2023, underscoring an alarming public health concern. Moreover, excess medical expenses per individual linked to the condition increased from $10,179 in 2012 to $12,022 in 2022, highlighting the economic burden of the illness. Key risk factors for both conditions include:
- Obesity
- A sedentary lifestyle
- Genetic predisposition
These factors are critical to recognize for effective management.
Diabetes includes various classifications, such as type 1 and type 2 forms, while hypertension can be categorized as primary or secondary. A case study revealed that among adults with this condition, 47.4% had an A1C value of 7.0% or higher, indicating a substantial portion are not achieving optimal glycemic control, which emphasizes the need for improved management strategies. Grasping these foundational concepts is essential for those recently diagnosed to implement effective management strategies and enhance their health outcomes.
T2DSolutions acts as an essential resource center, providing extensive education and community assistance for individuals managing Type 2 and Type 3 conditions, helping empower individuals with the knowledge and tools required for improved health. Stay tuned for our upcoming resources that will further assist you in your journey, and consider subscribing to receive updates on new content and features from T2D Solutions.
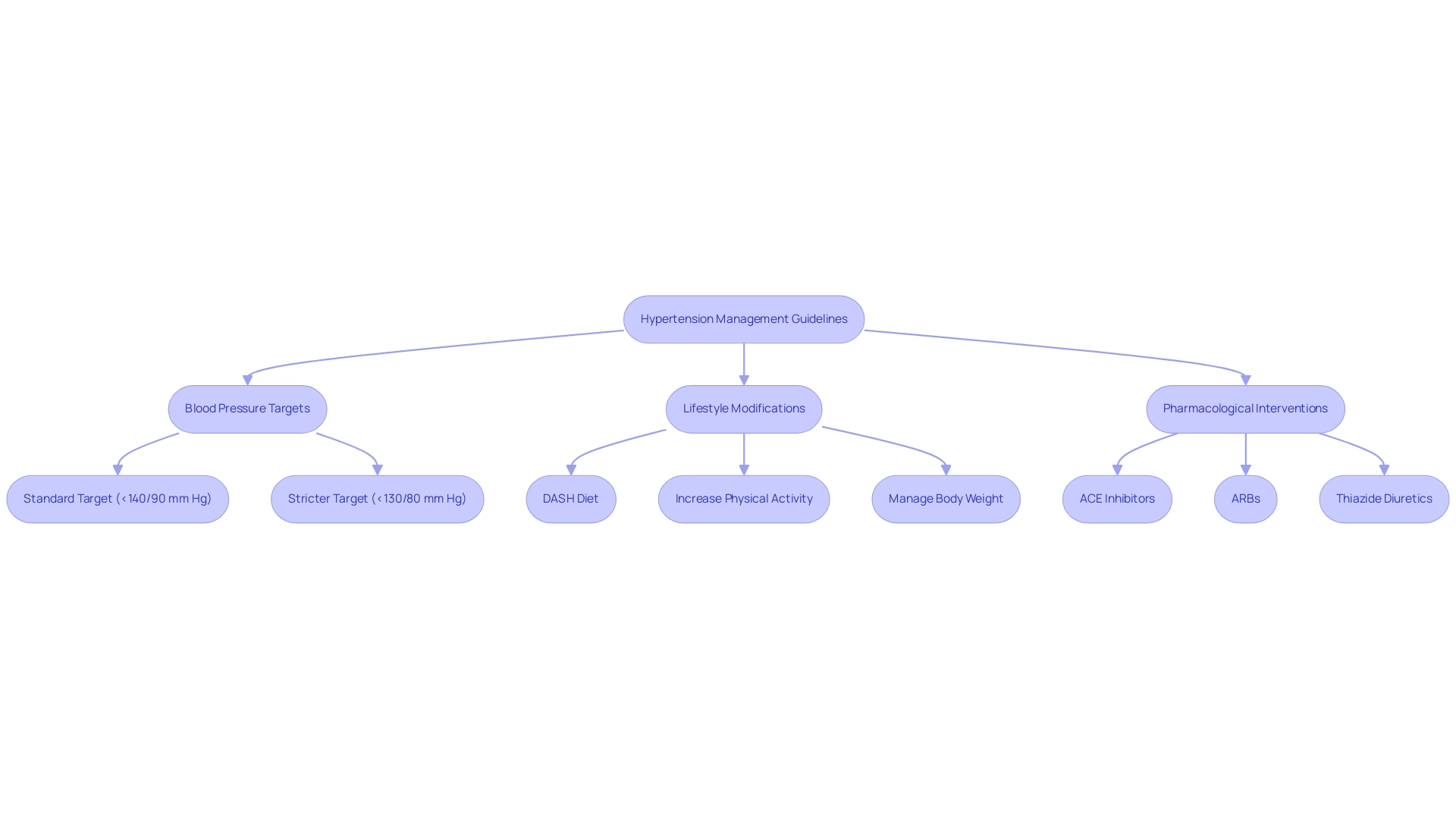
Key Hypertension Guidelines from the American Diabetes Association
The American Diabetes Association hypertension guidelines emphasize the critical need for regular blood pressure monitoring in individuals with the condition, recommending a target blood pressure of less than 140/90 mm Hg. For individuals with additional cardiovascular risk factors, the American Diabetes Association hypertension guidelines recommend a more stringent target of less than 130/80 mm Hg. These guidelines emphasize that lifestyle modifications should be the first line of defense; practical recommendations include:
- Adopting the DASH diet, which focuses on fruits, vegetables, and low-fat dairy
- Increasing physical activity
- Managing body weight effectively
Pharmacological interventions are also essential, particularly the use of ACE inhibitors, ARBs, and thiazide diuretics, which have shown efficacy in managing hypertension among individuals with diabetes. In the VERTIS CV trial, which followed 8,246 individuals with type 2 mellitus and established ASCVD for a median of 3.0 years, the use of ertugliflozin demonstrated significant cardiovascular outcomes, illustrating the importance of effective treatment strategies. Adherence to the American Diabetes Association hypertension guidelines is crucial for mitigating the risk of diabetes-related complications and enhancing overall cardiovascular health.
Furthermore, T2D Solutions aims to support patients in implementing these guidelines by providing educational resources and community support. The latest recommendations highlight the importance of collaboration between primary care and specialty professionals to ensure comprehensive care transitions for high-risk individuals. As noted by the American Diabetes Association Professional Practice Committee, 'Recommendation 16.5a was added to delineate the glycemic goals for most critically ill individuals with hyperglycemia,' emphasizing the need for customized strategies in managing blood sugar and high blood pressure.
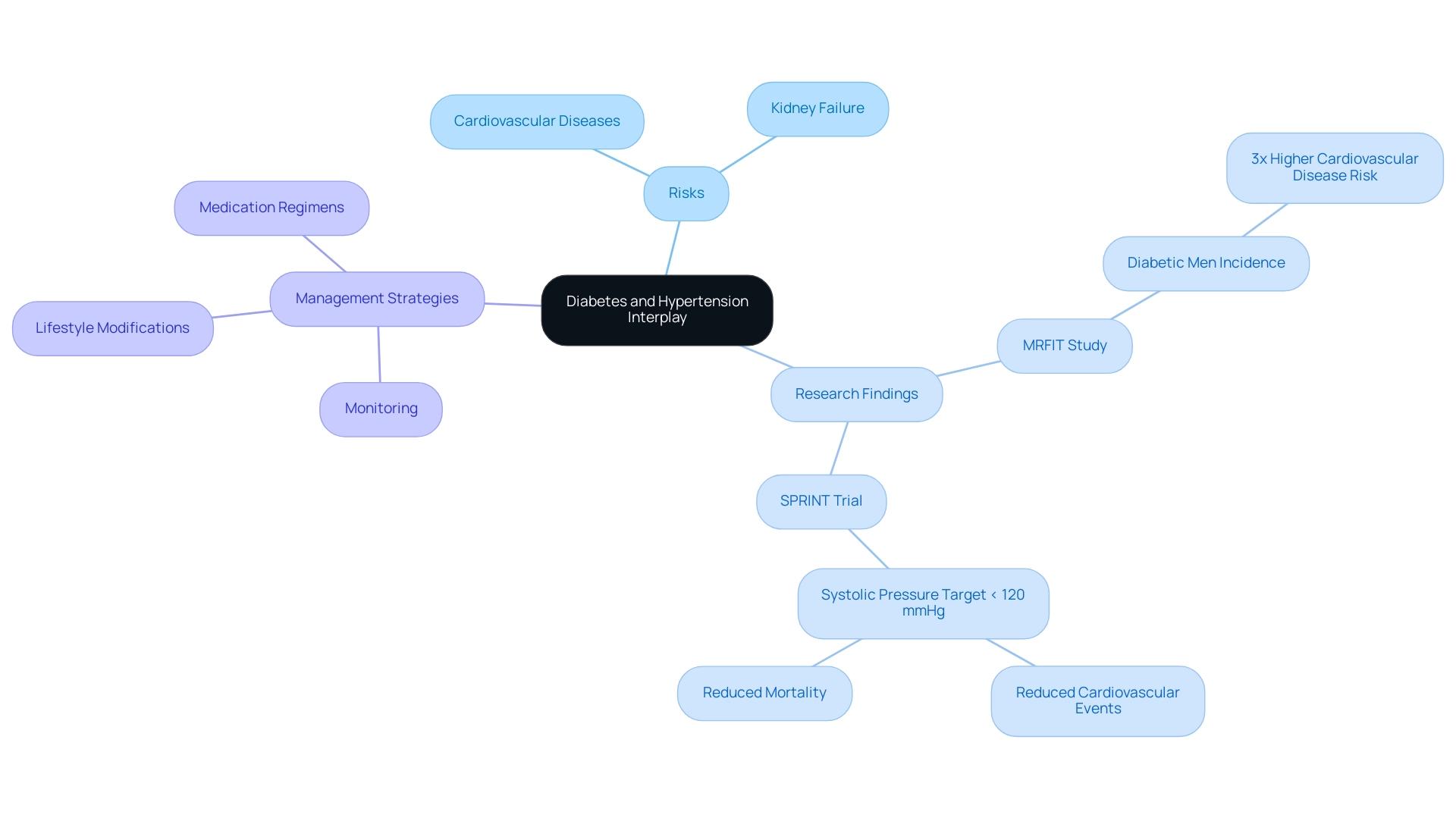
The Interplay Between Diabetes and Hypertension: Risks and Management Strategies
The coexistence of high blood pressure and elevated blood sugar significantly amplifies the risk of serious complications, including cardiovascular diseases and kidney failure. Research indicates that patients with diabetes are particularly susceptible to high blood pressure due to mechanisms such as insulin resistance and vascular damage. Additionally, hypertension can worsen diabetic complications by imposing extra strain on both the cardiovascular system and the kidneys.
The Multiple Risk Factor Intervention Trial (MRFIT) underscores this relationship, revealing that diabetic men experience up to three times the incidence of cardiovascular disease compared to non-diabetic counterparts, regardless of other risk factors. This highlights the vital necessity for comprehensive risk factor management.
Effective management strategies should prioritize the simultaneous control of glucose levels and blood pressure, especially by aiming for a systolic pressure of less than 120 mmHg, as recommended by the American Diabetes Association hypertension guidelines, which have shown that this approach can significantly reduce cardiovascular events and mortality. This integrated approach includes:
- Regular monitoring
- Lifestyle modifications
- Tailored medication regimens
With a focus on the degree of blood pressure reduction being more critical than the choice of antihypertensive medication.
At T2DSolutions, we strive to offer newly diagnosed individuals resources and assistance for managing both diabetes and high blood pressure. Our platform will provide educational resources, community assistance, and tools to help individuals recognize symptoms and adhere to their treatment plans. As T.J.G., a Senior Biomedical Fellow, states, "This work was supported by grants from the British Heart Foundation (RG/13/7/30099, RE/13/5/30177), the Wellcome Trust Senior Biomedical Fellowship, and the National Science Center of Poland (2011/03/B/NZ4/02454)."
Such expertise reflects the importance of a coordinated effort in managing these interrelated conditions to mitigate risks and improve overall health outcomes.
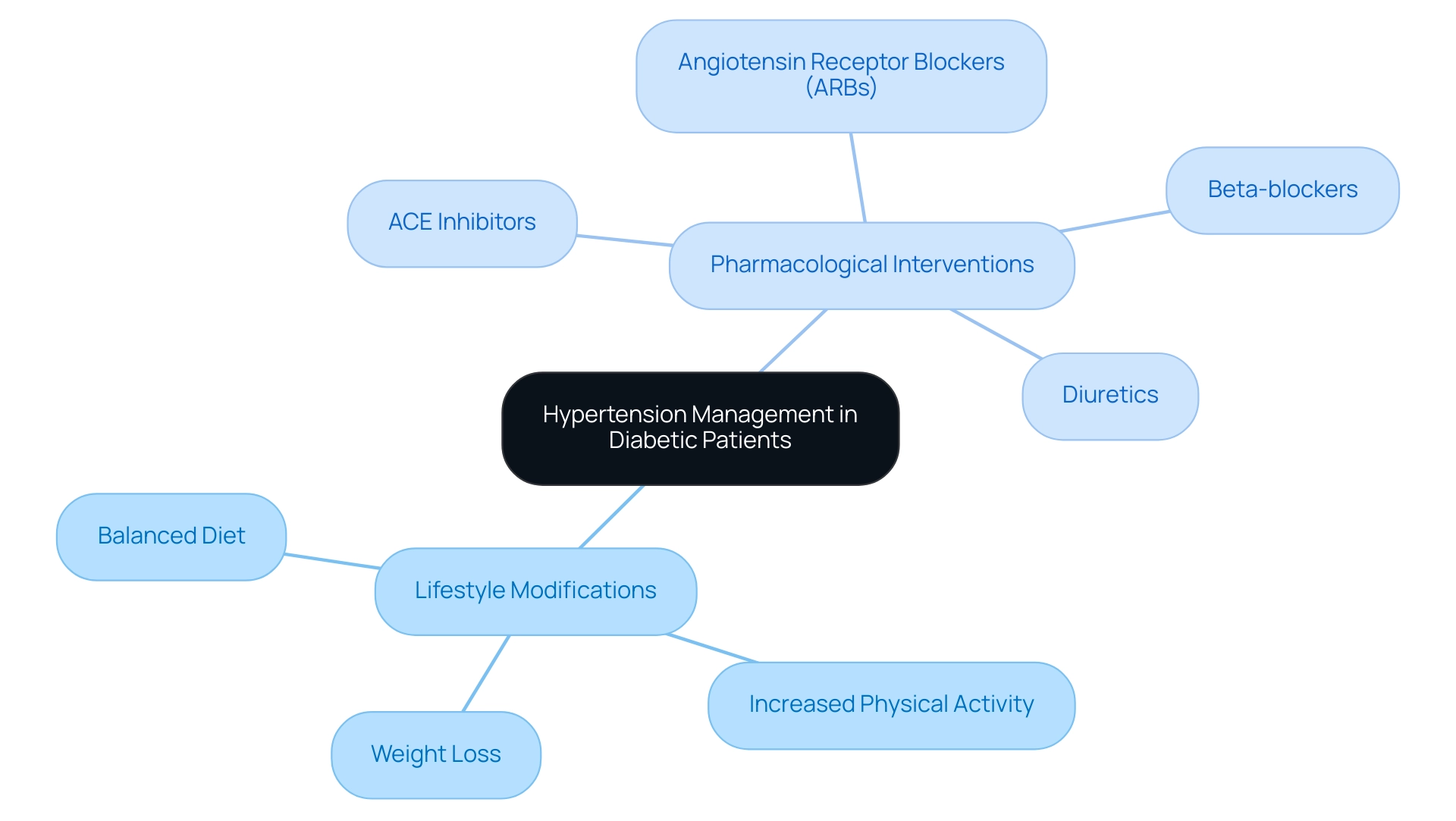
Treatment Approaches for Hypertension in Diabetic Patients
The management of high blood pressure in diabetic patients often begins with essential lifestyle modifications according to the American Diabetes Association hypertension guidelines. These changes typically include:
- Adopting a balanced diet
- Increasing physical activity
- Achieving weight loss
All of which play a significant role in blood pressure regulation. If these lifestyle adjustments do not yield sufficient results as outlined by the American Diabetes Association hypertension guidelines, pharmacological interventions become necessary.
According to the American Diabetes Association hypertension guidelines, medications such as:
- ACE inhibitors
- Angiotensin receptor blockers (ARBs)
- Beta-blockers
- Diuretics
have demonstrated effectiveness in controlling hypertension among individuals with diabetes. The choice of a specific medication may rely on various factors, including the individual's overall health, existing comorbidities, and the potential for side effects. Regular review and adjustment of treatment plans are crucial, as they should be tailored to the individual's response to therapy.
Notably, a recent study indicated that fasting insulin levels showed a reduction of −0.95 μIU/mL, illustrating that effective management strategies can lead to measurable health improvements. Furthermore, ongoing research underscores the necessity of continuously integrating lifestyle interventions into routine care, in accordance with the American Diabetes Association hypertension guidelines, ensuring that both lifestyle and pharmacological approaches are utilized for optimal blood pressure control. As George J. Fodor observed, 'The outcomes of this study align with those of George J. Fodor,' highlighting the increasing agreement on the necessity for a dual strategy in managing high blood pressure among individuals with diabetes.
Additionally, a case study titled 'Sustainability of Lifestyle Intervention Effects' reviewed the long-term outcomes of lifestyle interventions, highlighting that while some showed sustained effects on T2D incidence, others did not maintain significant differences over time. This reinforces the importance of continuous integration of lifestyle strategies into patient care, ultimately aiming to reduce the risk of cardiovascular events.
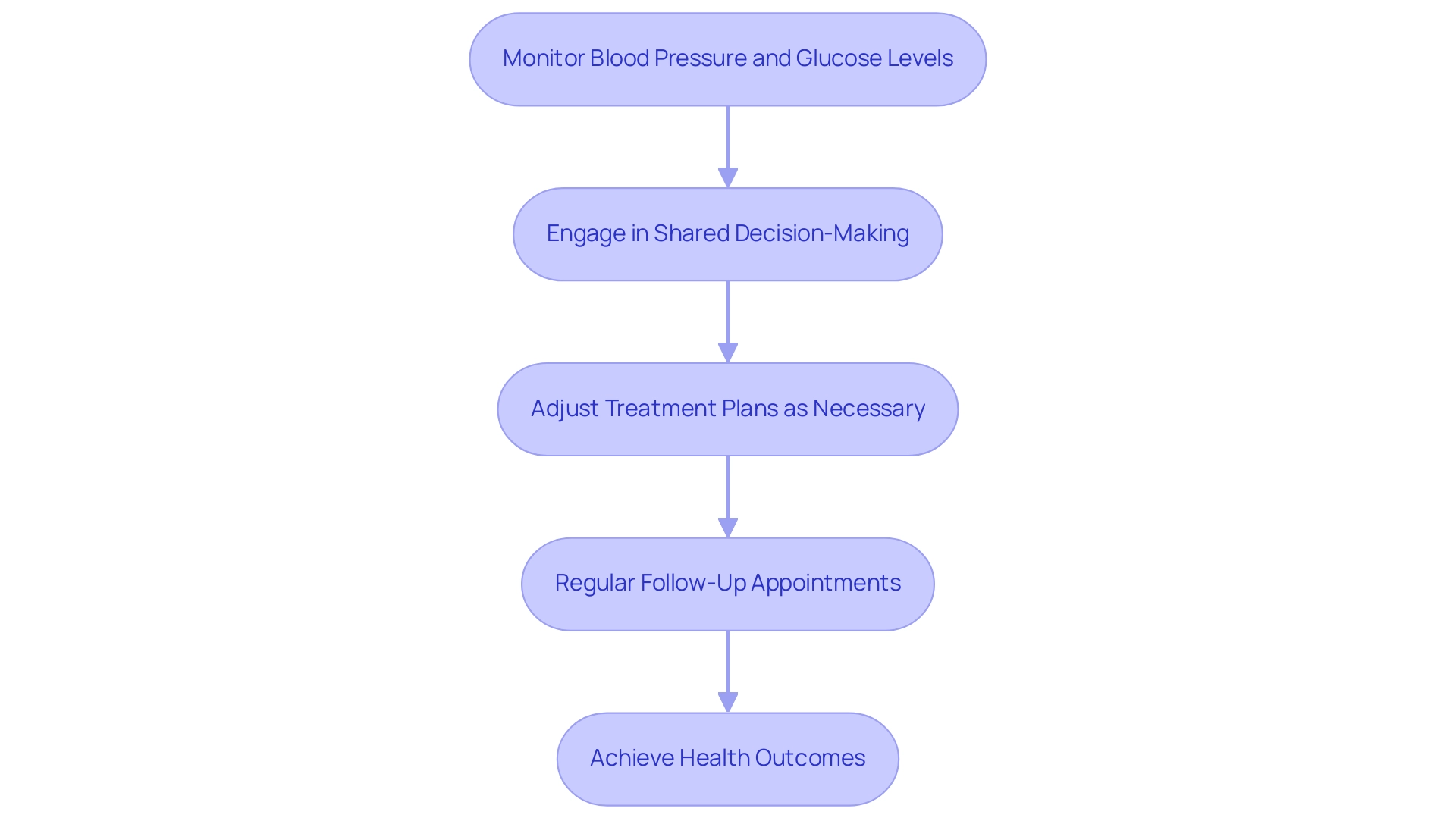
Personalized Care: Monitoring and Adjusting Hypertension Treatment in Diabetes
As T2DSolutions launches as a comprehensive resource hub for Type 2 and Type 3 diabetes education and community support, personalized care remains fundamental in effectively managing hypertension among individuals with diabetes, according to the American Diabetes Association hypertension guidelines. Regular monitoring of blood pressure and blood glucose levels, along with overall health assessments, is essential for evaluating the effectiveness of treatment strategies according to the American Diabetes Association hypertension guidelines. Healthcare providers at T2DSolutions are encouraged to engage in shared decision-making with individuals, considering their individual preferences, values, and lifestyle factors.
Adjustments to treatment plans may be necessary based on responses, potential side effects, and changes in health status. Regular follow-up appointments, along with transparent communication between individuals and healthcare providers, are essential components for successful management. Evidence indicates that patients who possess a copy of their care plan are significantly more likely than those without to achieve their treatment goals, including systolic blood pressure and low-density lipoprotein targets, with odds ratios indicating substantial improvements (SBP OR, 1.39; LDL OR, 1.46; p<0.001).
Furthermore, studies indicate that integrated care for blood sugar management enhances quality of care and health outcomes, with the good management group demonstrating lower HbA values (β of -0.217, p = .008). The case study titled 'Personalized Medicine Benefits for Diabetes' illustrates that personalized medicine, which tailors treatments based on individual genetic profiles, could lead to more effective therapies and prevention strategies. T2DSolutions will provide a range of resources, including educational materials on managing the condition, access to support groups for shared experiences, and tools for monitoring health metrics.
As such, implementing personalized care strategies not only enhances patient adherence but also improves overall health outcomes, underscoring its importance in hypertension management as outlined by the American Diabetes Association hypertension guidelines for those living with diabetes.
Conclusion
The interplay between diabetes and hypertension presents a complex challenge that requires a comprehensive understanding of both conditions. As outlined, diabetes is characterized by elevated blood sugar levels, while hypertension involves increased blood pressure, both of which can exacerbate each other and lead to serious health complications. The statistics reveal a concerning rise in diagnosed diabetes and the associated economic burden, emphasizing the need for effective management strategies.
Key guidelines from the American Diabetes Association stress the importance of:
- Regular blood pressure monitoring
- Lifestyle modifications as first-line interventions
The recommendation for a target blood pressure of less than 140/90 mm Hg, or even lower for those with additional risk factors, highlights the necessity of proactive management. The effectiveness of pharmacological treatments, coupled with lifestyle changes, is crucial in mitigating the risks associated with these coexisting conditions.
The evidence presented underscores that the coexistence of diabetes and hypertension significantly elevates the risk of:
- Cardiovascular diseases
- Kidney failure
Integrated management strategies that focus on controlling both blood sugar and blood pressure are essential. Personalized care, regular monitoring, and patient engagement in treatment decisions play pivotal roles in achieving optimal health outcomes.
In conclusion, understanding the relationship between diabetes and hypertension is vital for effective management. Armed with the right resources and knowledge, individuals can take charge of their health, implement informed lifestyle changes, and work collaboratively with healthcare providers to navigate the complexities of these conditions. The commitment to ongoing education and support from platforms like T2DSolutions will empower patients to make meaningful strides in their health journeys.



