Overview
The A1C calculation formula, which is A1C (%) = (Average Blood Glucose (mg/dL) + 46.7) / 28.7, is crucial for accurately assessing an individual's average blood glucose levels over the previous two to three months, thereby guiding diabetes management. The article emphasizes the importance of this formula in evaluating treatment effectiveness and highlights the need for regular A1C monitoring to prevent complications associated with poor glucose control, supporting a comprehensive approach to diabetes care.
Introduction
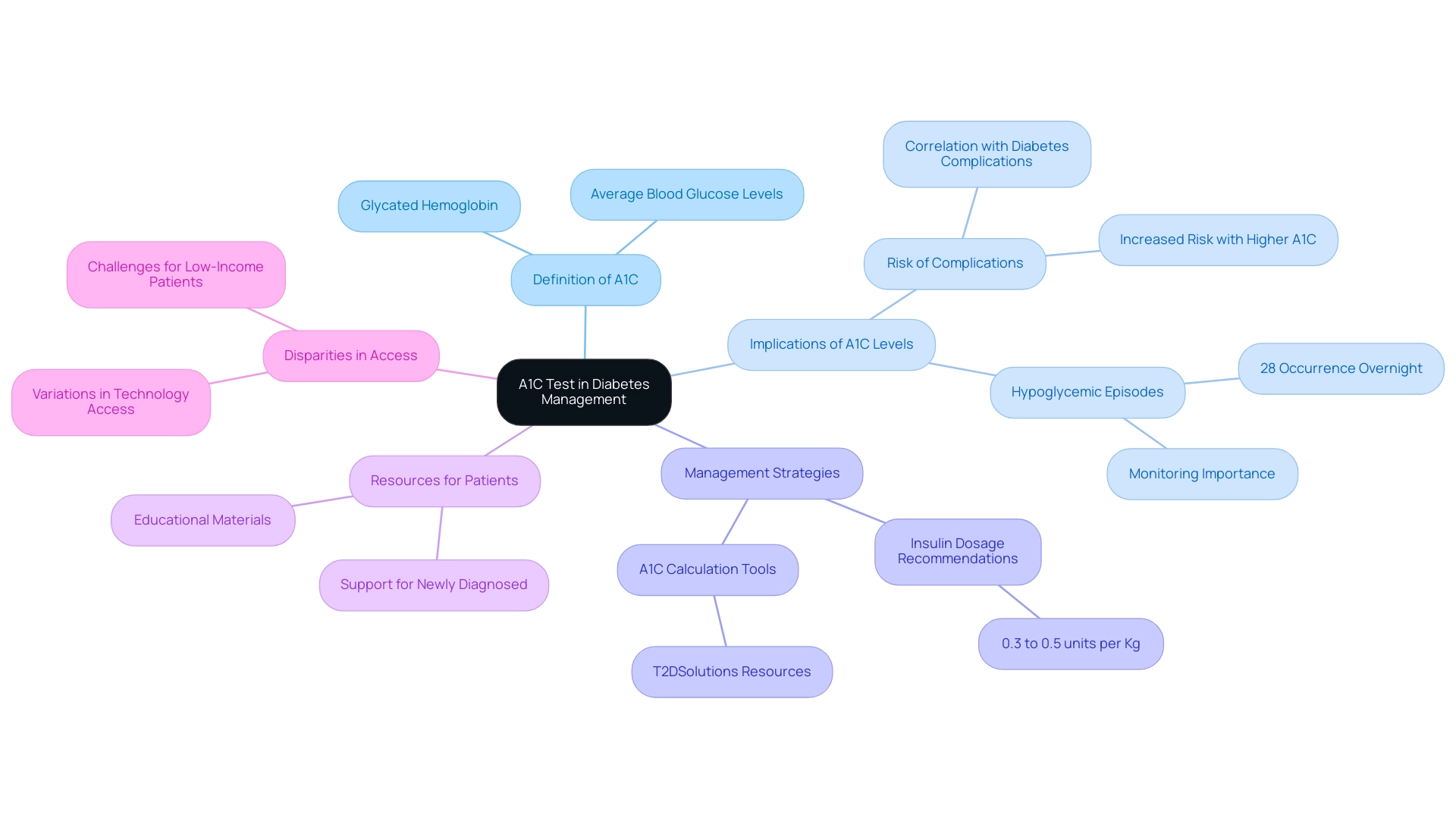
Managing diabetes effectively requires a comprehensive understanding of various metrics, with the A1C test standing out as a crucial tool in this process. This test measures average blood glucose levels over the past two to three months, offering valuable insights into a patient's long-term glucose control. As diabetes rates continue to rise across diverse populations, the significance of the A1C test in preventing complications and guiding treatment strategies cannot be overstated.
From calculating A1C percentages to recognizing its limitations, this article delves into the multifaceted role of the A1C test in diabetes management, highlighting essential practices and emerging methods that can enhance patient care. Through a detailed exploration of A1C monitoring, healthcare professionals and patients alike can better navigate the complexities of diabetes management and improve health outcomes.
Understanding the A1C Test: A Key Indicator in Diabetes Management
The A1C test, also known as glycated hemoglobin, serves as a fundamental measure of average blood glucose levels over the preceding two to three months. This essential instrument in blood sugar oversight enables healthcare professionals to obtain valuable insights into a patient's long-term glucose regulation. By determining the percentage of hemoglobin that is glycated, or coated with sugar, clinicians can assess the effectiveness of strategies for controlling blood sugar.
A higher A1C percentage reflects suboptimal blood sugar control, which correlates with an elevated risk of diabetes-related complications. Notably, the highest proportion of hypoglycemic episodes occurred overnight (28%) between 05:00 and 09:00 AM, underscoring the importance of monitoring blood glucose levels in relation to A1C testing. Given that the incidence of type 2 blood sugar condition has markedly increased across various racial and ethnic groups from 2002 to 2018, understanding and utilizing the A1C test is essential for minimizing these risks.
Furthermore, the recommended total daily insulin dose should start between 0.3 to 0.5 units per Kg for most individuals with this condition, underscoring the need for precise management based on A1C levels. Furthermore, it is essential to acknowledge the considerable differences in access to diabetes-related technologies and assistance for non-specialists, which can create obstacles for those recently diagnosed. T2DSolutions aims to bridge these gaps by offering a comprehensive A1C calculation formula designed to help individuals track their A1C levels and manage blood sugar effectively.
A case study by Umpierrez (2015) concentrated on CABG individuals showed that while A1C testing is crucial, there was no variation in mortality, emphasizing the intricacies of controlling blood sugar levels. In summary, the A1C test is not only a vital metric for evaluating care but also an indispensable component in preventing complications associated with poor glucose control. T2DSolutions is prepared to assist recently diagnosed individuals with resources and tools to improve their health journey.
How to Calculate A1C: Formulas and Methods Explained
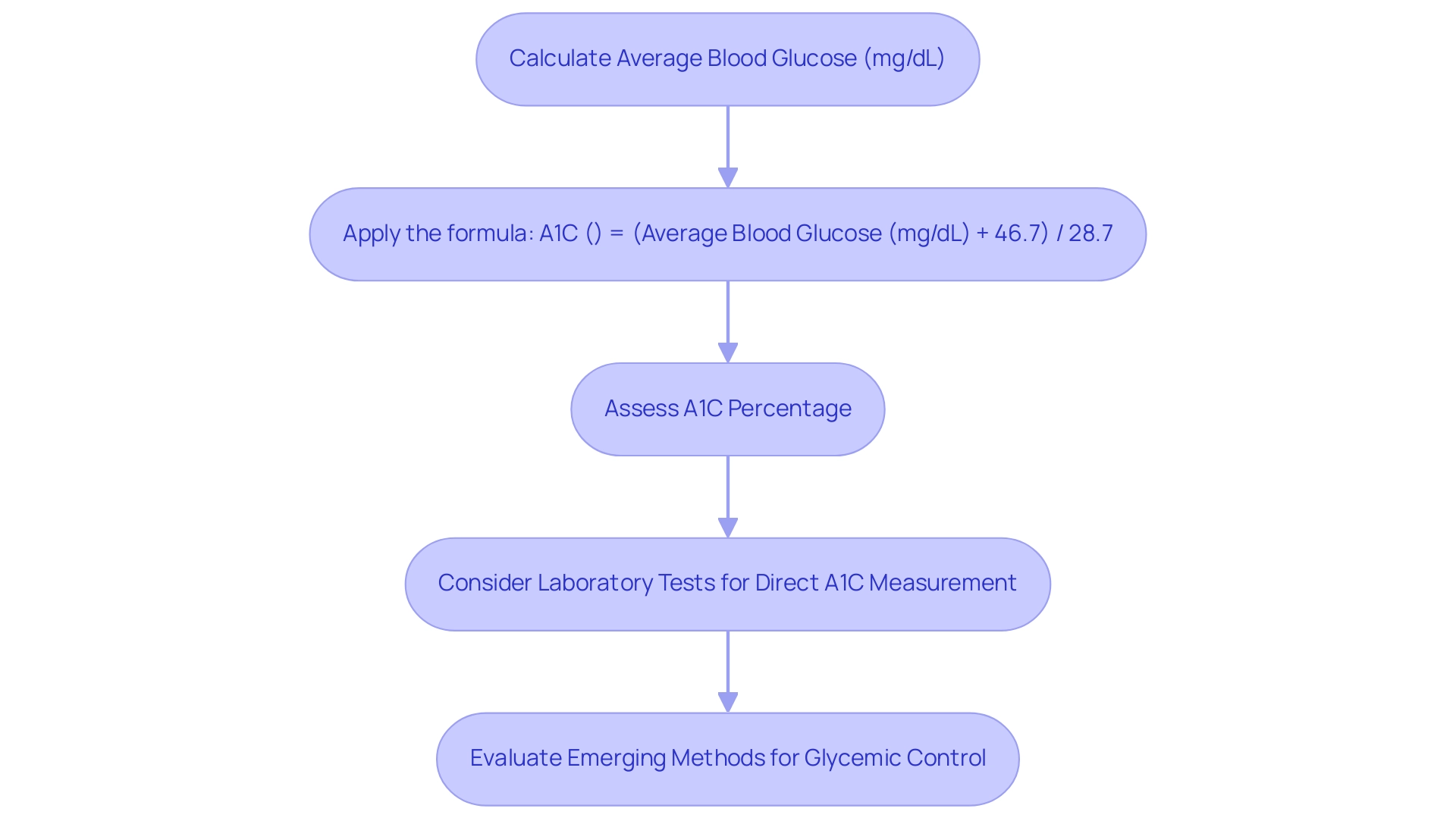
Calculating A1C is crucial in managing blood sugar levels, utilizing several methods, with the A1C calculation formula being the most prevalent as it correlates average blood glucose levels to A1C percentages. The standard A1C calculation formula used is:
A1C (%) = (Average Blood Glucose (mg/dL) + 46.7) / 28.7.
This A1C calculation formula allows healthcare professionals to convert average blood glucose readings into an A1C percentage, which is vital for assessing an individual's diabetes control.
T2DSolutions aims to support newly diagnosed individuals by providing comprehensive resources and tools to understand these calculations better. Moreover, laboratory tests that provide direct A1C measurements are often seen as more accurate than estimates derived from glucose readings. Emerging methods within the medical community suggest a movement toward integrating estimated average glucose and glucose time in range, as highlighted in the case study titled 'Emerging Methods for Glycemic Control.'
This shift aims to provide a more accurate view of blood sugar averages and fluctuations, although these methods are not yet widely available to all patients. Furthermore, an important statistic to consider is that 70.8% of U.S. adults with diagnosed conditions related to blood sugar had a systolic blood pressure of 140 mmHg or greater or diastolic blood pressure of 90 mmHg or greater, highlighting the intricacies of handling such conditions. As one expert noted, Hemoglobin A1C is a valuable tool in managing blood sugar disorders and other glycemic control issues, but it functions best in an interprofessional healthcare team environment to be effective.
This emphasizes the importance of open communication with healthcare providers in creating a comprehensive health care plan. T2DSolutions is dedicated to improving education and management regarding this condition, ensuring that patients have access to the necessary information and support to understand these nuances in A1C testing. Understanding these nuances is essential, as relying solely on A1C could lead to misdiagnosis, underscoring the importance of utilizing multiple methods for accurate assessment.
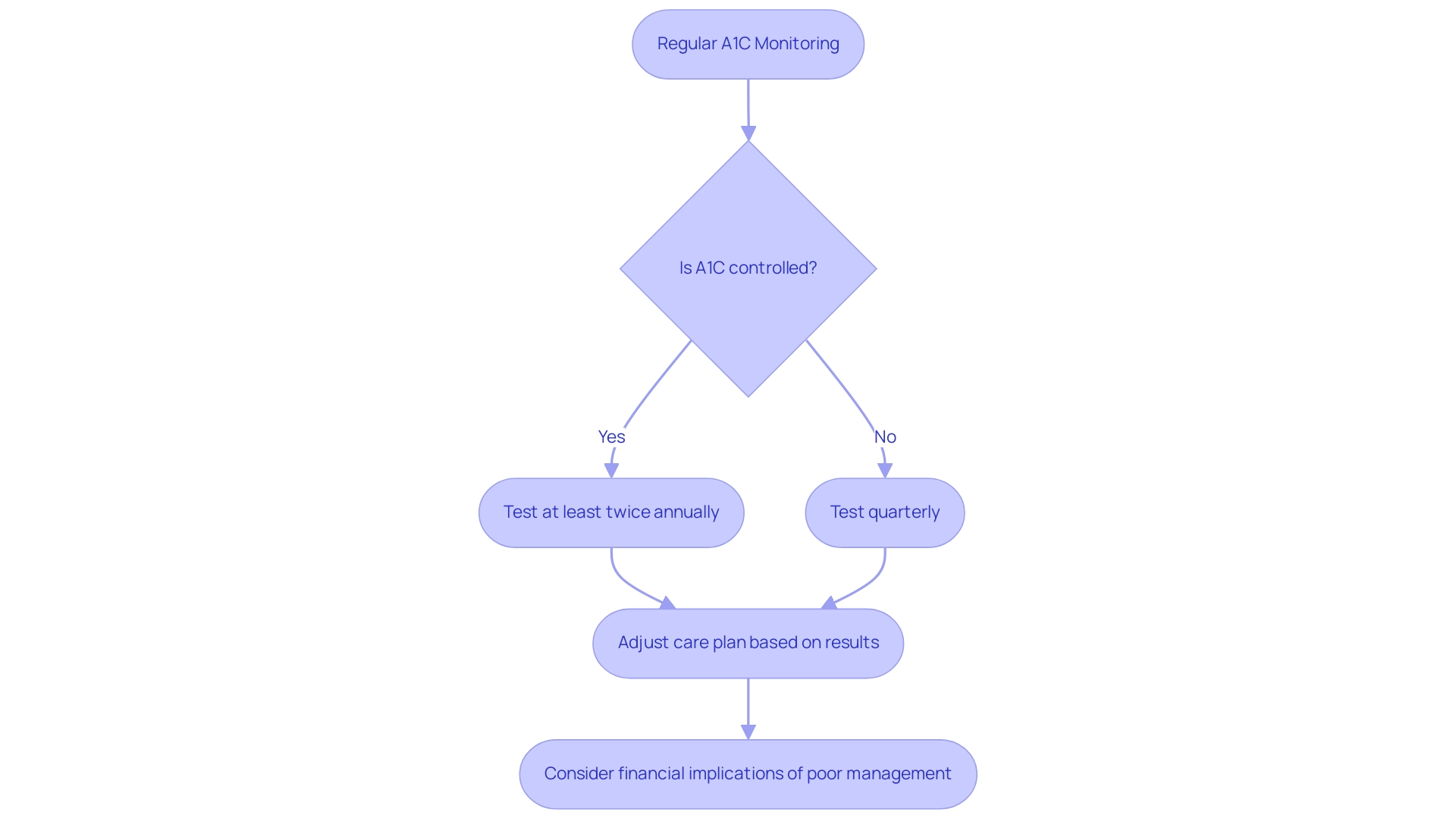
The Importance of Regular A1C Monitoring in Diabetes Care
Regular monitoring of A1C levels using the A1C calculation formula is vital for individuals managing their condition, serving as a key indicator of treatment effectiveness and facilitating necessary adjustments to care plans. According to the American Diabetes Association, most adults with the condition should undergo A1C testing at least twice annually if their status is well-controlled, while those experiencing treatment changes or not achieving target levels should be tested quarterly. This proactive approach to monitoring significantly aids in making timely interventions, thereby reducing the risk of complications associated with poorly managed blood sugar levels.
Notably, a recent study indicated that among adults with the condition, approximately 47.4% had A1C values of 7.0% or higher, reflecting ongoing challenges in maintaining optimal glycemic control. The financial implications of poorly managed blood sugar levels are significant, with excess medical costs per person rising from $10,179 in 2012 to $12,022 in 2022. The significance of regular A1C monitoring is additionally backed by expert insights, including those from Robert A. Gabbay, a member of the American Diabetes Association Professional Practice Committee, who stresses the necessity of structured care in managing the condition effectively, as detailed in the 'Standards of Care in Diabetes–2024.'
Additionally, deintensifying therapy for older adults, particularly regarding hypoglycemia-causing medications, is a crucial strategy in managing blood sugar. Real-world examples show that treatment modifications based on the A1C calculation formula can lead to enhanced outcomes for individuals, emphasizing the essential requirement for regular monitoring in care. ATd Solutions, we provide extensive resources and tools to help you monitor your A1C levels effectively and manage your condition more efficiently.
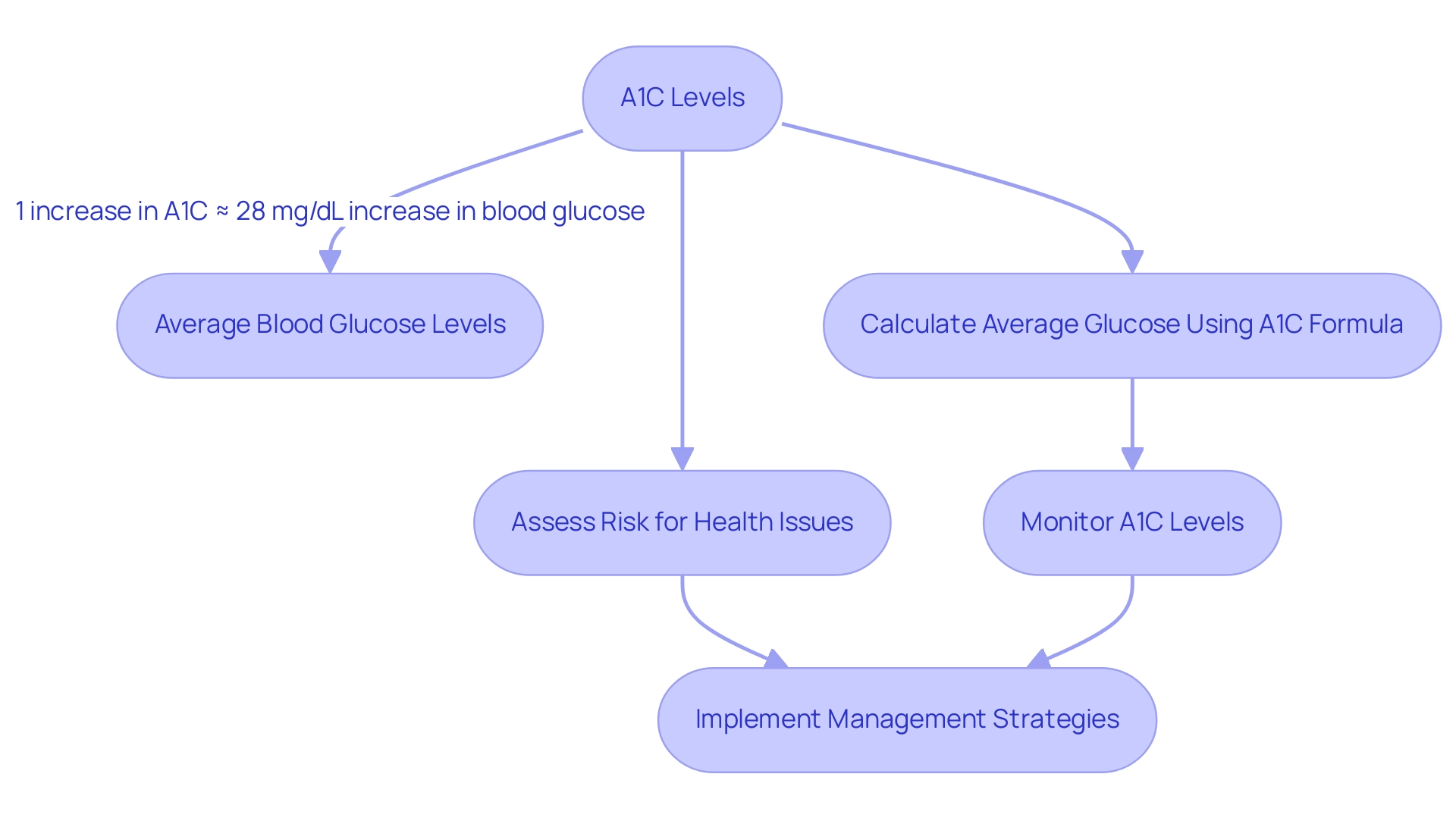
Connecting A1C Levels to Average Blood Glucose: What You Need to Know
The connection between A1C levels and average blood glucose is crucial in managing the condition, as the A1C calculation formula provides a thorough understanding of a patient's glucose regulation over time. Research has demonstrated that for each 1% increase in A1C, there is an approximate rise of 28 mg/dL in average blood glucose levels. This established correlation enables healthcare providers to estimate average glucose levels based on A1C percentages through the A1C calculation formula, thereby facilitating enhanced management strategies.
As highlighted by Dr. Nam H. Cho, the primary conclusion of this research is that the A1C assay was beneficial as a screening tool for type 2 and as a predictor of future onset. This underscores the importance of understanding A1C levels for patients, as it empowers them to make informed decisions regarding their lifestyle and treatment options. Furthermore, according to the A1C calculation formula, A1C levels ≥5.6% indicate an elevated risk for future health issues, supporting the need for early preventive interventions.
A longitudinal study titled 'Longitudinal Analysis of Diabetes Risk Factors' highlighted that A1C levels were independently linked to an increased risk of new-onset conditions, reinforcing the necessity of regular screenings for individuals at risk. Furthermore, as highlighted by Emily Eyth, the latest suggested techniques, including estimated average glucose and glucose time in range, offer modern perspectives on health control. By understanding how A1C variations relate to blood glucose levels, individuals can use the A1C calculation formula to actively participate in their condition care, improving their overall health results.
At t D Solutions, we provide extensive A1C and blood sugar calculators, along with educational materials and community assistance, to empower newly diagnosed patients in their health journey.
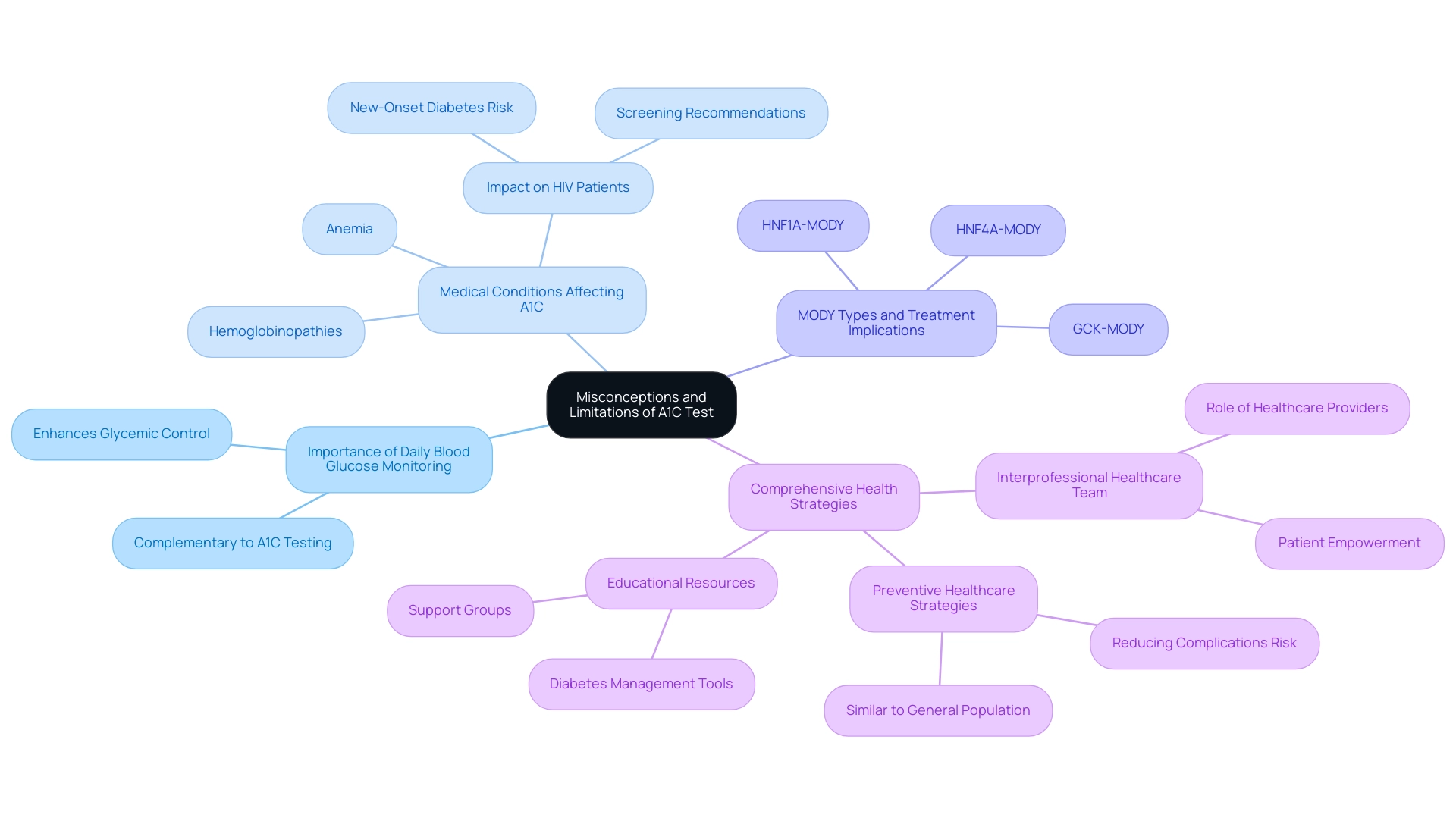
Common Misconceptions and Limitations of the A1C Test
While the A1C calculation formula plays a crucial role in managing blood sugar levels, it is essential to recognize its limitations. A widespread misunderstanding is that the A1C calculation formula can serve as the sole metric for monitoring the condition; however, it is most effective when used in conjunction with daily blood glucose monitoring. For instance, new-onset blood sugar disorder is estimated to occur in more than 5% of individuals infected with HIV on protease inhibitors, highlighting a specific population that may be affected by A1C testing limitations.
Certain medical conditions, such as anemia and hemoglobinopathies, can distort A1C results, emphasizing the need for an A1C calculation formula to ensure accurate evaluations of glycemic control. Additionally, common forms of MODY, such as GCK-MODY, HNF1A-MODY, and HNF4A-MODY, have specific treatment implications that could further complicate the reliance on A1C alone. Acknowledging these limitations is vital for both patients and healthcare providers who utilize the A1C calculation formula.
A thorough health condition oversight strategy should incorporate the A1C calculation formula and multiple monitoring techniques to ensure precise evaluation and effective treatment. As mentioned by Emily Eyth, 'Hemoglobin A1c is a valuable tool in managing blood sugar conditions and other glycemic control disorders, but it functions best in an interprofessional healthcare team environment to be effective.' Furthermore, a case study titled 'Diabetes Risk in People With HIV' emphasizes that preventive healthcare strategies similar to those for the general population are critical for reducing the risk of complications.
Grasping these subtleties can greatly improve care and outcomes. T2DSolutions aims to become a comprehensive resource hub for Type 2 and Type 3 blood sugar management education and community support. The platform will provide educational resources, access to support groups, and tools specifically crafted to help newly diagnosed individuals in navigating their diabetes care effectively.
By addressing the limitations of A1C testing and providing essential resources, T2D Solutions will empower patients to take charge of their health and improve their management outcomes.
Conclusion
The A1C test serves as a cornerstone in diabetes management by providing a vital measure of long-term blood glucose control. Its ability to reflect average glucose levels over two to three months enables healthcare professionals to assess treatment effectiveness and adjust care plans accordingly. Regular monitoring of A1C levels is critical, as it helps in identifying patients at risk of complications and facilitates timely interventions. Despite its importance, it is essential to recognize the limitations of the A1C test, including potential inaccuracies in specific populations and medical conditions.
Emerging methods and tools, such as those offered by T2DSolutions, aim to enhance understanding and management of diabetes through comprehensive resources that support patients in tracking their A1C levels and making informed decisions. By integrating the A1C test with daily blood glucose monitoring and other assessment methods, individuals can achieve a more accurate picture of their glycemic control, ultimately leading to improved health outcomes.
In conclusion, the A1C test is not merely a number; it represents a vital aspect of diabetes care that can significantly influence treatment strategies and patient wellbeing. By fostering awareness of its role and limitations, as well as providing robust support systems, patients and healthcare providers can work together to navigate the complexities of diabetes management effectively.



