Overview:
The Glucose Management Indicator (GMI) is a crucial metric derived from continuous glucose monitoring (CGM) data that estimates an individual's average blood sugar levels, providing a dynamic alternative to traditional A1C tests. The article supports this by detailing how GMI enhances diabetes management through better insights into glucose patterns, improved patient-provider communication, and the potential for timely treatment adjustments, despite acknowledging its limitations in accessibility and data variability.
Introduction
The Glucose Management Indicator (GMI) is revolutionizing diabetes care by providing a dynamic assessment of glucose levels through continuous glucose monitoring (CGM) data. This innovative metric not only offers an alternative to traditional A1C testing but also facilitates a more nuanced understanding of daily glucose fluctuations.
As healthcare providers increasingly recognize the importance of GMI in managing diabetes, recent studies highlight its role in improving patient outcomes and fostering better communication between patients and their care teams.
With the launch of T2DSolutions as a dedicated resource for diabetes education, understanding GMI is more critical than ever for those navigating their treatment options.
This article delves into the significance of GMI, its advantages, limitations, and its potential to empower patients in their diabetes management journey.
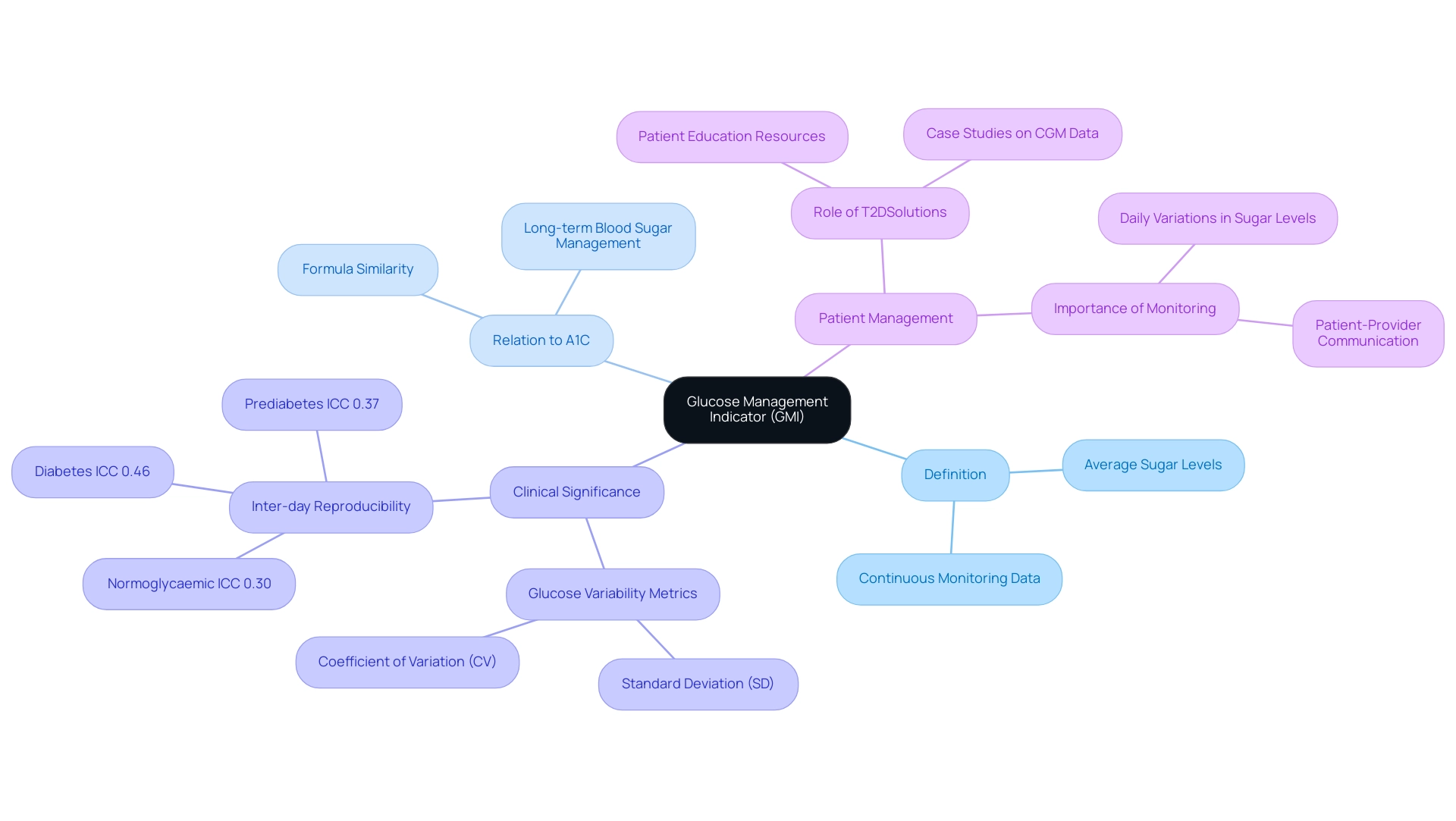
Understanding the Glucose Management Indicator (GMI)
What is GMI? The Glucose Management Indicator is an essential metric obtained from continuous monitoring (CGM) data, offering an estimate of an individual's average sugar levels over a specified duration. GMI is determined through a formula that closely matches the conventional A1C test, commonly employed to assess long-term blood sugar management in individuals with blood sugar issues. This correlation allows healthcare providers and patients to interpret GMI results in a familiar context.
Significantly, GMI acts as a crucial instrument for efficient management of blood sugar levels, providing insights into daily variations that can greatly affect treatment choices. Recent studies emphasize what is GMI in clinical practice, as it highlights its role in monitoring average blood sugar levels and facilitating better patient-provider communication. For instance, the inter-day reproducibility of CGM measurements shows an ICC of 0.46 (95% CI 0.39–0.55) for individuals with the condition, indicating a moderate level of reliability.
Fernando Ovalle, M.D., director of the UAB Multidisciplinary Comprehensive Diabetes Clinic, emphasizes, 'It was Type 1,' highlighting the significance of precise sugar level monitoring in managing the condition. As T2DSolutions launches as a new resource hub for Type 2 and Type 3 diabetes education, it aims to assist newly diagnosed patients in understanding what is GMI and managing their diabetes. The platform will provide valuable resources, including case studies like 'Graphs Visualizing CGM Data,' which offer practical illustrations of sugar fluctuations pre- and post-treatment, showcasing the effectiveness of GMI in real-world scenarios.
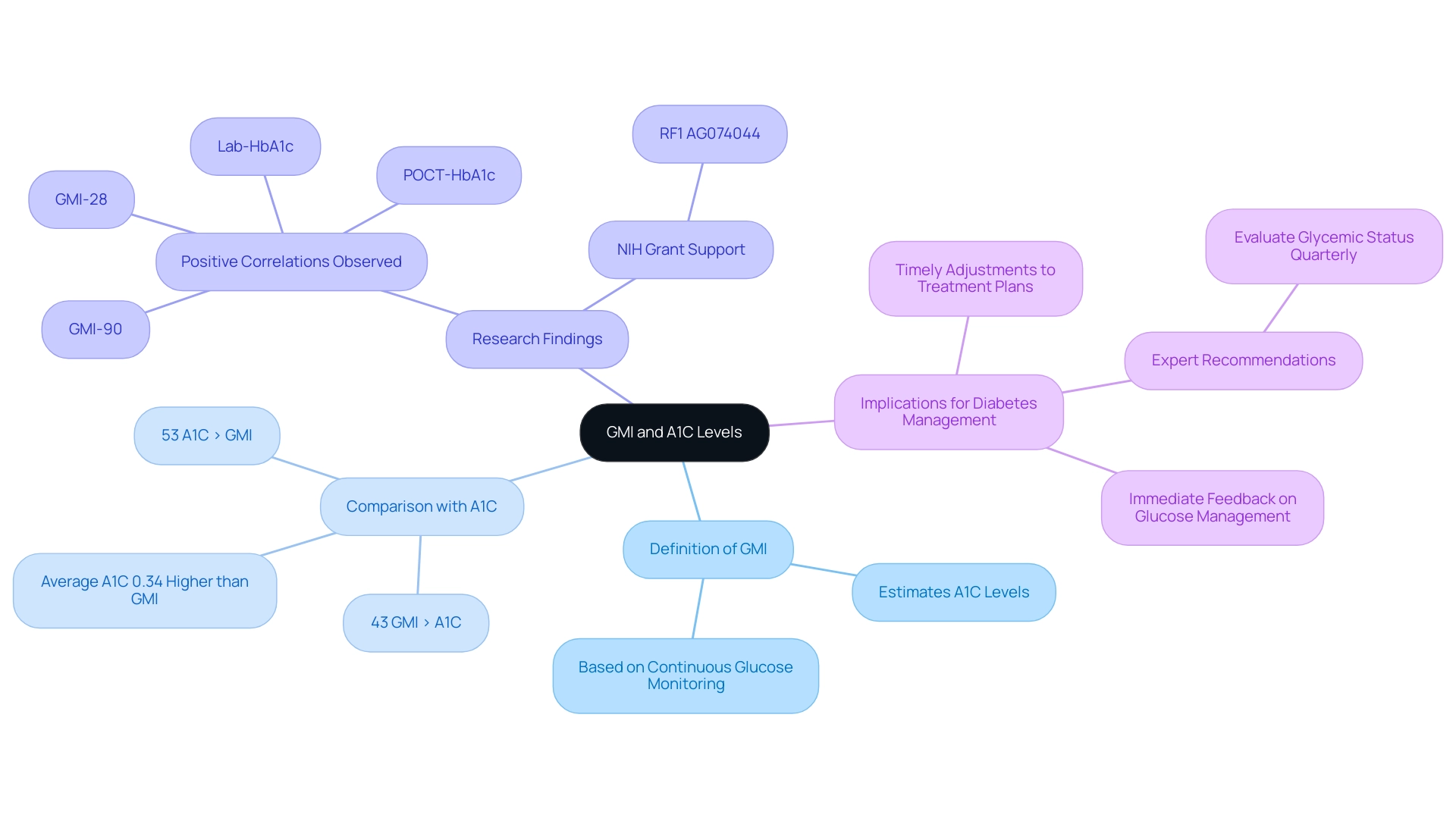
The Role of GMI in Estimating A1C Levels
What is GMI? The Glucose Management Indicator serves a crucial function in estimating A1C levels, which are traditionally measured through blood tests every three months. Unlike A1C, the GMI provides a dynamic estimate based on continuous glucose monitoring (CGM) data, facilitating more frequent evaluations of glucose control. Recent research indicates a strong correlation between GMI and A1C levels, which highlights what is GMI as a dependable alternative for individuals who may lack regular access to laboratory testing.
It is important to note that data on CGM effectiveness is sparse for diverse populations, including underrepresented groups and older adults, particularly those with type 2 conditions not on insulin. A retrospective analysis involving 26 individuals with both type 1 and type 2 blood sugar disorders demonstrated that while A1C was, on average, 0.34% higher than GMI, this discrepancy was not statistically significant. Notably, in 53% of individuals, A1C levels exceeded GMI, whereas in 43%, GMI levels were higher.
Additionally, significant positive correlations were observed among Lab-HbA1c, POCT-HbA1c, GMI-28, and GMI-90, further supporting what is GMI in managing blood sugar levels. These findings suggest that healthcare providers should consider incorporating CGM-derived GMI metrics into their assessments of glycemic control. By monitoring what is GMI, individuals receive immediate feedback on their glucose management, which enables timely adjustments to their treatment plans.
This proactive strategy is vital for optimizing diabetes care and enhancing overall health outcomes, aligning with the expert recommendation by Elsayed et al. to evaluate glycemic status at least quarterly in individuals not meeting their therapy goals. The research is backed by NIH grant RF1 AG074044, highlighting the significance of continued inquiry into the role of GMI in various groups.
As T2DSolutions opens as a new resource center for education and community assistance, understanding what is GMI will be crucial in helping recently diagnosed individuals comprehend their sugar management and treatment choices.
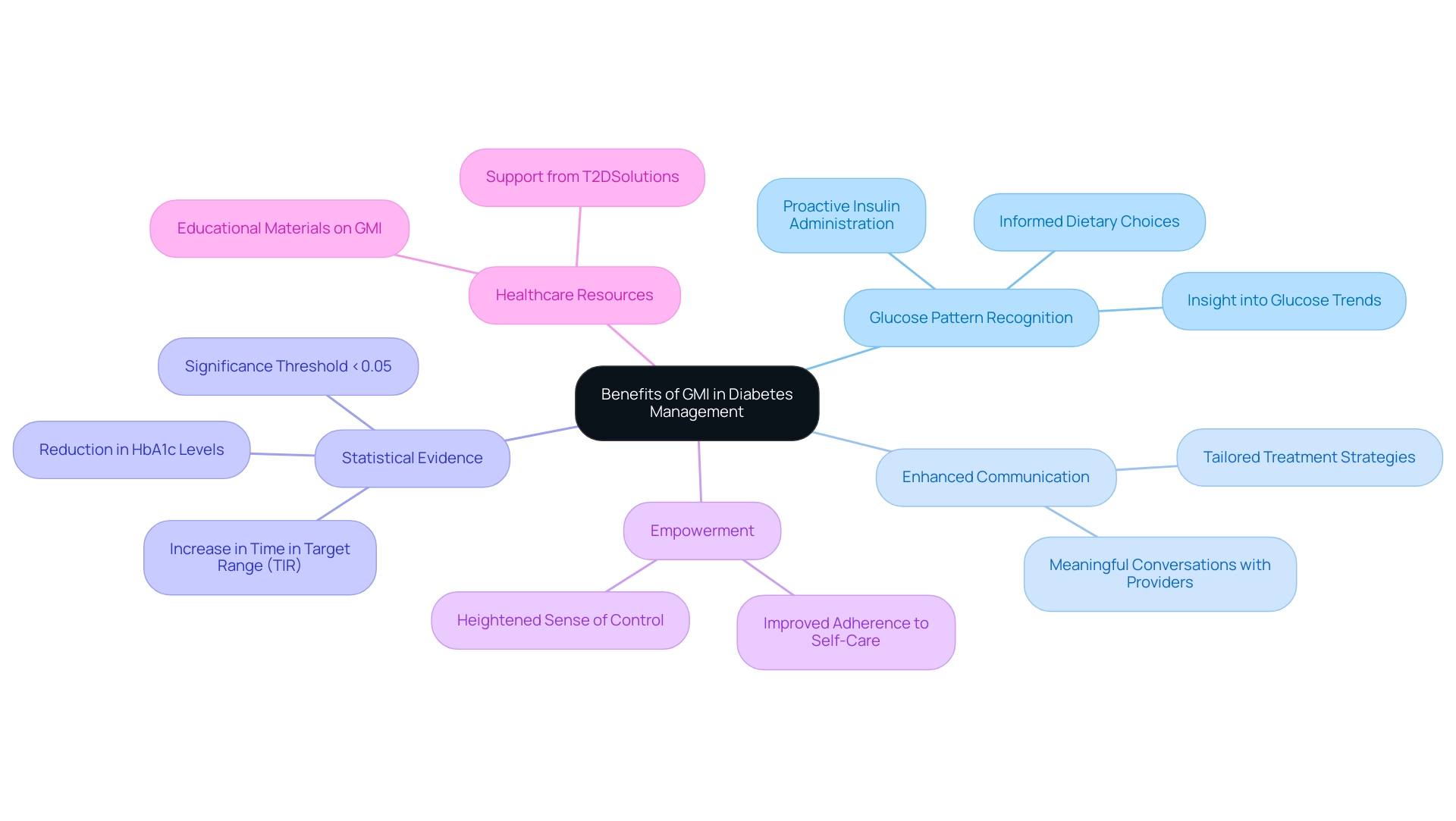
Benefits of Using GMI in Diabetes Management
Understanding what is GMI, the Glucose Management Indicator, can provide numerous advantages in diabetes management. Primarily, what is GMI provides individuals with a detailed insight into glucose patterns, enabling them to recognize trends that can inform their dietary choices and insulin administration. This analytical capability is crucial, as it allows for proactive adjustments rather than reactive measures.
Furthermore, GMI fosters enhanced communication between patients and healthcare providers. Such clarity facilitates more meaningful conversations regarding treatment strategies, ultimately leading to tailored care that meets individual needs.
As T2DSolutions launches as a comprehensive resource hub for Type 2 and Type 3 health education, understanding what is GMI will play a pivotal role in the resources provided. Research has highlighted positive effects on average blood glucose levels, with reductions in hypoglycemic events and an increase in time spent within the target range (TIR). Notably, studies have shown that these effects are statistically significant, with a threshold of <0.05.
A systematic review and meta-analysis encompassing 15 randomized controlled trials revealed that what is GMI refers to a notable reduction in HbA1c levels and a significant increase in TIR, corroborating its role in effective management of the condition. This case study, titled "Effects of Continuous Glucose Monitoring on Glycemic Control," provides concrete evidence answering what is GMI in managing blood sugar.
Moreover, individuals utilizing GMI often report a heightened sense of empowerment in managing their condition, which correlates with improved adherence to self-care practices. This proactive engagement not only enhances glucose control but also contributes significantly to the overall well-being of individuals managing this condition. As diabetes educators highlight, "The opinions stated in this publication reflect those of the authors and do not necessarily reflect the official perspectives of HCA Healthcare or any of its affiliated entities," empowering individuals through tools like GMI is crucial for promoting independence and confidence in their management journey.
T2DSolutions will offer additional support and resources to help patients effectively understand what is GMI in their daily management of diabetes.
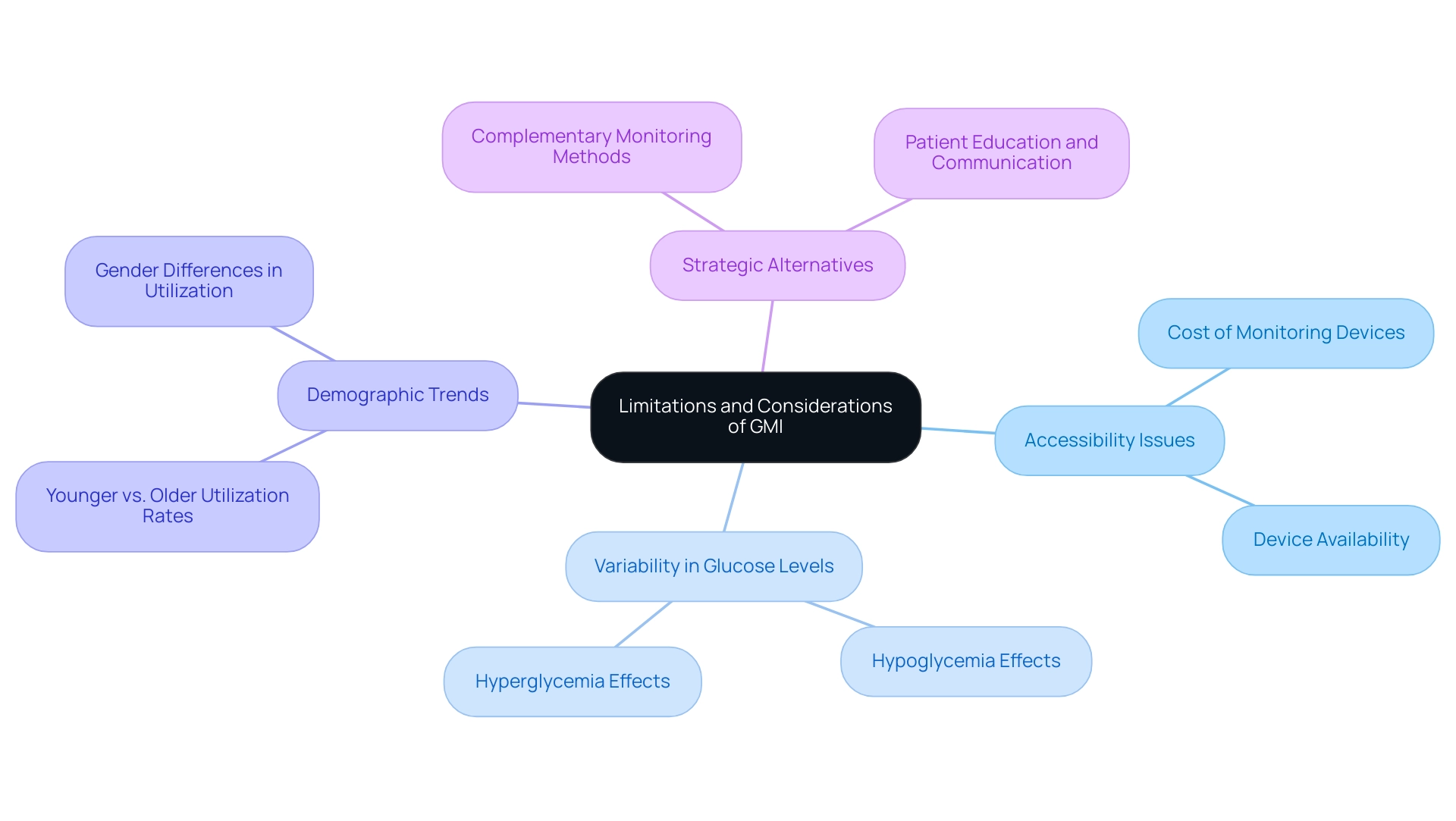
Limitations and Considerations of GMI
What is GMI? The Management Indicator provides essential insights into sugar control; however, it is crucial to recognize its limitations. A significant concern is the reliance on continuous monitoring of blood sugar data, which is not universally accessible due to cost and device availability. Estimates suggest that CGM utilization among adults with type 1 diabetes is alarmingly low, with some studies indicating rates between 8–17%.
This disparity emphasizes the need for alternative strategies in sugar management. Furthermore, GMI estimates can be affected by variations in glucose levels, such as hypoglycemia or hyperglycemia, which may not be consistently captured in the monitoring data. As Kovatchev BP highlights in his research, it is essential to approach what is GMI with a critical perspective, considering its limitations in managing blood sugar.
Additionally, the positive predictive value of using ICD-9 and ICD-10 codes to identify individuals with type 1 diabetes is 96.5%, underscoring the reliability of diabetes identification. The case study titled 'Demographic Trends in CGM Utilization' reveals that CGM use varies significantly by age group, with younger individuals showing higher utilization rates, while older age groups exhibit lower odds of utilization. Thus, individuals are encouraged to utilize GMI, as understanding what is GMI can complement other monitoring methods and help maintain open communication with their healthcare providers.
This comprehensive approach will empower patients to make informed decisions regarding their care, ensuring they understand what is GMI and leverage it effectively while acknowledging its constraints.
Conclusion
The Glucose Management Indicator (GMI) emerges as a vital tool in the landscape of diabetes management, offering a dynamic assessment of glucose levels that goes beyond traditional A1C testing. By utilizing continuous glucose monitoring (CGM) data, GMI provides patients and healthcare providers with a clearer picture of daily glucose fluctuations, facilitating more informed treatment decisions. The strong correlation between GMI and A1C levels reinforces its reliability, making it a practical alternative for patients who may not have consistent access to laboratory testing.
However, while GMI presents numerous advantages—including enhanced patient empowerment and improved communication with healthcare teams—it is essential to acknowledge its limitations. Accessibility to CGM technology remains a significant barrier for many, and the accuracy of GMI can be influenced by extreme glucose variations. Therefore, it is crucial for patients to approach GMI as part of a broader diabetes management strategy that incorporates various monitoring methods and ongoing dialogue with healthcare providers.
As resources like T2DSolutions continue to promote education and support regarding diabetes management, understanding and effectively utilizing GMI will be instrumental in helping individuals navigate their treatment options. By embracing GMI, patients can not only improve their glucose control but also foster a sense of autonomy and confidence in their health journey. The future of diabetes care hinges on innovative approaches such as GMI, which empower patients and enhance their overall well-being.



