Overview
Understanding the CPT code for diabetes is crucial for those navigating the complexities of diabetes-related healthcare. It plays a vital role in accurately billing for services such as consultations, treatments, and continuous glucose monitoring. By grasping these codes, healthcare providers can ensure proper reimbursement, which ultimately enhances the care you receive. This means that every service you need is documented and compensated, leading to better health outcomes as you manage your diabetes.
It's understandable to feel overwhelmed by these details, but know that you are not alone in this journey. We are here to support you every step of the way. By familiarizing yourself with these codes, you empower not only yourself but also your healthcare team to provide the best possible care tailored to your needs. Remember, seeking clarity on these matters is a positive step toward taking control of your health.
Introduction
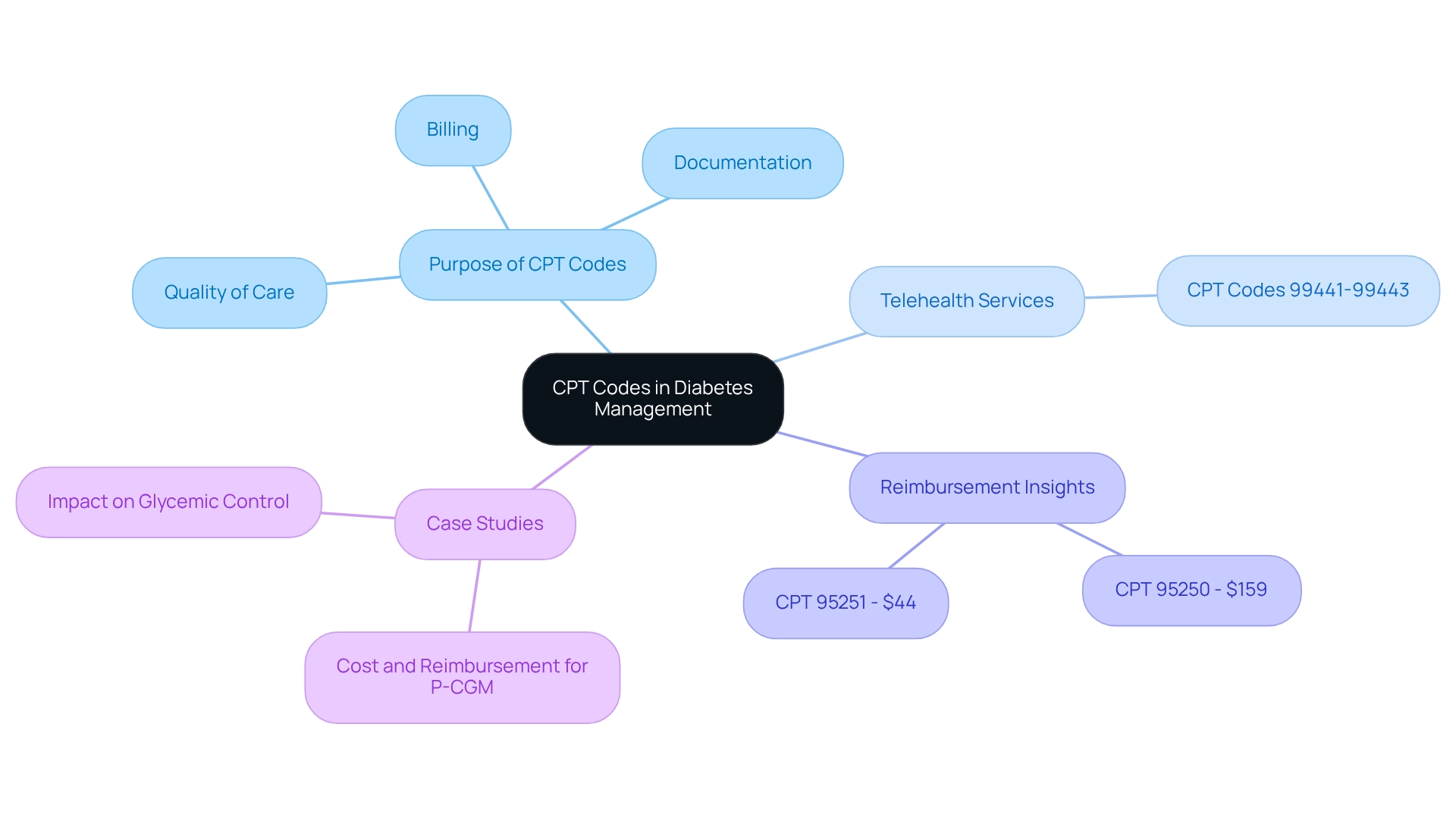
In the intricate world of diabetes management, understanding the role of Current Procedural Terminology (CPT) codes is crucial. These essential codes are the backbone for reporting and billing healthcare services. They ensure that patients receive the comprehensive care they need and that healthcare providers are appropriately reimbursed. As telehealth becomes more prominent and continuous glucose monitoring is integrated into standard care, grasping the nuances of these codes is vital for both providers and patients alike.
It's understandable to feel overwhelmed with all the information surrounding diabetes management. With a focus on accurate documentation and reimbursement practices, this article explores the significance of CPT codes in diabetes management. We will delve into key codes, common challenges, and best practices that can pave the way for improved patient outcomes and streamlined billing processes. Remember, you're not alone in this journey; we are here to support you every step of the way.
Introduction to CPT Codes in Diabetes Management
Understanding the CPT code for diabetes is crucial for effectively managing your health. This medical identifier, part of the Current Procedural Terminology (CPT), is essential for reporting and billing healthcare services, especially in diabetes management. By grasping these identifiers, you can ensure that all services provided—like consultations, evaluations, and treatments—are accurately documented. This clarity is vital for healthcare providers to secure the appropriate reimbursements from insurance companies, which can directly impact your care.
For example, codes like 99441-99443 are designated for telehealth services related to glucose management. This highlights how important classification has become in modern diabetes treatment. When used effectively, the CPT code for diabetes not only facilitates proper billing but also enhances the overall quality of care. It ensures that every service rendered is accounted for and reimbursed, allowing you to receive the support you need.
Did you know that over 93% of private payers in the United States have established medical policies for professional continuous glucose monitoring (P-CGM)? This statistic underscores the growing recognition of these services in managing blood sugar conditions. Incorporating P-CGM devices into primary care is expected to improve glycemic control and reduce complications, further emphasizing the need for accurate coding.
Moreover, case studies reveal that the average Medicare reimbursement for CPT 95250, which covers the placement and training for P-CGM, is around $159. In contrast, CPT 95251, related to data interpretation, averages $44. This financial aspect highlights how the CPT code for diabetes significantly influences the economics of diabetes management, affecting both providers and patients like you.
M.S., a key contributor to this work, emphasizes the importance of the CPT code for diabetes, stating, 'CPT classifications not only simplify billing procedures but also improve engagement and satisfaction among individuals.' As healthcare evolves, the role of these classifications in effectively managing blood sugar conditions remains vital, ensuring you receive the comprehensive support necessary for optimal health outcomes.
At T2DSolutions, we are dedicated to helping newly diagnosed patients understand the importance of the CPT code for diabetes and its role in managing your condition effectively. As a resource center for education and community support related to blood sugar management, we are here to assist you in navigating the complexities of billing and reimbursement processes. You're not alone in this journey; we encourage you to explore T2 Solutions for more information on blood sugar management and the support resources available to you.
Key CPT Codes for Diabetes Services
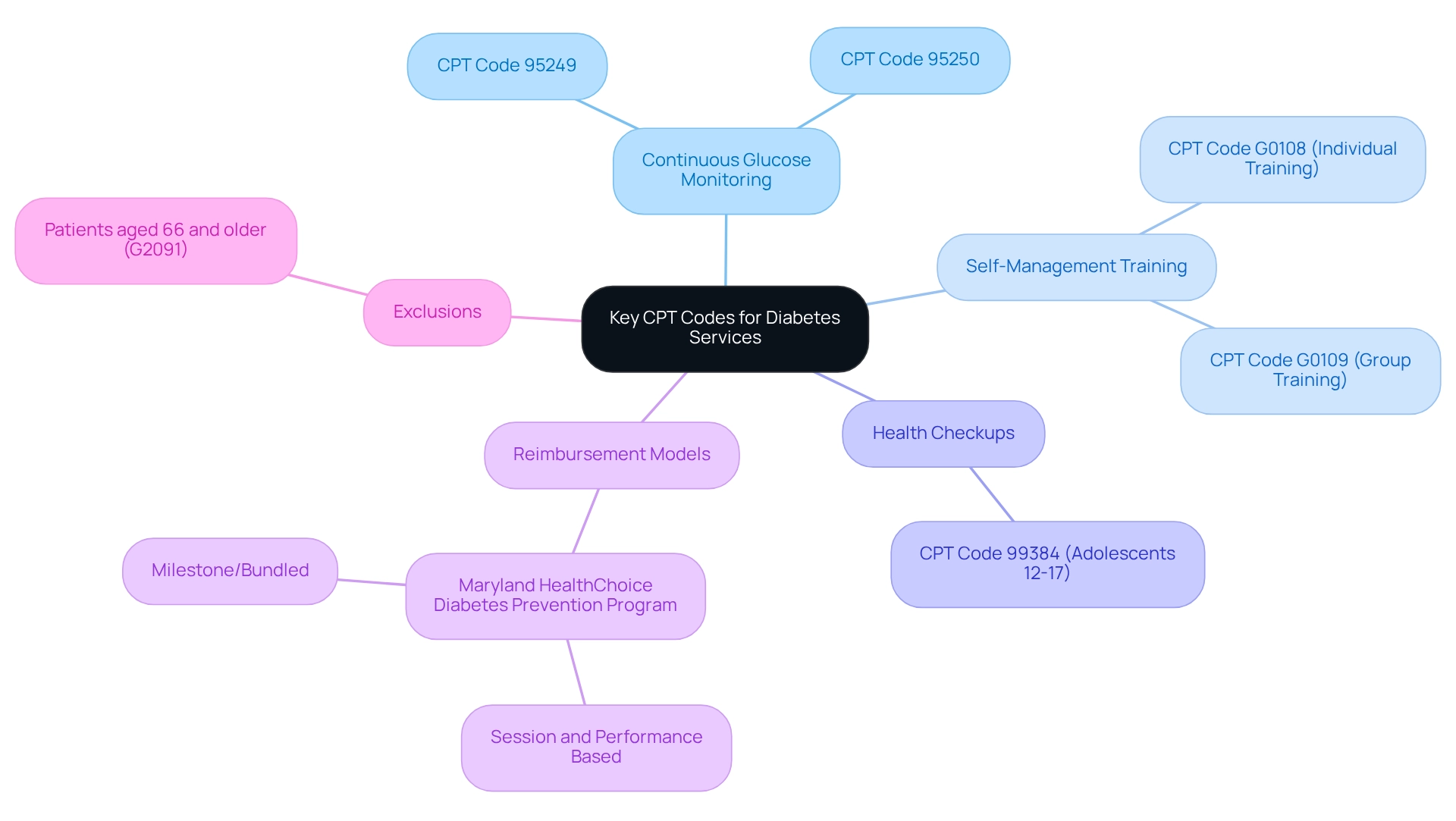
When it comes to managing blood sugar conditions, understanding important CPT codes for diabetes is crucial. These codes help healthcare providers effectively bill for their services, ensuring that you receive the care you need. For instance, CPT designation 95249 is assigned for the initial placement of a continuous glucose monitor (CGM), which plays a vital role in real-time glucose tracking. Following that, CPT number 95250 covers the education associated with using CGMs, empowering you to manage your condition confidently.
Additionally, codes like G0108 and G0109 are specifically designated for diabetes self-management training (DSMT). G0108 pertains to individual training sessions, while G0109 addresses group sessions, providing flexibility in how you receive education and support. Knowing these identifiers is essential for healthcare practitioners, as it allows them to accurately charge for services, helping to minimize financial barriers for patients seeking necessary treatment.
Moreover, CPT Code 99384 relates to health checkups for teenagers aged 12 to 17, highlighting the broader classification framework that impacts blood sugar management across different age groups. The significance of these CPT designations extends beyond billing; they are fundamental to the overall management of blood sugar conditions. For example, the Maryland HealthChoice Diabetes Prevention Program has successfully implemented reimbursement models that encourage participation in the National Diabetes Prevention Program (DPP).
This initiative underscores the importance of adaptable payment frameworks in fostering better health outcomes for participants. It shows how effective coding and billing methods can lead to increased engagement and care.
As we look ahead to 2025, the landscape of services for managing blood sugar conditions continues to evolve, particularly with a focus on the CPT code for diabetes. Statistics indicate that reimbursement rates for self-management training related to blood sugar conditions are vital for ensuring that you receive the education necessary to manage your health effectively. It’s important to note that individuals aged 66 and older with claims for frailty and advanced illness diagnosis (G2091) are excluded, providing context on the demographics relevant to managing blood sugar conditions.
By staying informed about these essential regulations and their implications, healthcare providers can better support you in navigating the complexities of managing blood sugar, especially with the use of the CPT code for diabetes.
As T2DSolutions launches as a new resource hub for education and community support regarding blood sugar conditions, it aims to provide valuable information on these CPT codes and their relevance to management. This resource is designed to empower newly diagnosed patients like you with the knowledge needed to understand treatment options and navigate the healthcare system effectively. In the words of Sharon Hollander, "Unlock the secrets to efficient wound care billing with proven strategies that boost reimbursement. Learn how to streamline your billing process, avoid common errors, and maximize your practice’s revenue with expert insights." This highlights the importance of understanding billing practices in managing diabetes-related conditions. You're not alone in this journey, and we are here to support you every step of the way.
Reimbursement and Billing for Diabetes CPT Codes
Understanding the precise use of the CPT code for diabetes is crucial for ensuring proper reimbursement for diabetes services. Insurance firms and Medicare have established specific guidelines that determine which identifiers qualify for reimbursement and the related payment rates. For example, compensation for Diabetes Self-Management Training (DSMT) services relies heavily on careful documentation and the correct application of the CPT code for diabetes.
As a provider, it’s important to be aware of the reimbursement rates tied to each classification and the necessary documentation to avoid claim denials. This knowledge can significantly impact your practice and the care you provide.
Looking ahead to 2025, we anticipate that reimbursement rates for diabetes-related CPT classifications will reflect ongoing adjustments in healthcare policies. This highlights the need for providers to stay updated on these changes. The conversion factor for CY 2022 is $34.6062, offering a concrete financial context for understanding reimbursement rates. Additionally, the introduction of session and performance-based reimbursement methodologies, as demonstrated in the Maryland HealthChoice Diabetes Prevention Program, has effectively encouraged participation in lifestyle change programs, leading to improved health outcomes for participants.
This case analysis illustrates how effective reimbursement strategies can enhance participation in management programs for blood sugar conditions. Moreover, the impact of CPT documentation on reimbursement for related services is significant. Proper programming is essential for ensuring that services are adequately reimbursed, as emphasized by healthcare billing experts who stress that precise classification directly influences the financial viability of practices.
As the landscape of managing blood sugar conditions evolves, grasping reimbursement guidelines for the CPT code for diabetes will be vital for providers aiming to navigate the complexities of insurance reimbursement effectively.
It’s also essential to establish negotiated rates for services between CDC-recognized organizations and commercial plans, as this collaboration is key to optimizing reimbursement strategies. In light of recent developments, including coding and billing for the Medicare Diabetes Prevention Program (MDPP) using CMS Calendar Year MDPP Payment Rates and associated HCPCS G-codes, healthcare providers must familiarize themselves with the latest reimbursement guidelines for the CPT code for diabetes related to blood sugar management in 2025. This understanding not only aids in securing necessary funding for diabetes-related services but also ensures that individuals receive the comprehensive care they need.
By addressing reimbursement challenges and employing effective strategies, providers can enhance access to management resources for blood sugar control, ultimately improving patient outcomes.
Furthermore, standardized, single-page glucose reports from continuous glucose monitoring (CGM) devices, as suggested by the American Diabetes Association, should be viewed as a standard summary for all CGM devices. This expert insight underscores the importance of accurate documentation in managing diabetes-related care and reimbursement. Remember, you’re not alone in this journey; we are here to support you every step of the way.
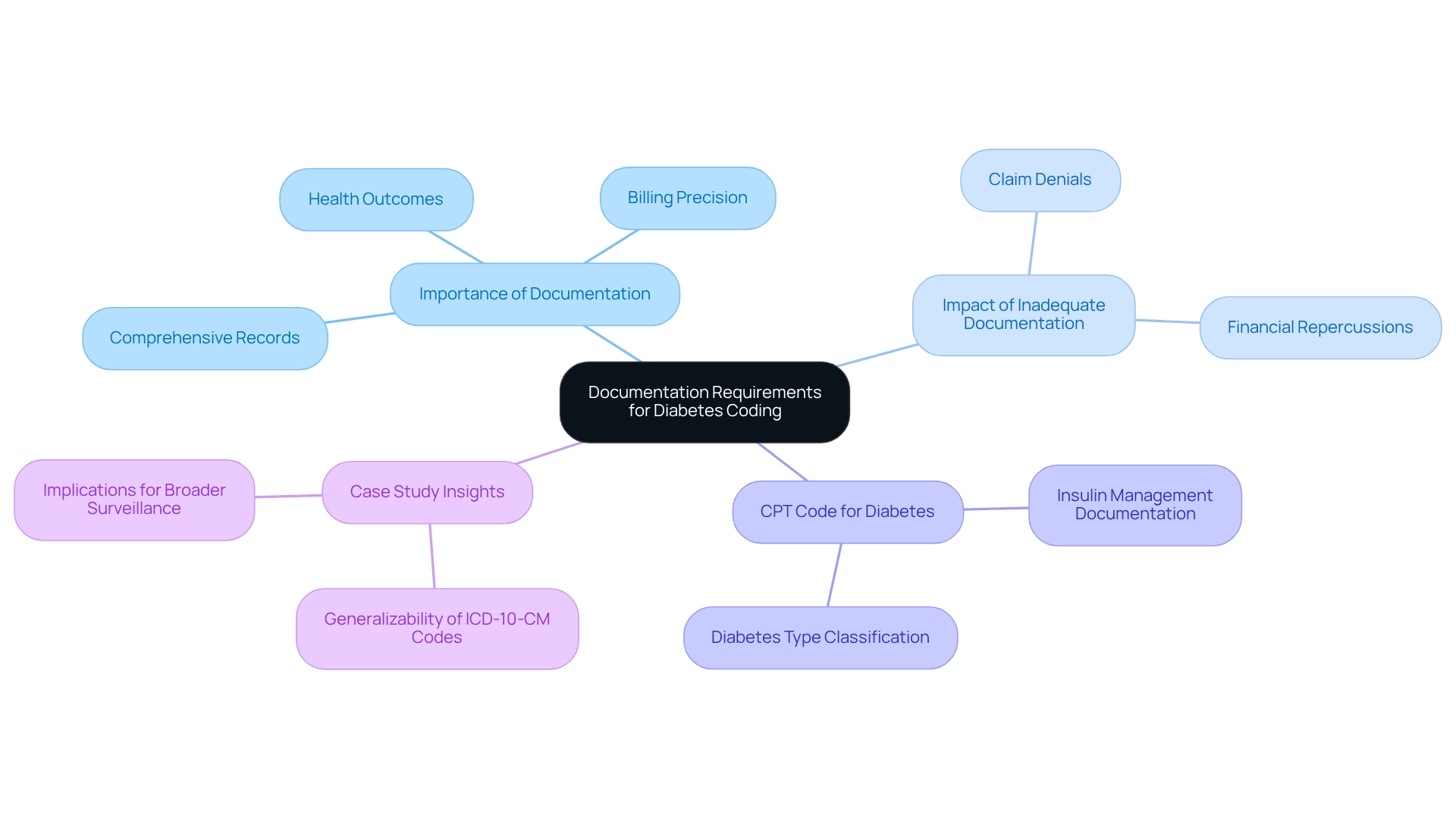
Documentation Requirements for Diabetes Coding
Effective diabetes coding is rooted in meticulous documentation, which forms the foundation for justifying the CPT code for diabetes. It's essential for healthcare providers to maintain comprehensive records that reflect client diagnoses, treatment plans, and all services rendered. For instance, when billing for insulin management, it’s crucial to clearly document the individual's insulin regimen and any related complications.
A recent study revealed that 93.2% of individuals with Type 2 Diabetes Mellitus (T2DM) were classified as overweight or obese. This statistic underscores the importance of precise documentation that accurately reflects each individual's health status and treatment needs.
Inadequate documentation can lead to claim denials and significant financial repercussions for healthcare providers. Therefore, implementing systematic documentation practices is vital for ensuring compliance and effectively supporting billing processes, particularly concerning the CPT code for diabetes. A case study on the generalizability of ICD-10-CM codes for diabetes surveillance highlighted the critical nature of accurate diabetes type classification, which is essential for effective management and billing.
The results suggested that while these findings are strong within a particular healthcare system, caution is necessary when applying them in different contexts due to variations in documentation practices and the demographics of individuals.
Moreover, professional insights emphasize that comprehensive documentation is not just a regulatory necessity but also a best practice that enhances care quality. Kay Piper, a HIM coding specialist, states, "Uncover critical guidance" regarding the significance of documentation in billing for diabetes-related conditions. By thoroughly recording all pertinent information, including the CPT code for diabetes, providers can enhance their billing precision and ultimately contribute to improved health outcomes for those they serve.
As the landscape of blood sugar management continues to evolve, staying informed about documentation requirements and common billing errors will be essential for healthcare professionals in 2025 and beyond. This thorough approach not only assists healthcare professionals but also ensures that newly diagnosed individuals receive the appropriate care and resources they need for effective management of their condition. You're not alone in this journey; we are here to support you every step of the way.
Common Challenges in Diabetes Billing and Coding
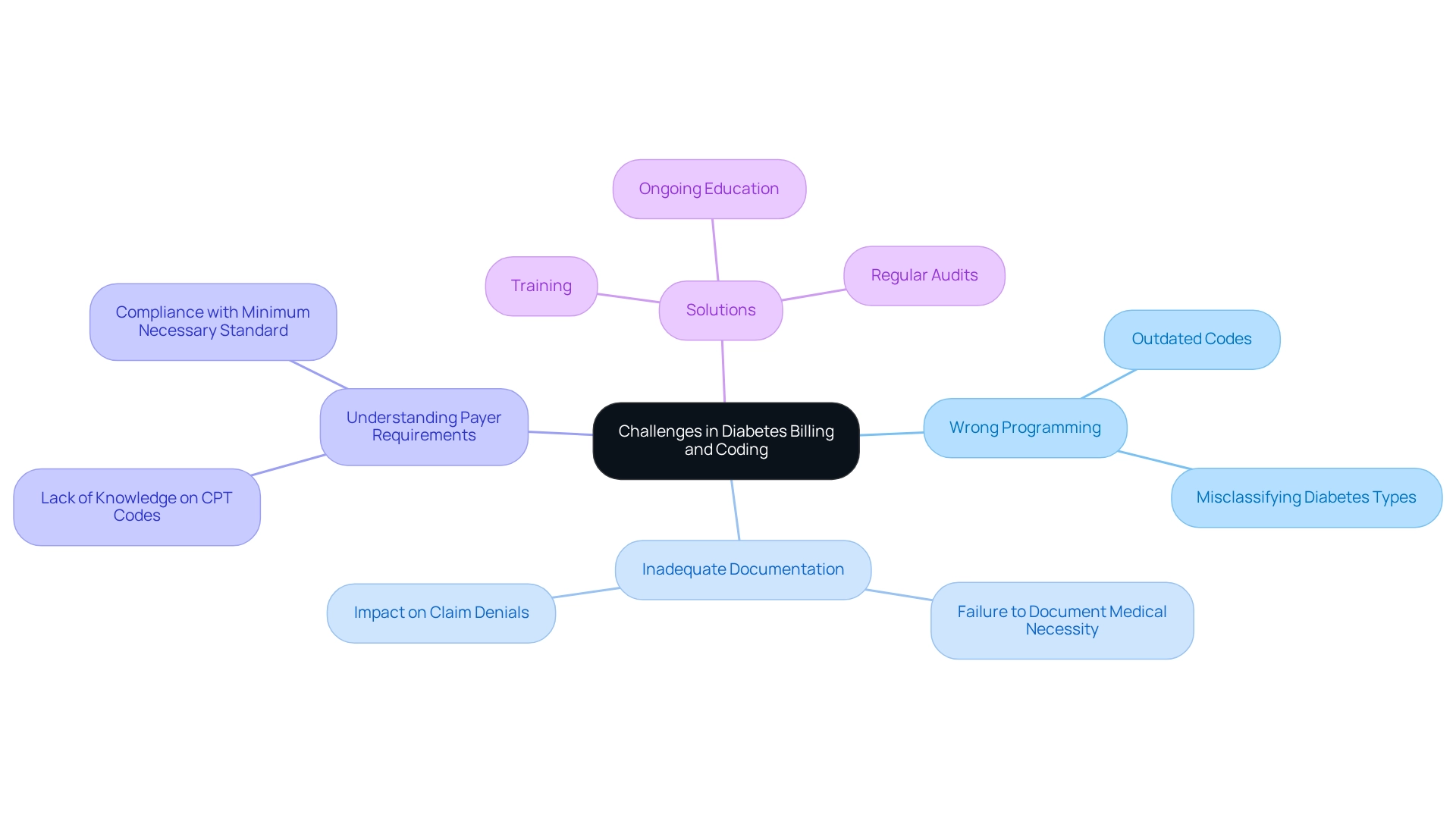
Billing and coding for diabetes services, including the cpt code for diabetes, can be quite challenging. These challenges can significantly affect both patient care and healthcare provider operations. Many providers face common issues, such as:
- Selecting the wrong programming
- Inadequate documentation
- A lack of understanding of payer requirements regarding the cpt code for diabetes
It's understandable to feel overwhelmed; for instance, providers may accidentally use outdated codes or forget to document the medical necessity of services. This can lead to claim denials and financial losses, which adds to the stress of managing diabetes.
As Steve Alder, editor-in-chief of The HIPAA Journal, points out, the minimum necessary standard requires that only the least required information is used or disclosed. This includes the accurate documentation of the cpt code for diabetes, which is crucial for effective care.
Managing diabetes is often complicated by various comorbidities, making documentation efforts even more challenging. A recent study evaluated the accuracy of International Classification of Diseases (ICD) classifications in administrative databases among confirmed NAFLD individuals in Calgary, Alberta, Canada. This study highlights the importance of precise classifications to effectively represent care dynamics. Additionally, a case study titled 'Healthcare Utilization Patterns in Diabetes Patients' revealed that patients who meet their glycemic targets have different visitation patterns compared to those who do not. This emphasizes how critical precise classification is in understanding and enhancing healthcare strategies.
Statistics indicate that five years is clinically valid for recognizing the onset of diabetes, yet the accuracy of classification remains a persistent issue. Consistent training and audits are essential for healthcare providers to improve documentation accuracy and adhere to current guidelines, especially those related to the cpt code for diabetes. Participating in ongoing education can help reduce common programming mistakes, such as misclassifying diabetes types or overlooking related conditions.
Expert insights suggest that addressing these challenges requires a proactive approach. Staying informed about the cpt code for diabetes, programming changes, and payer policies is vital. By fostering a culture of precision and responsibility in programming practices, healthcare providers can improve their billing processes and ultimately enhance patient outcomes. Remember, you're not alone in this journey—we are here to support you every step of the way.
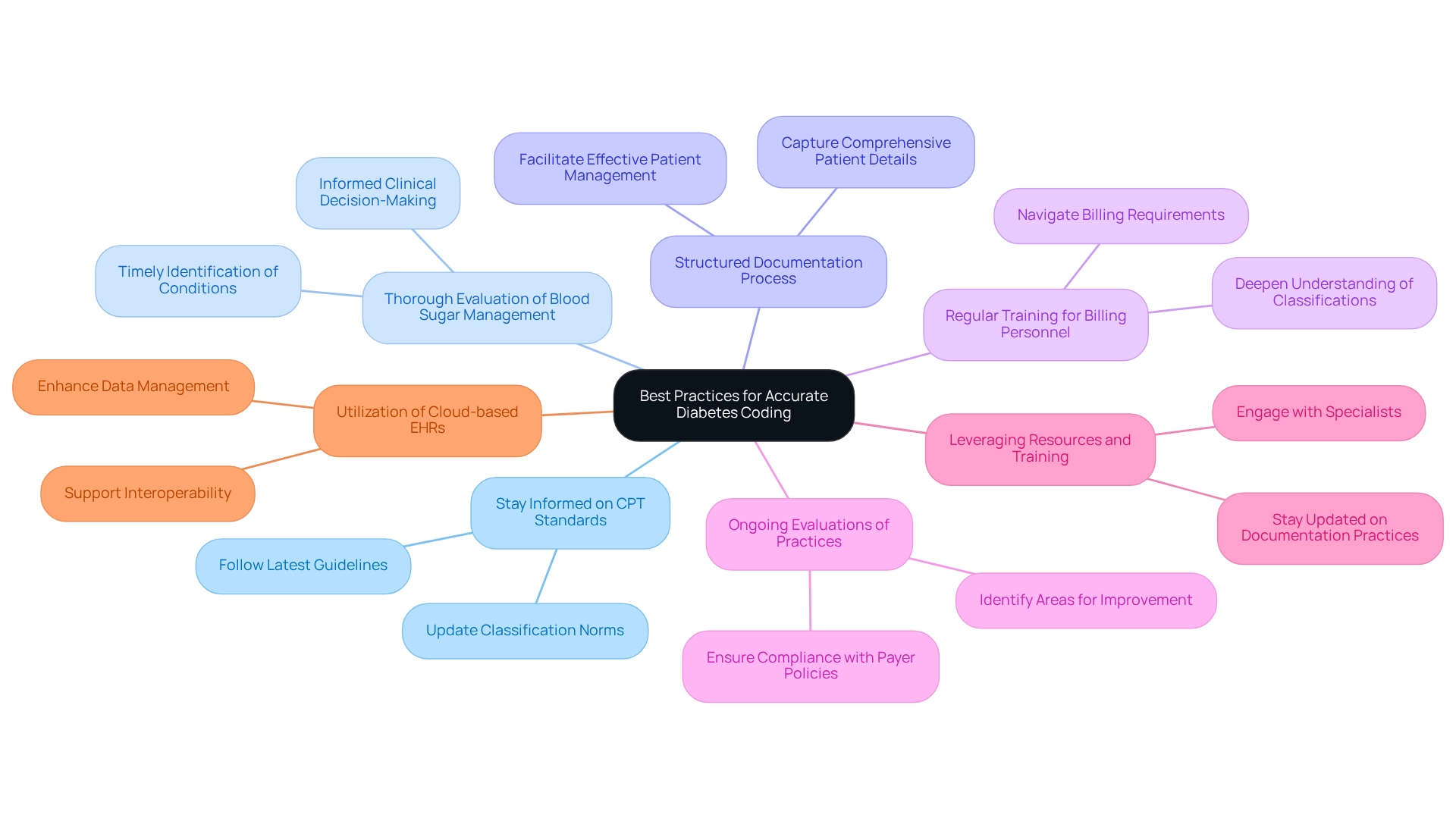
Best Practices for Accurate Diabetes Coding
To achieve precise health condition classification, healthcare providers must embrace several best practices. Staying informed about the latest CPT standards and guidelines, especially regarding the CPT code for diabetes, is essential. It's important to recognize that classification norms are often updated. A thorough evaluation of blood sugar management strategies is vital for the timely identification of conditions and informed clinical decision-making. This proactive approach can significantly reduce errors and enhance classification accuracy.
A structured documentation process that captures comprehensive patient details is equally crucial.
Regular training sessions for billing personnel are important, as they deepen understanding of related classifications and billing requirements, including the CPT code for diabetes. This ensures that staff are well-equipped to navigate the complexities of managing blood sugar conditions. Ongoing evaluations of programming practices are necessary; these assessments help identify areas for improvement and ensure compliance with payer policies. For instance, a pilot study at Stanford School of Medicine demonstrated that integrating a wearable glucose monitor with electronic health records improved provider workflow and communication, ultimately enhancing care quality for patients with diabetes-related conditions.
Such case studies highlight the importance of accurate documentation in facilitating effective patient management.
Moreover, expert recommendations suggest that healthcare providers should leverage available resources and training programs to stay updated on documentation practices. Engaging with specialists in programming can provide valuable insights into maintaining accuracy and compliance in diabetes classification. As William Hoyos emphasized, collaboration among professionals is essential for refining practices.
Additionally, the emergence of cloud-based EHRs presents potential solutions for interoperability and data management, further supporting precise classification. By adopting these best practices, healthcare providers can ensure that their documentation processes are not only accurate but also aligned with the latest industry standards. This commitment ultimately leads to improved patient outcomes, reminding us that you're not alone in this journey—we are here to support you every step of the way.
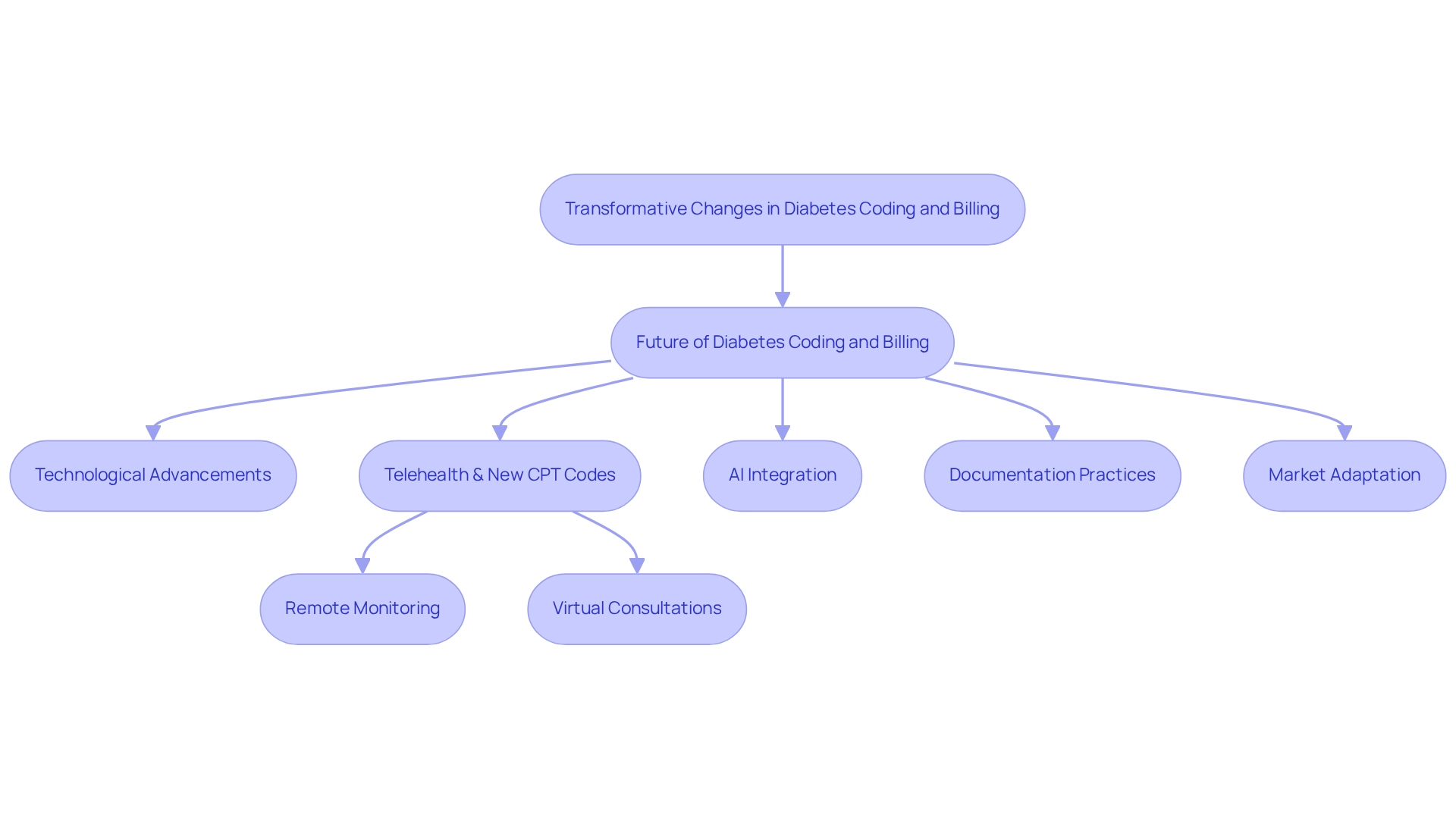
The Future of Diabetes Coding and Billing
The landscape of diabetes classification and billing is on the brink of significant transformation, driven by technological advancements and evolving healthcare delivery models. Digital transformation is not just a project; it’s a continuous process of adaptation and innovation. This is crucial as the rise of telehealth leads to the emergence of new CPT codes for diabetes, specifically designed to facilitate remote monitoring and virtual consultations. This change not only improves patient access to care but also requires a reassessment of documentation practices to ensure they accurately represent these innovative service delivery methods.
Moreover, the integration of artificial intelligence into programming processes is poised to streamline billing operations, minimizing errors and improving efficiency. As blood sugar control management progresses with the introduction of innovative treatment alternatives, documentation practices must adjust accordingly to capture these advancements accurately. Industry leaders emphasize the importance of staying abreast of these trends, as they will be crucial for healthcare providers aiming to maintain compliance and optimize reimbursement strategies in the coming years.
The ongoing conversations regarding consumerism in healthcare have gathered speed, especially in the past two years. This emphasizes the necessity for flexible documentation practices that correspond with patient-centered care. It’s understandable to feel overwhelmed by these changes, but know that support is available.
As we approach 2025, specialist forecasts indicate that the future of managing diabetes-related billing will increasingly depend on technology-driven solutions, particularly regarding the CPT code for diabetes. This includes advancements in billing practices that leverage data analytics to enhance accuracy and efficiency. By adopting these changes, healthcare providers can more effectively manage the intricacies of blood sugar control and ensure that they are prepared to address the requirements of those they serve.
As James Bilefield aptly stated, "When a snake sheds its skin, it changes; when a caterpillar becomes a butterfly, it transforms," underscoring the profound changes in blood sugar management and classification. You’re not alone in navigating these transitions; many are experiencing similar journeys.
Additionally, the case study titled 'Market Adaptation' illustrates how entrepreneurs often start with a B2C approach but may find that a B2B2C model is more effective for reaching a larger audience. Understanding market dynamics and adapting business strategies accordingly can lead to increased patient and provider engagement. Furthermore, as the integration of AI systems scales, attention to deployment modalities, regulatory systems, and ongoing monitoring for risks and adverse events will be essential to ensure the effectiveness of these innovations in diabetes coding. We are here to support you every step of the way as these changes unfold.
Conclusion
Understanding the importance of Current Procedural Terminology (CPT) codes in diabetes management is essential for both healthcare providers and patients. These codes play a critical role in accurate billing and reimbursement, which ultimately impacts the quality of care patients receive. From specific codes related to continuous glucose monitoring to the reimbursement challenges faced by providers, it's clear that meticulous documentation and coding practices are foundational to effective diabetes management.
As we explore best practices, common challenges, and future trends, we see an evolving landscape of diabetes coding and billing. It's understandable to feel overwhelmed by these changes. However, as telehealth and technology continue to reshape our healthcare environment, staying informed about coding updates and reimbursement strategies will be vital for providers. This knowledge can help optimize patient outcomes. The integration of innovative solutions, such as artificial intelligence, further underscores the necessity for adaptive coding practices in response to the dynamic needs of diabetes care.
In conclusion, having a comprehensive understanding of CPT codes, along with effective documentation and proactive engagement with coding changes, can significantly enhance the diabetes management experience for both patients and providers. You're not alone in this journey. By prioritizing these practices, the healthcare community can ensure that individuals living with diabetes receive the support and resources necessary for optimal health outcomes. Together, we can pave the way for a more effective and patient-centered approach to diabetes care.
Frequently Asked Questions
Why is understanding the CPT code for diabetes important?
Understanding the CPT code for diabetes is crucial for effectively managing health, as it helps in reporting and billing healthcare services, ensuring accurate documentation of consultations, evaluations, and treatments.
How do CPT codes impact diabetes management?
CPT codes facilitate proper billing and enhance the quality of care by ensuring that all services rendered are accounted for and reimbursed, which directly affects patient care and provider reimbursements.
What are some examples of CPT codes related to diabetes?
Examples include codes 99441-99443 for telehealth services related to glucose management, CPT 95249 for the initial placement of a continuous glucose monitor (CGM), and G0108 and G0109 for diabetes self-management training (DSMT).
What is the average reimbursement for CPT 95250 and CPT 95251?
The average Medicare reimbursement for CPT 95250, which covers the placement and training for P-CGM, is around $159, while CPT 95251, related to data interpretation, averages $44.
How do CPT codes influence the economics of diabetes management?
CPT codes significantly influence the economics of diabetes management by affecting reimbursement rates for services, which in turn impacts both healthcare providers and patients.
What role does T2DSolutions play in helping patients understand CPT codes?
T2DSolutions is dedicated to helping newly diagnosed patients understand the importance of CPT codes for diabetes and their role in managing the condition effectively, providing education and community support.
What is the significance of continuous glucose monitoring (CGM) in diabetes management?
Continuous glucose monitoring (CGM) is recognized for improving glycemic control and reducing complications, highlighting the importance of accurate coding for these services.
What should patients know about diabetes self-management training (DSMT) codes?
Patients should know that G0108 pertains to individual training sessions and G0109 addresses group sessions for diabetes self-management training, providing flexibility in how they receive education and support.
