Overview:
A good GMI percentage is essential for effective diabetes management, as it provides a real-time estimate of average glucose levels, helping patients and healthcare providers assess glycemic control. The article emphasizes that understanding GMI, alongside traditional metrics like HbA1c, enables timely adjustments in treatment and lifestyle, ultimately improving health outcomes for individuals managing their diabetes.
Introduction
The Glucose Management Indicator (GMI) has emerged as a vital tool in the realm of diabetes management, providing a modern approach to understanding glycemic control.
As healthcare continues to evolve, the integration of GMI with traditional metrics like HbA1c offers a more nuanced view of a patient's glucose levels, allowing for timely interventions and personalized treatment plans.
This article delves into the significance of GMI, its practical applications, and how it complements existing diabetes management strategies.
By exploring the relationship between GMI and other critical metrics such as Time in Range (TIR), healthcare professionals and patients alike can better navigate the complexities of diabetes care, ultimately leading to improved health outcomes.
Understanding the Glucose Management Indicator (GMI)
The Glucose Management Indicator (GMI) is a vital metric derived from continuous monitoring data, providing an estimate of a person's average sugar levels over a designated timeframe. Expressed as a percentage, understanding what is a good GMI percentage is an indispensable tool for both patients and healthcare providers in evaluating glycemic control. Unlike traditional methods, GMI offers a more immediate reflection of glucose levels, facilitating timely adjustments in treatment strategies and lifestyle modifications.
Comprehending GMI is essential for individuals overseeing their condition, as it enables them to make informed health decisions. According to Elsayed et al., it is recommended to assess glycemic status, including A1C or other measurements, at least twice a year for patients meeting goals, and quarterly for those not meeting glycemic targets. This highlights the significance of regular monitoring in enhancing management of blood sugar.
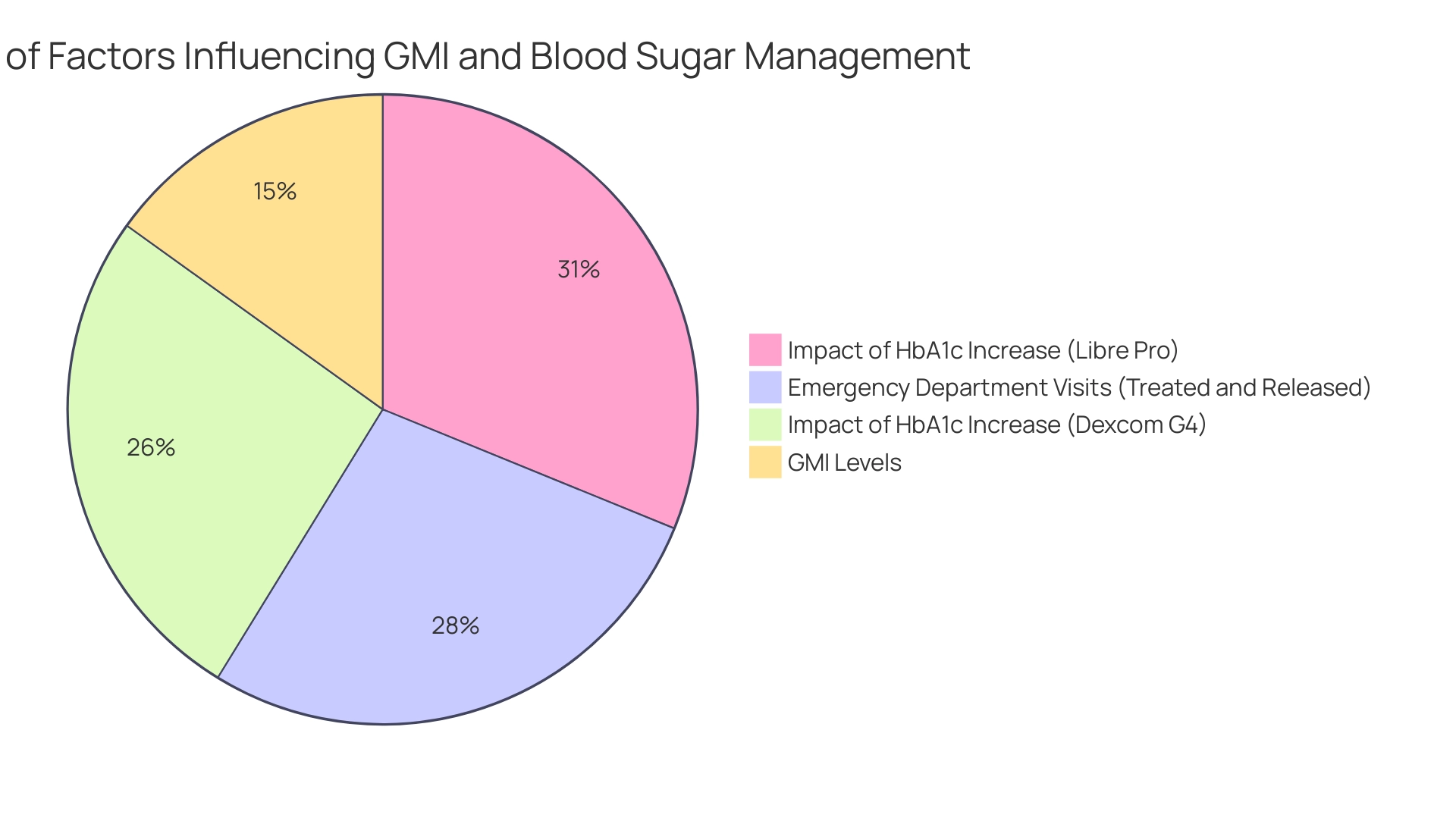
Furthermore, unjustified insurance coverage criteria limit access to CGM, which is considered a necessary tool for effective management of the condition. Recent statistics indicate that for every 1 percentage point increase in HbA1c, mean sugar levels rise significantly—approximately 52 mg/dL for the Dexcom G4 and 62 mg/dL for the Libre Pro. These figures underscore the direct relationships between GMI and average sugar levels, highlighting what is a good GMI percentage for managing blood sugar conditions.
For instance, effective glucose management can significantly reduce emergency department visits; in 2020, among emergency department visits with any listed diagnosis related to blood sugar issues, 54.9% were treated and released, showcasing the importance of proactive management strategies. Additionally, T2DSolutions provides a comprehensive resource hub designed to assist newly diagnosed individuals in understanding their GMI levels and managing their condition effectively. By providing educational materials, community support, and access to the latest management tools for the condition, T2 Solutions empowers individuals to take control of their health and make informed decisions regarding their glycemic control.
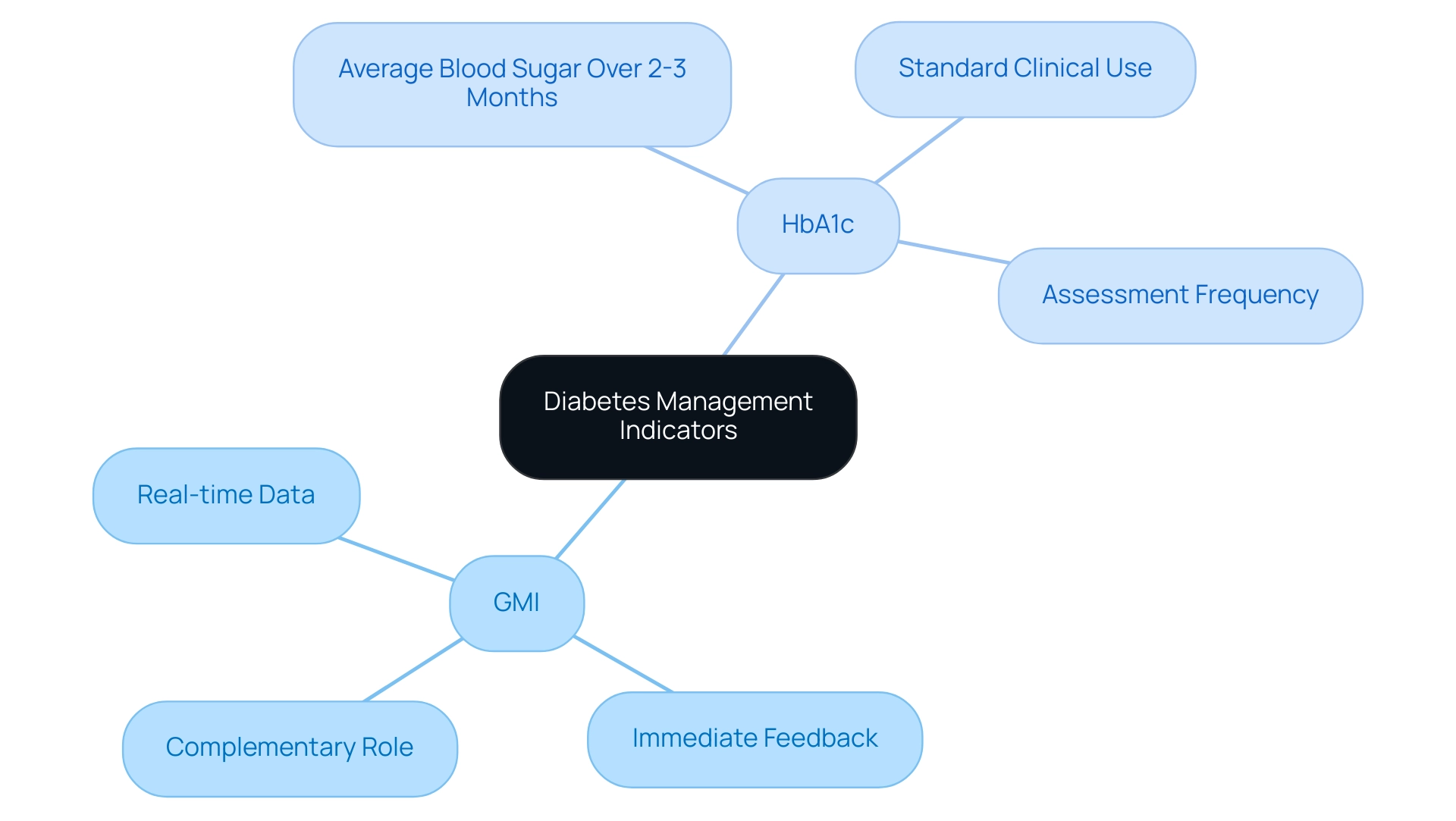
Comparing GMI and HbA1c: Key Differences and Similarities
The Glycemic Management Indicator (GMI) and HbA1c are both integral measures utilized in the management of diabetes, each serving distinct roles in care. HbA1c, a long-established standard, reflects the average blood sugar levels over a period of two to three months. This metric is widely employed in clinical settings to assess a patient's overall glycemic control.
In contrast, GMI provides a more immediate viewpoint by utilizing real-time data from continuous monitoring (CGM) systems. As such, GMI provides timely feedback on glucose fluctuations, enabling healthcare providers to make quicker adjustments to treatment regimens. According to Elsayed et al., it is crucial to assess glycemic status at least twice a year for individuals meeting goals, and more frequently for those not achieving their glycemic targets.
While both GMI and HbA1c are valuable indicators of glycemic control, their complementary nature is crucial for a comprehensive understanding of a patient's health. Recent studies, including findings from a study on pregnant women with type 1 conditions, have shown a significant negative correlation between time in range and HbA1c, underscoring the importance of interpreting discrepancies between these two metrics. The case study titled 'Clinical Implications of CGM and HbA Discrepancies' further illustrates that understanding these differences can prevent under- or overtreatment of this condition.
Therefore, a robust understanding of both GMI and HbA1c is essential for optimizing care related to blood sugar management.
Applying GMI in Diabetes Management: Practical Insights
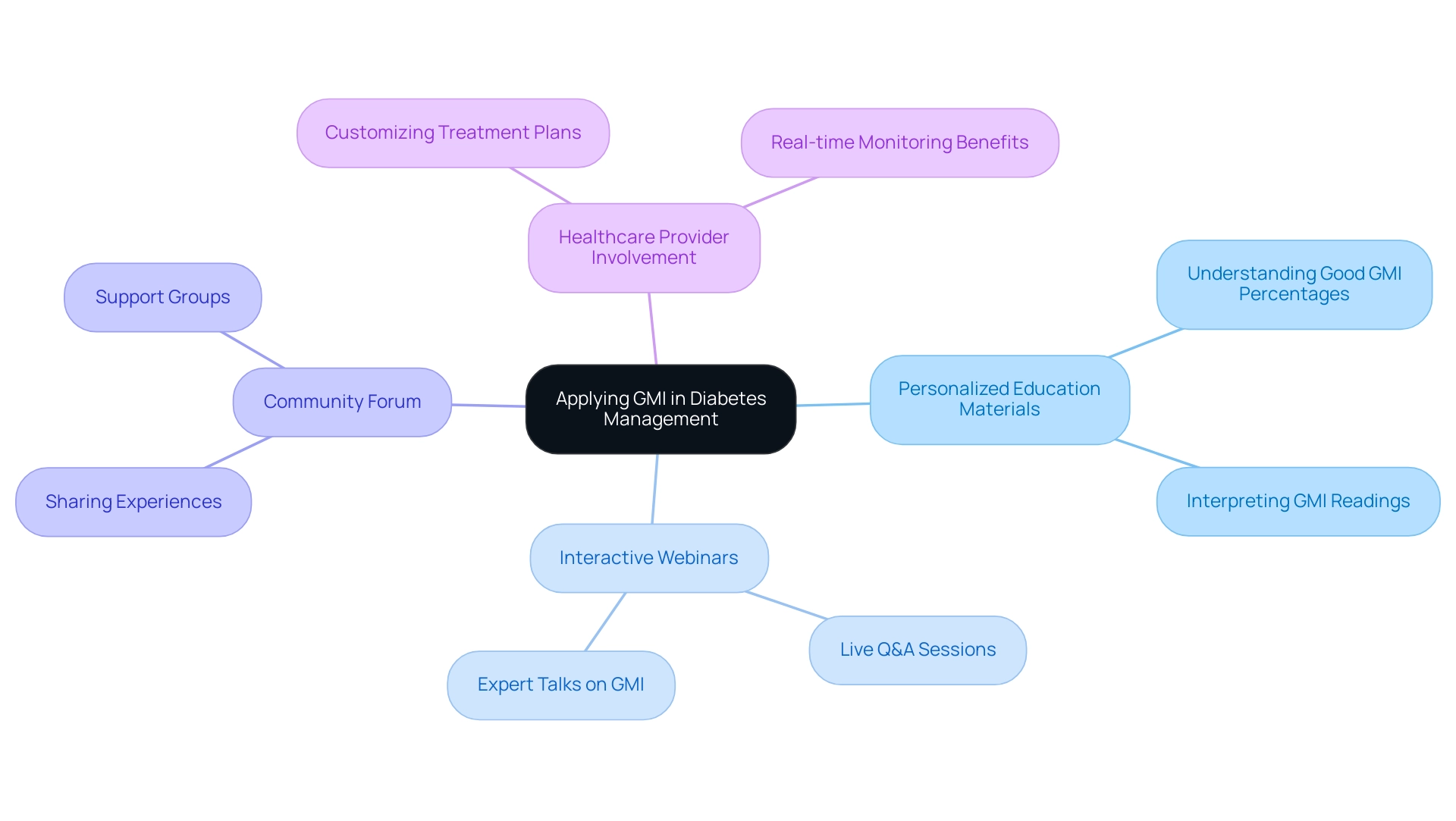
Incorporating Glycemic Management Indicator (GMI) into blood sugar control entails a structured and practical approach that T2DSolutions aims to support, particularly in answering what is a good GMI percentage. As a newly launched resource hub for Type 2 and Type 3 diabetes education and community support, T2D Solutions is committed to providing those recently diagnosed with the tools needed to understand what is a good GMI percentage for effectively utilizing GMI readings. This includes:
- Personalized education materials
- Access to interactive webinars
- A community forum for sharing experiences
By making informed adjustments to their carbohydrate intake, medication dosages, and physical activity levels, individuals can enhance their self-management. Healthcare providers play a pivotal role by leveraging GMI data to customize treatment plans that address what is a good GMI percentage for the unique needs of each individual, ensuring timely and relevant interventions. For example, if an individual's GMI shows increased sugar levels, a healthcare professional might suggest dietary changes or alterations in medication.
It's noteworthy that in the Libre Pro study, 18% of participants had a difference of greater than 1.0 percentage points (>11 mmol/mol), leading us to consider what is a good GMI percentage, which highlights the variability in GMI readings. Furthermore, understanding what is a good GMI percentage is essential for interpreting these readings in the context of traditional measures, especially since the original ADAG and DCCT equations do not fully align with GMI. T2DSolutions will educate individuals on what is a good GMI percentage and how to accurately interpret their GMI readings, empowering them to engage proactively in their health management, ultimately leading to enhanced health outcomes and an improved quality of life.
This proactive approach is supported by findings from the HypoDE Study, which demonstrated that real-time continuous glucose monitoring significantly reduces the risk of severe hypoglycemic events, underscoring the practical applications of GMI in daily care for individuals with blood sugar management. As Andre E. Manov observes, 'The incorporation of GMI into management of blood sugar levels can significantly improve outcomes for individuals by offering a clearer view of glycemic control,' a principle that T2DSolutions embodies as it unveils its extensive support for individuals, prompting the inquiry of what is a good GMI percentage. Additionally, testimonials from early users of T2D Solutions highlight how these resources have positively influenced their condition management journey.
The Role of Time in Range (TIR) in Managing Diabetes with GMI
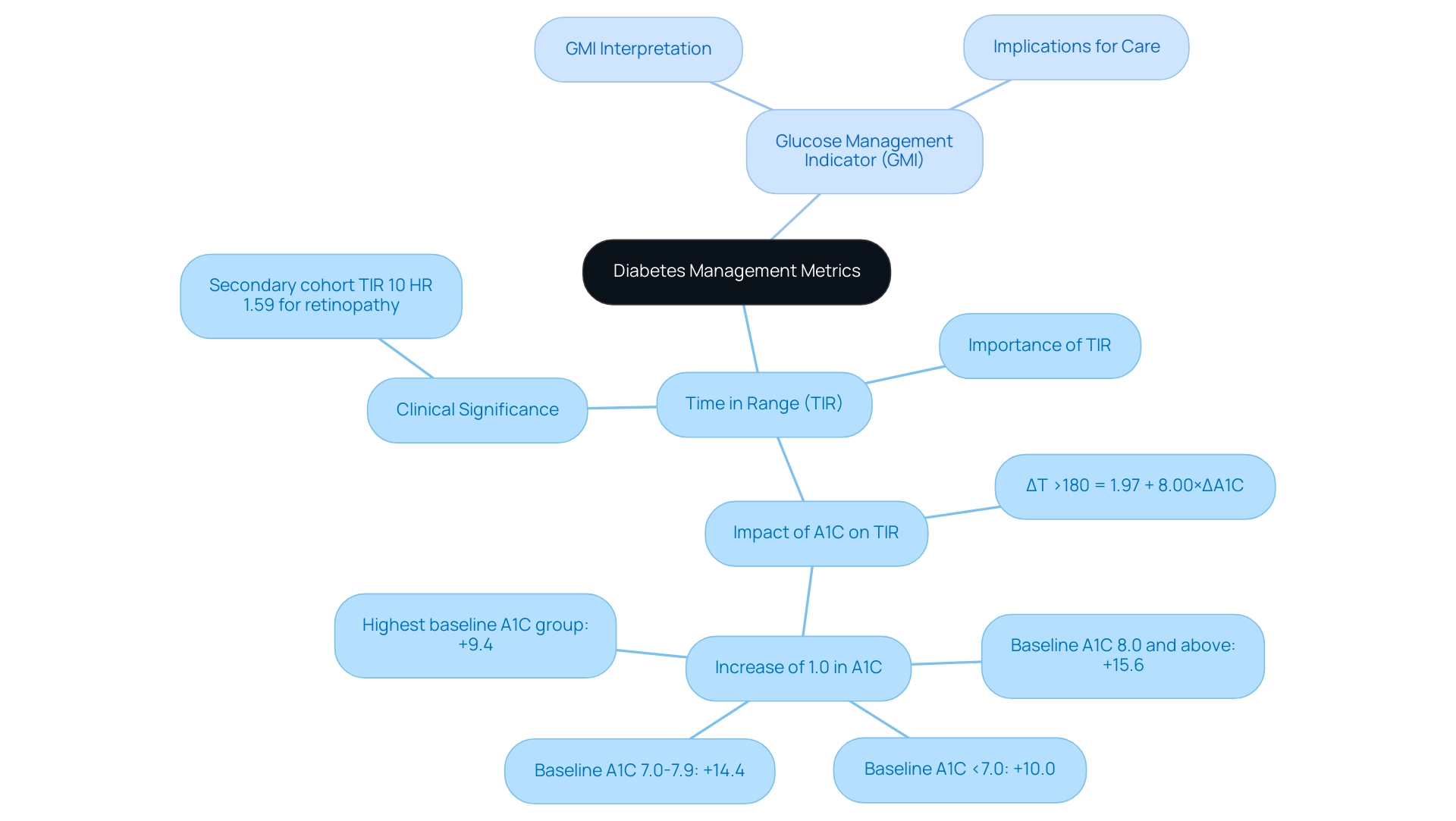
a2d Solutions, we acknowledge that Time in Range (TIR) acts as a crucial metric for assessing the percentage of time an individual's glucose levels stay within a specified target range. Analyzing TIR in conjunction with the Glucose Management Indicator (GMI) helps clarify what is a good GMI percentage, providing a holistic perspective on an individual's glycemic control, which is essential for newly diagnosed individuals seeking effective diabetes management. Our resource hub aims to educate individuals about these metrics, empowering them to understand their health better.
For example, it is possible for an individual to attain a favorable GMI reflecting good average blood sugar levels, yet simultaneously show a low TIR, which leads to the question of what is a good GMI percentage, indicating a pattern of frequent hyperglycemic and hypoglycemic episodes. This dual-metric method, supported by T2DSolutions, encourages a deeper comprehension of condition management, shifting the emphasis beyond simple averages to the significance of reducing sugar fluctuations. Notably, a secondary cohort TIR of 10% has an adjusted hazard ratio (HR) of 1.59 for retinopathy, emphasizing the clinical significance of maintaining TIR.
Furthermore, the equation for estimating change in T >180 based on A1C is:
ΔT >180 = 1.97 + 8.00×ΔA1C
This illustrates how changes in A1C levels impact TIR. The case study titled 'Estimation of Change in T >180 from A1C Change' highlights that an increase of 1.0% in A1C is predicted to increase T >180 by +10.0% for baseline A1C <7.0%, thereby enhancing the practical application of these concepts. By integrating TIR with GMI, healthcare providers can enhance care significantly, especially when considering what is a good GMI percentage, as this combination not only promotes stability in sugar levels but also reduces the risk of complications related to diabetes.
According to Mary L. Johnson, RN, CDE at the International Diabetes Center, recent consensus statements highlight the significance of specific continuous glucose monitoring (CGM) metrics, further underscoring the essential role of TIR in effective management of the condition. At&T Solutions, our dedication is to enable individuals with the information and resources necessary to manage their health journey effectively, offering a thorough resource for their education and assistance.
Evaluating the Accuracy of GMI in Estimating A1C Levels
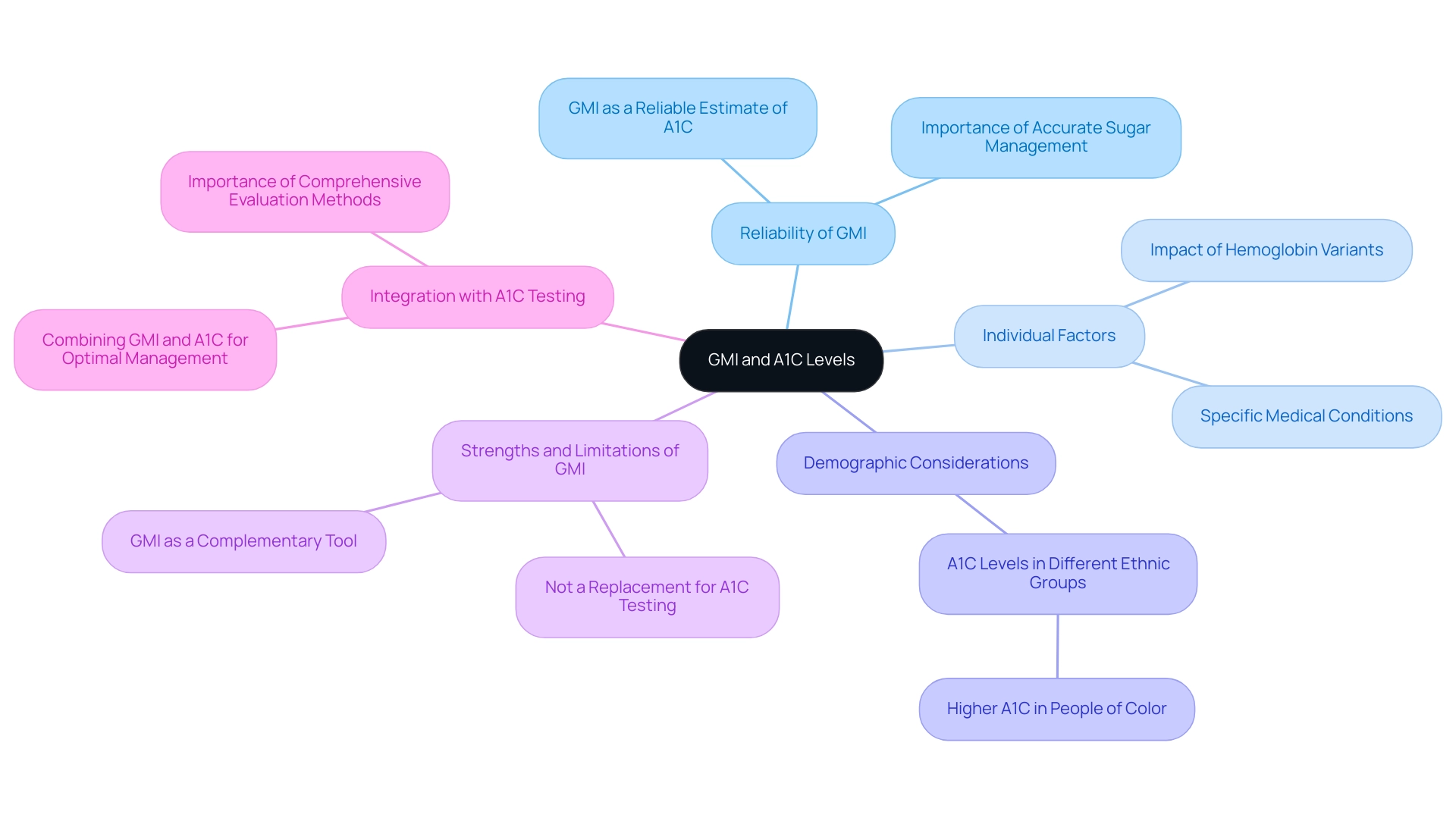
T2DSolutions is committed to offering recently diagnosed individuals extensive resources for comprehending and handling Type 2 and Type 3 conditions. As a new resource hub, T2DSolutions aims to support patients in navigating their condition journey. The reliability of the Glucose Management Indicator (GMI) in estimating A1C levels has raised questions about what is a good GMI percentage within the healthcare community.
Research indicates that GMI can serve as a reliable estimate of A1C levels, which raises the question of what is a good GMI percentage, providing a significant advantage in managing blood sugar. Notably, lowering HbA1c levels has been shown to reduce the risk of major complications, emphasizing the importance of precise sugar management. However, it is essential to acknowledge that individual factors, such as hemoglobin variants and specific medical conditions, can influence the accuracy of GMI readings.
Consequently, while GMI is a valuable tool for approximating A1C, it should not be viewed as a replacement for traditional A1C testing; rather, it is best utilized as a complementary method. Acknowledging the strengths and limitations of GMI is essential for healthcare providers to make informed treatment choices and interact effectively with patients regarding their management strategies. Dr. Diana Isaacs observes that research indicates individuals of color possess marginally elevated average A1C levels compared to white individuals, emphasizing the intricacy of sugar measurement and the necessity for customized strategies in managing blood sugar care.
Furthermore, recent findings indicate that nonglycemic factors can impact HbA1c levels, particularly in the non-diabetic range, underscoring the need for comprehensive evaluation methods. To enhance management of blood sugar levels, it is important to know what is a good GMI percentage in addition to incorporating traditional A1C testing to optimize glucose control and help prevent complications. T2DSolutions aims to be your go-to resource for understanding these metrics and improving diabetes management strategies.
Conclusion
The Glucose Management Indicator (GMI) represents a significant advancement in diabetes management, providing a timely and accurate reflection of a patient's average glucose levels. Its integration with traditional metrics like HbA1c allows for a more comprehensive approach to glycemic control, enabling healthcare providers to tailor treatment plans based on real-time data. This dual-metric strategy not only enhances patient understanding but also empowers individuals to make informed decisions regarding their health.
The relationship between GMI and Time in Range (TIR) further enriches diabetes care by highlighting the importance of maintaining stable glucose levels. This holistic view shifts the focus from averages to the critical need for minimizing fluctuations, thereby reducing the risk of complications associated with diabetes. As evidenced by various studies and case examples, understanding these metrics together can lead to improved health outcomes and a better quality of life for patients.
Ultimately, the incorporation of GMI into diabetes management underscores the necessity for continuous monitoring and personalized care strategies. By leveraging the strengths of both GMI and HbA1c, healthcare providers can ensure that patients receive the most effective interventions tailored to their unique needs. As the landscape of diabetes care continues to evolve, embracing these innovative tools will be vital in the journey towards optimal health and well-being.



