Overview
An ADA meal plan is a structured dietary framework designed to help individuals manage their blood sugar levels through balanced nutrition, including portion control and carbohydrate counting. The article emphasizes that effective implementation of this plan, supported by professional guidance and personalized strategies, can significantly improve glycemic control and overall health outcomes for those managing diabetes.
Introduction
Navigating the complexities of diabetes management requires a strategic approach to dietary choices, particularly through the framework established by the American Diabetes Association (ADA). As T2DSolutions emerges as a pivotal resource for individuals managing Type 2 and Type 3 diabetes, it highlights the significance of structured meal planning.
This article delves into the essential components of ADA meal plans, offering insights into their implementation, common challenges, and the vital role of professional support. By understanding these elements, newly diagnosed patients can empower themselves to make informed decisions that enhance their health and well-being, ultimately transforming their dietary habits into a powerful tool for diabetes management.
Understanding ADA Meal Plans: A Comprehensive Overview
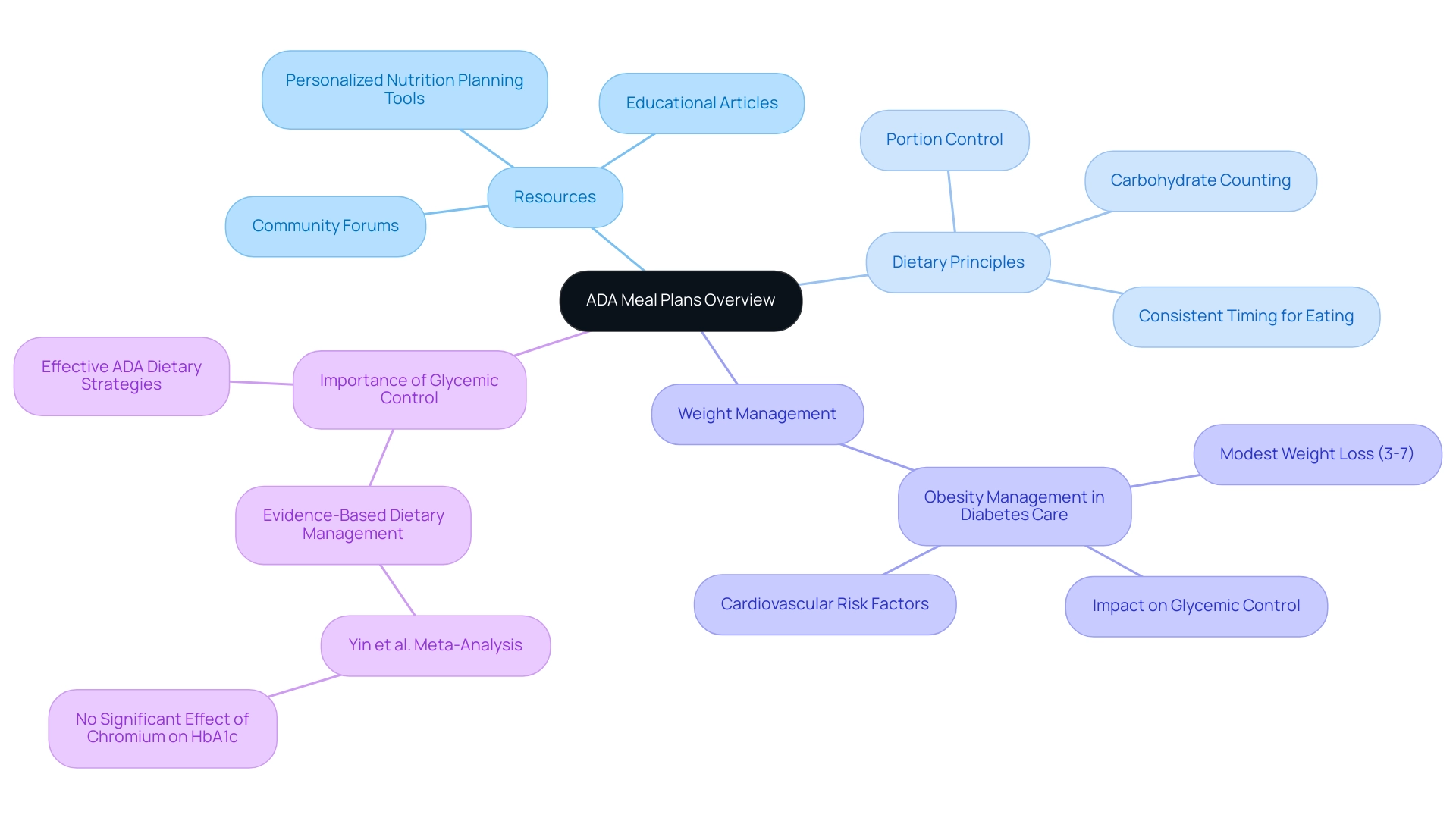
As the organization launches as a comprehensive resource hub for Type 2 and Type 3 blood sugar regulation education and community support, it emphasizes the importance of informed dietary choices. T2DSolutions will provide a variety of resources, including:
- Personalized nutrition planning tools
- Educational articles
- Community forums
All designed to empower individuals managing diabetes. The American Diabetes Association (ADA) meal plan offers a structured framework for these nutritional choices, emphasizing balanced nutrition with principles such as:
- Portion control
- Carbohydrate counting
Alongside the importance of consistent timing for eating.
These personalized meal strategies are designed to reflect individual dietary needs, preferences, and health objectives, empowering patients to make informed choices that support their overall health management. A relevant case study titled 'Obesity Management in Diabetes Care' underscores the critical role of weight management in delaying the progression from prediabetes to type 2 conditions, highlighting that modest weight loss (3-7% of baseline weight) can significantly improve glycemic control and cardiovascular risk factors. This emphasizes the necessity of integrating weight management approaches into dietary strategies for those with blood sugar issues.
Statistics indicate that effective ADA dietary strategies can result in enhanced glycemic control, illustrating that well-organized nutritional selections are essential for managing blood sugar. Additionally, insights from Yin et al. indicate that evidence-based dietary management is essential, as their meta-analysis found no significant effect of chromium supplements on HbA1c levels.
Understanding the components of an ADA meal plan is essential for newly diagnosed patients as they navigate their dietary landscape in pursuit of optimal health management. To stay informed about the latest resources and information from our organization, we encourage you to subscribe for email updates.
Implementing an ADA Meal Plan: Practical Tips for Success
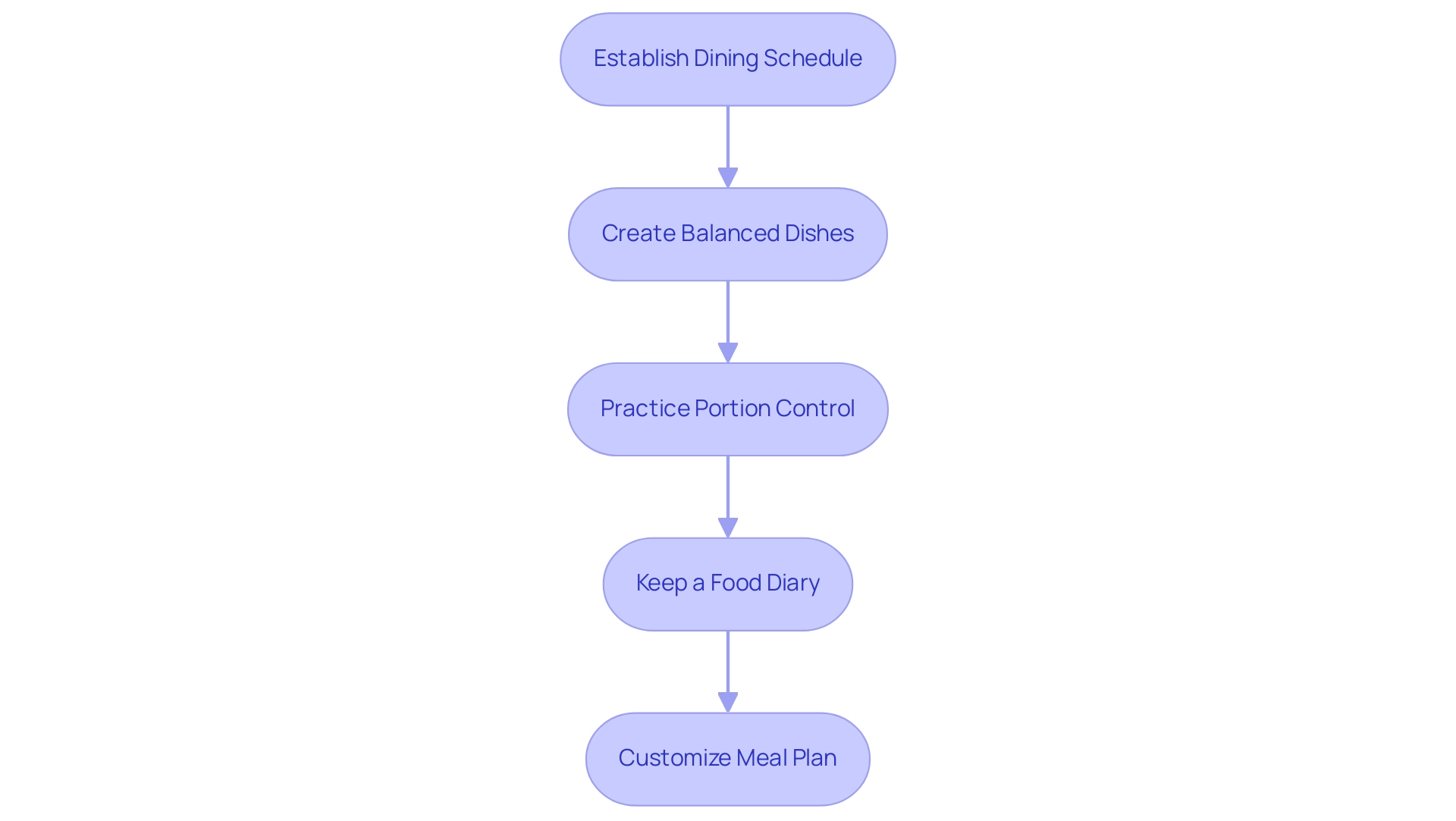
As T2DSolutions launches as a new resource hub for Type 2 and Type 3 glucose intolerance education and community support, we invite you to subscribe for updates on our upcoming resources. Implementing an ADA meal plan requires a series of practical steps designed to improve long-term success. Establishing a consistent dining schedule is paramount, as it aids in regulating blood sugar levels—an essential aspect of diabetes management.
Balanced dishes should include an appropriate ratio of carbohydrates, proteins, and healthy fats. Emphasizing a variety of fruits, vegetables, whole grains, and lean proteins not only enhances nutritional value but also supports overall health. Moreover, portion control is essential for managing caloric intake and preventing blood sugar spikes.
Keeping a food diary can be beneficial for tracking daily food choices and recognizing patterns that might affect glucose levels. Customizing the ADA meal plan to align with personal preferences and lifestyle choices enhances adherence and satisfaction, supporting the maintenance of healthy eating habits over time. T2DSolutions will provide resources and tools to assist newly diagnosed patients in implementing these strategies effectively.
Recent studies have demonstrated that organized weight-loss programs, which offer dietary recommendations and behavioral support, have resulted in significant outcomes, with fat mass accounting for 87% of the total weight lost in the D/HBS cohort at 4 weeks. As noted by David M. Nathan, MD, 'The long-term benefits of the two DPP interventions on disease development... are a testament to the power of these interventions and reinforce their importance in the reduction of this condition.' This highlights the effectiveness of organized dietary schedules across various groups, as demonstrated in the case study on the generalizability of weight-loss program outcomes.
Such interventions emphasize the significance of a well-structured strategy for nutrition planning in attaining optimal management of type 2 diabetes, reinforcing the organization's dedication to assisting newly diagnosed patients on their health journey.
Key Nutritional Components of an ADA Meal Plan
An effective dietary strategy created by the American Diabetes Association (ADA), known as the ada meal plan, includes several essential nutritional elements vital for managing blood sugar, rendering it an invaluable resource as T2DSolutions initiates support for newly diagnosed patients. At the forefront is the focus on carbohydrates, which have a direct impact on blood glucose levels. The ADA advocates for the selection of complex carbohydrates, such as:
- Whole grains
- Legumes
- Colorful vegetables
These are rich in fiber and help to regulate glucose absorption, thereby minimizing spikes in blood sugar.
Furthermore, protein sources—ranging from lean meats and fish to eggs and plant-based alternatives—play a crucial role in muscle maintenance and promoting satiety. The inclusion of healthy fats, particularly from:
- Avocados
- Nuts
- Olive oil
is also encouraged, albeit in moderation, to support cardiovascular health. To complete the dietary strategy, a range of fruits and vegetables are highlighted for their essential vitamins and minerals, ensuring a balanced diet that promotes overall wellness while effectively managing diabetes.
Additionally, according to the Institute of Medicine and the Academy of Nutrition and Dietetics, dietary fat should constitute 20% to 35% of total energy intake, which further guides the composition of a nutritionally sound ada meal plan. For those newly diagnosed, the ADA offers free live cooking classes monthly, which can be a valuable resource for learning healthy meal preparation. Moreover, non-nutritive sweeteners can be considered for those seeking alternatives that do not raise blood glucose levels, but their overall food context must be taken into account.
The Exchange List Approach is another practical method for managing carbohydrate intake, allowing individuals to substitute foods within the same group while maintaining dietary consistency. As the organization evolves, it will keep offering extensive resources and assistance, including educational articles, community forums, and interactive tools for individuals managing their condition. We encourage newly diagnosed patients to subscribe to Td Solutions for updates and access to valuable resources that can aid in their diabetes management.

Common Challenges and Solutions in Following an ADA Meal Plan
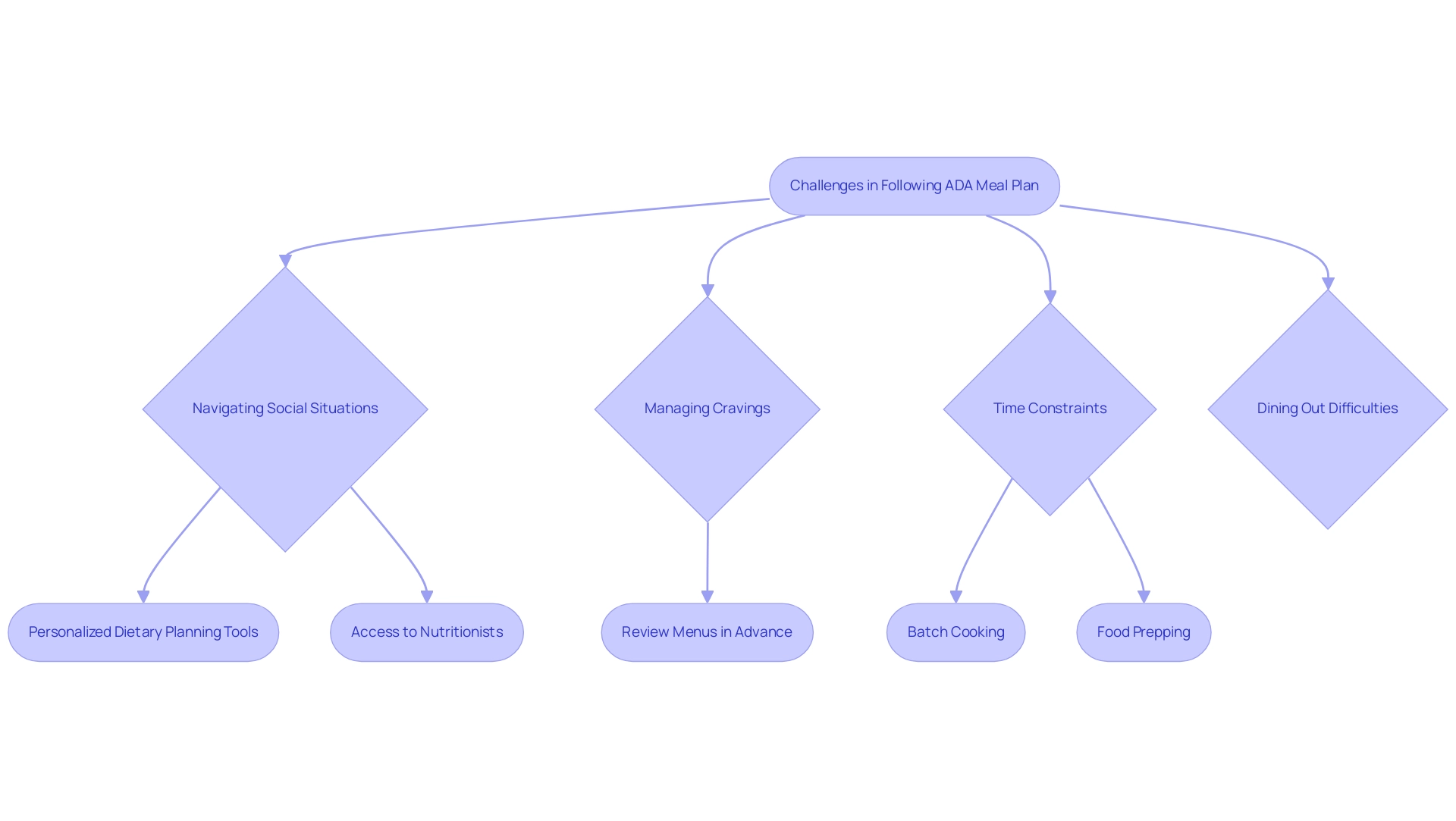
Following an ADA meal plan presents various challenges, such as navigating social situations, managing cravings, and dealing with time constraints. Dining out, in particular, can complicate dietary adherence, as many menu options may not conform to the established guidelines. Statistics show that adherence to these recommendations is only at 46.7% (median 40, IQR 53.3) for the total sample, highlighting the difficulties faced by individuals.
To alleviate this issue, the organization acts as a comprehensive resource center for newly diagnosed patients, providing:
- Personalized dietary planning tools
- Access to nutritionists
- A database of restaurants with healthy options
We encourage individuals to review menus in advance and select restaurants known for offering nutritious options. Furthermore, cravings for high-sugar or high-fat foods often arise, which can hinder compliance.
As researchers point out, 'food insecurity, like poverty, won’t be an easy problem to fix,' emphasizing the broader context of challenges that may affect adherence to dietary guidelines. The company offers tools and strategies for identifying healthier substitutes and allowing for occasional indulgences in moderation. Time constraints can also present significant obstacles in food preparation; however, implementing practices such as:
- Batch cooking
- Food prepping
can streamline efforts during busy periods.
Additionally, the limitations of self-reported data in assessing dietary adherence, as noted in the case study on self-reported dietary adherence limitations, suggest that biases may exist due to participants' potential misreporting. By proactively tackling these challenges and utilizing practical solutions, individuals can improve their capacity to comply with ADA dietary guidelines successfully, backed by the resources available at our organization, including testimonials from users who have successfully managed their nutritional challenges with our assistance.
The Role of Professional Support in Meal Planning
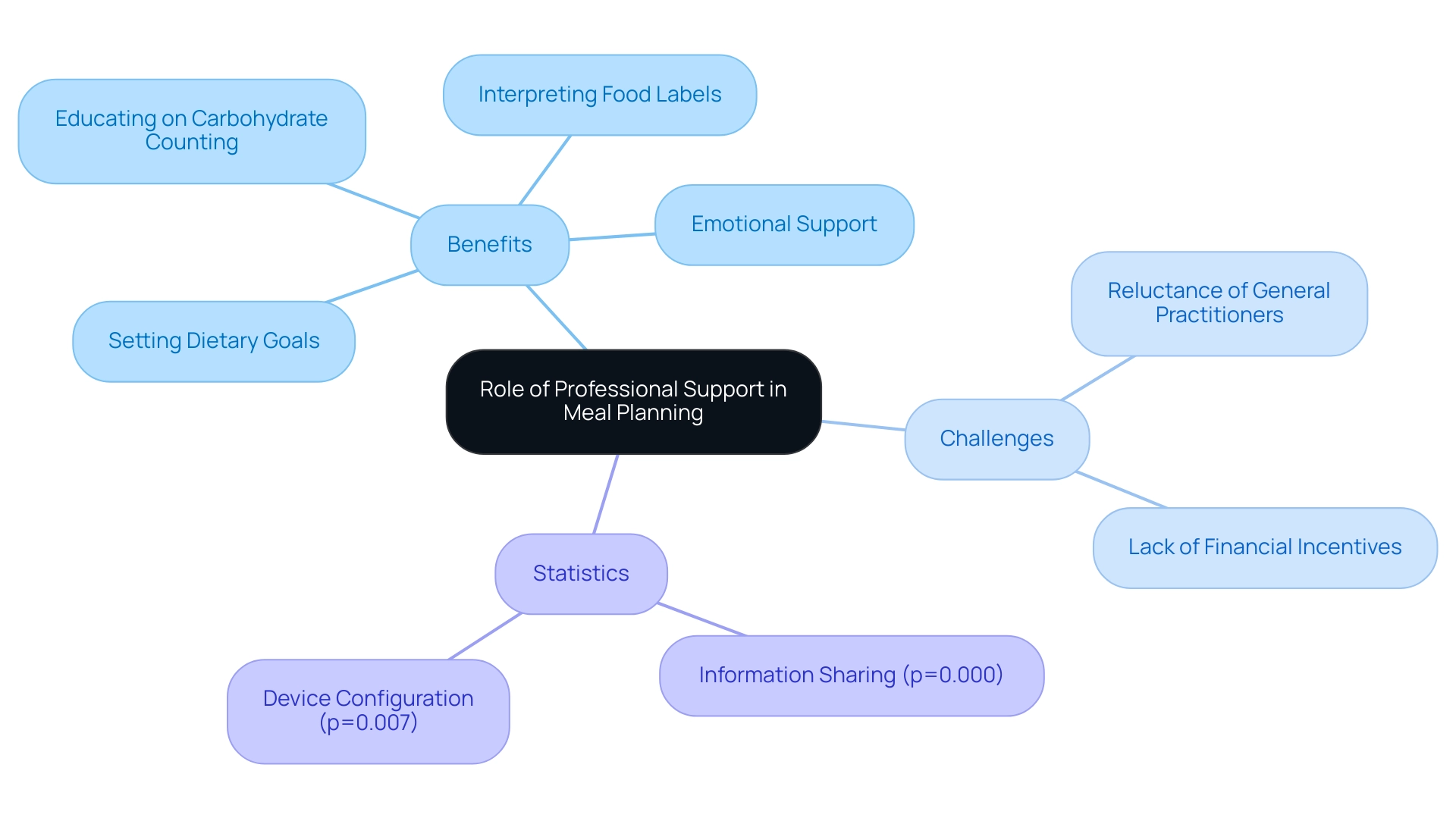
The successful execution of an ADA meal plan greatly benefits from professional assistance, which is essential for individuals managing their blood sugar levels. This organization acts as a valuable resource hub, connecting individuals with Certified Diabetes Educators and registered dietitians who provide personalized guidance tailored to each individual's needs. Their expertise aids in:
- Setting realistic dietary goals
- Educating patients on carbohydrate counting
- Interpreting food labels effectively
Additionally, these professionals play a vital role in offering emotional support, addressing the psychological challenges associated with chronic conditions such as diabetes. T2DSolutions offers tools and resources that facilitate collaboration between healthcare professionals and patients, ensuring that individuals receive comprehensive support. Regular follow-ups with healthcare teams are crucial; they not only help individuals remain accountable but also facilitate necessary adjustments to meal plans as circumstances evolve.
However, the research on collaborative care models in managing diabetes-related issues highlights challenges such as:
- The reluctance of general practitioners to engage with collaborative healthcare professionals in complex cases
- The lack of financial incentives for team-based care
This highlights the necessity for a cultural shift in healthcare practices to embrace collaboration in managing blood sugar conditions. Furthermore, statistical differences in service provision for type 2 mellitus (T2DM) were found among health professionals with varying perceptions on information sharing (p=0.000) and device configuration (p=0.007).
These statistics reinforce the argument for professional guidance in dietary planning, especially when implementing an ADA meal plan, as effective collaboration and communication can lead to better patient outcomes. As one healthcare professional stated, 'We must continuously evaluate how we can run this clinic more efficiently. I am able to perform several tasks simultaneously.'
This quote illustrates the necessity for efficiency in managing diabetes-related care and highlights the critical role healthcare professionals play in supporting patients effectively. By leveraging such professional support through T2DSolutions, individuals can enhance their confidence and competence in managing diabetes through effective meal planning, ultimately improving their overall health outcomes.
Conclusion
Navigating the complexities of diabetes management through structured meal planning is essential for individuals managing Type 2 and Type 3 diabetes. The American Diabetes Association (ADA) meal plans provide a robust framework that prioritizes balanced nutrition, portion control, and carbohydrate counting, all tailored to individual needs and health objectives. As highlighted, incorporating weight management strategies and adhering to these plans can significantly enhance glycemic control and overall health.
Implementing an ADA meal plan involves practical steps such as:
- Establishing a consistent meal schedule
- Emphasizing a variety of nutritious foods
- Personalizing choices to fit individual lifestyles
The importance of maintaining a food diary and recognizing patterns that affect glucose levels cannot be overstated. Moreover, addressing common challenges—such as social dining situations and time constraints—requires proactive strategies that facilitate adherence to dietary guidelines.
Professional support plays a pivotal role in successfully implementing these meal plans. Access to Certified Diabetes Educators and registered dietitians can provide personalized guidance and emotional support, helping individuals set realistic dietary goals and navigate the complexities of food choices. Regular collaboration with healthcare teams ensures that meal plans remain effective and adaptable to changing circumstances.
In conclusion, by leveraging the resources available through T2DSolutions and embracing the structured approach of ADA meal plans, individuals can empower themselves to take control of their diabetes management. This informed dietary strategy not only promotes better health outcomes but also fosters confidence in making wise nutritional choices crucial for long-term wellness.



