Overview
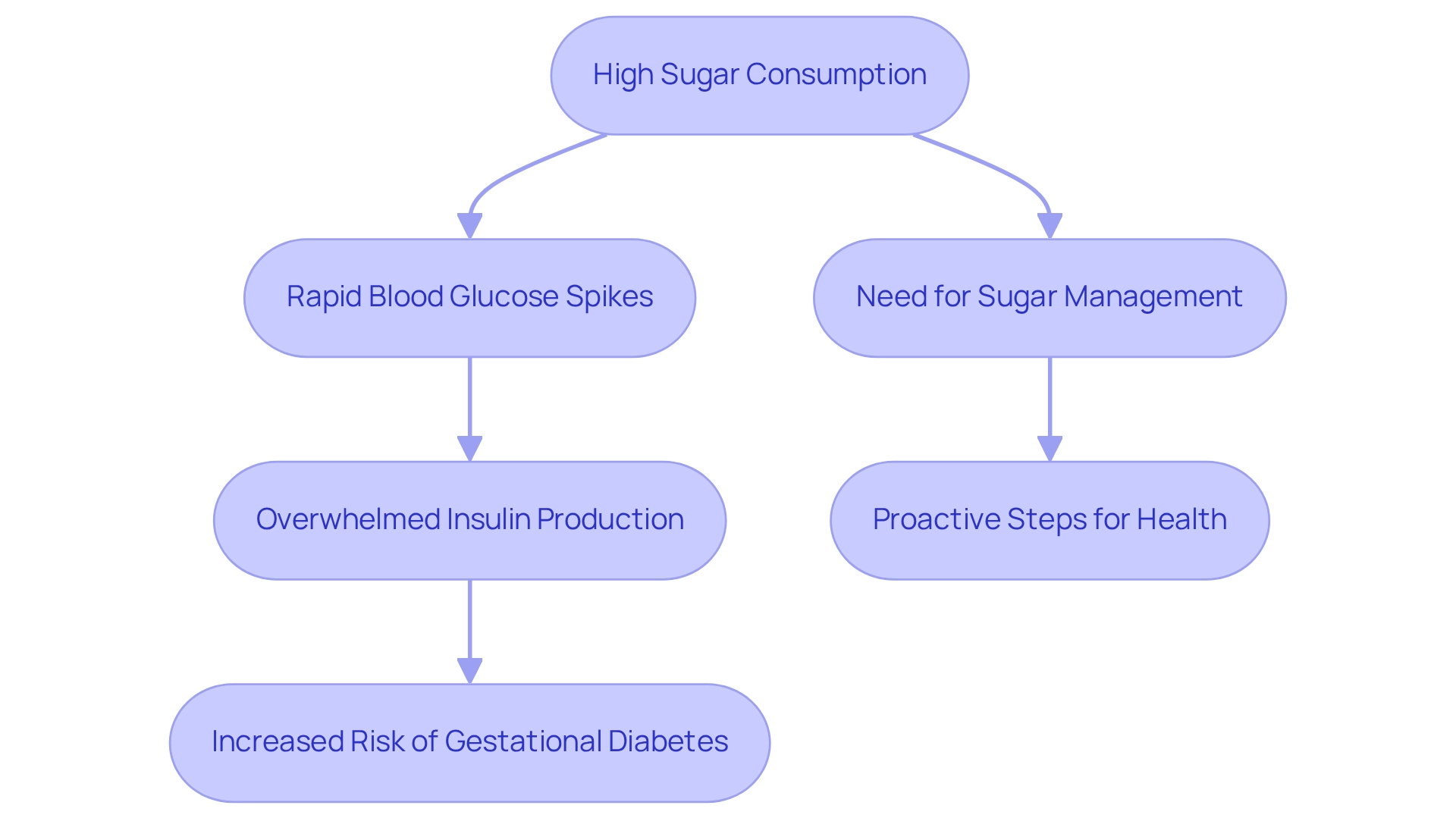
It's important to recognize the significant connection between eating too much sugar and gestational diabetes. Excessive sugar intake can worsen insulin resistance, increasing the likelihood of developing gestational diabetes mellitus (GDM). This can be particularly concerning during pregnancy, as high sugar consumption often leads to spikes in blood glucose levels. These spikes can overwhelm the body's insulin production, raising the risk of GDM.
Understanding this relationship is crucial for expectant mothers. It’s understandable to feel apprehensive about dietary choices during this time. By being mindful of sugar intake, you can take proactive steps to safeguard your health and that of your baby. You're not alone in this journey; many women share similar concerns.
We encourage you to seek support and resources that can help you make informed dietary decisions. Remember, taking small, manageable steps can lead to positive changes. Together, we can navigate this path toward a healthier pregnancy.
Introduction
Gestational diabetes mellitus (GDM) is a significant health concern that arises during pregnancy, impacting both mothers and their developing children. As we witness a rise in the prevalence of this condition, understanding its implications becomes increasingly vital. GDM occurs when the body struggles to produce enough insulin to meet the heightened demands of pregnancy, resulting in elevated blood sugar levels that can lead to serious complications.
It's important to know that nearly 6-9% of pregnancies in the United States are projected to be affected by GDM in the near future. This statistic can be overwhelming, but proactive management through early screening, dietary adjustments, and lifestyle changes is essential.
In this article, we will explore various aspects of gestational diabetes—from its causes and risk factors to effective management strategies. Our goal is to equip expectant mothers with the knowledge needed to navigate this condition, ensuring they can safeguard their health and that of their babies. Remember, you're not alone in this journey; we are here to support you every step of the way.
Understanding Gestational Diabetes: An Overview
Gestational glucose intolerance (GDM) is a condition that occurs during pregnancy, often leading to concerns about whether eating too much sugar causes gestational diabetes. Typically identified in the second or third trimester, GDM is characterized by elevated blood sugar levels, raising the question of its implications for both the mother and the developing fetus. It’s important to understand that unlike pre-existing blood sugar issues, GDM arises when the body struggles to produce enough insulin to meet the increased demands of pregnancy.
This condition can lead to significant complications, including excessive fetal growth, preterm birth, and a heightened risk of developing type 2 diabetes later in life. It’s understandable to feel concerned about these potential outcomes.
Recent statistics indicate an increasing prevalence of pregnancy-related sugar issues. Estimates suggest that around 6-9% of pregnancies in the United States will be impacted by GDM in 2025. Grasping the nuances of gestational conditions is crucial for effective management and ensuring favorable outcomes for both mother and child.
Expert opinions emphasize the importance of early screening and education for expectant mothers. Healthcare experts advocate for regular examinations, especially for women who may be vulnerable, such as those with a family history of blood sugar issues or those who are overweight. Routine screening is also recommended for adults aged 45 years or older, highlighting the broader context of managing blood sugar conditions.
This proactive strategy can significantly lessen challenges associated with GDM. In collaboration with WHO, Md. Rabiul Islam stresses that governments of low- and middle-income countries (LMICs) should enhance the accessibility of healthcare programs, including more regular screenings for individuals at risk. This underscores the importance of proactive screening and management strategies for blood sugar conditions, particularly regarding the question of whether eating too much sugar causes gestational diabetes.
Practical instances demonstrate effective management techniques for pregnancy-related blood sugar issues. Many healthcare providers recommend personalized dietary plans and regular physical activity, which have been shown to help regulate blood sugar levels effectively. Continuous glucose monitoring has also emerged as a valuable tool for managing GDM, allowing for real-time adjustments to diet and activity levels.
The latest research emphasizes the necessity for thorough education on gestational health issues. Understanding the condition can empower women to take control of their well-being. Studies have shown that informed patients are more likely to adhere to management plans, leading to better health outcomes. Addressing risk factors such as obesity and a sedentary lifestyle is essential in understanding whether eating too much sugar causes gestational diabetes.
The challenges of managing diabetes-related issues in various contexts, such as those highlighted in the case study titled 'Challenges in Diabetes Management in Africa,' illustrate unique obstacles faced, including insufficient funding and limited access to healthcare facilities. Implementing early screening initiatives in these regions could be a strategic approach to managing blood sugar conditions, including GDM, while addressing the economic implications of the disease.
In summary, pregnancy-related glucose intolerance is a significant health concern that requires attention and understanding. By acknowledging the challenges and applying effective management strategies, expectant mothers can navigate this condition successfully, ensuring the well-being of both themselves and their babies. Remember, you're not alone in this journey; we are here to support you every step of the way.
The Impact of Sugar Consumption on Gestational Diabetes
It's understandable to feel concerned about sugar intake during pregnancy, especially with studies indicating a connection between high sugar consumption and gestational diabetes. Sugary foods and beverages can cause rapid spikes in blood glucose levels, which may overwhelm the body's ability to produce insulin. Research has shown that excessive intake of simple sugars raises questions about whether it contributes to gestational diabetes, as it is often linked to greater weight gain during pregnancy and a higher likelihood of developing this condition.
For instance, a study published in the Journal of Clinical Endocrinology & Metabolism found that women consuming large quantities of sugary foods faced an increased risk of pregnancy-related glucose intolerance. This discovery raises an important question: does eating too much sugar lead to gestational diabetes compared to those who limit their sugar intake? Therefore, managing sugar consumption is crucial for preventing this condition.
You're not alone in this journey. If you're feeling overwhelmed, remember that there are resources and support available to help you navigate these concerns. Taking proactive steps can make a significant difference in your health and well-being during this important time.
Recognizing the Symptoms of Gestational Diabetes
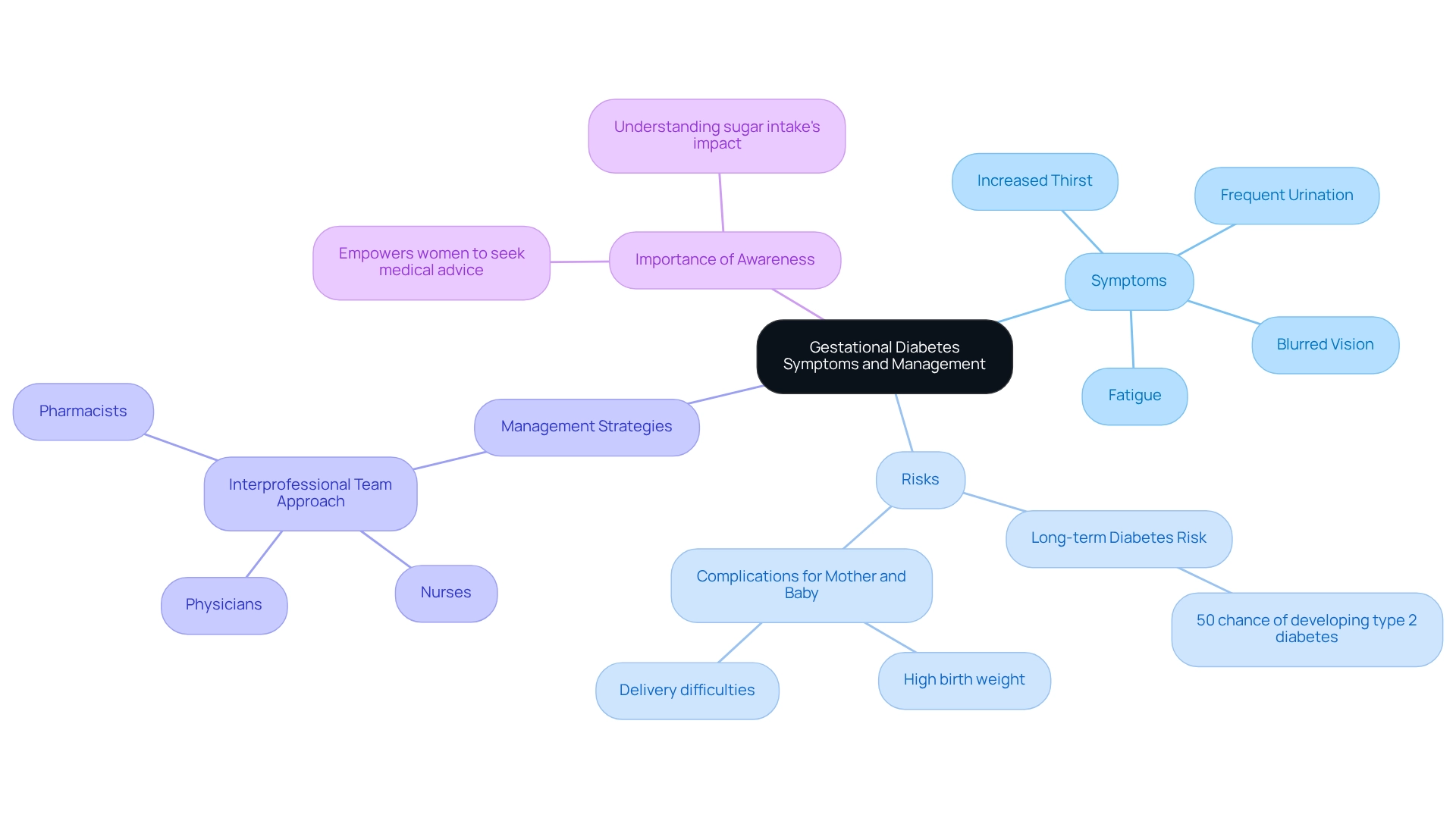
Gestational glucose intolerance often presents with subtle or even absent symptoms, which makes it crucial for pregnant individuals to remain vigilant about potential indicators. Common symptoms include:
- Increased thirst
- Frequent urination
- Fatigue
- Blurred vision
However, it's important to know that research indicates approximately 50% of women may not exhibit any noticeable symptoms. This underscores the critical importance of routine screening during pregnancy.
Moreover, about half of the women who experience pregnancy-related glucose intolerance may go on to develop type 2 diabetes, highlighting the long-term consequences of this condition.
The consequences of uncontrolled pregnancy-related blood sugar levels can be serious, leading to issues like high birth weight and delivery difficulties. A collaborative interprofessional team approach is essential for effective management, involving physicians, nurses, and pharmacists to ensure comprehensive care. As noted by the Cleveland Clinic, "Yes, having pregnancy-related sugar issues may make your condition high risk."
This teamwork not only enhances patient safety but also optimizes therapy and improves overall maternal and fetal health outcomes. This is illustrated in the case study titled 'Interprofessional Team Approach in GDM Management,' which shows how integrating diverse expertise and resources can significantly enhance patient care.
Awareness of these symptoms is vital, as it empowers women to seek medical advice and undergo necessary testing to understand if eating too much sugar contributes to gestational diabetes. By identifying the indicators and comprehending the dangers linked to pregnancy-related sugar issues, individuals can better understand whether their sugar intake is a factor and take proactive measures to protect their health and that of their baby.
At T2DSolutions, we are dedicated to offering resources and assistance for recently diagnosed patients managing gestational conditions. Our forthcoming material will provide useful information on controlling blood sugar levels during pregnancy, ensuring that individuals have access to the resources they require for effective management. Remember, you're not alone in this journey; we are here to support you every step of the way.
Identifying Risk Factors for Gestational Diabetes
Gestational glucose intolerance (GDM) can be influenced by various factors, significantly increasing a woman's risk of developing this condition. Key contributors include:
- Being overweight or obese
- Having a family history of blood sugar issues
- Being over the age of 25
It's understandable to feel concerned when recent statistics reveal a strong link between obesity and the occurrence of diabetes during pregnancy; women with a higher pre-pregnancy body mass index (BMI) face a notably elevated risk.
In fact, research indicates that the odds of cesarean sections in the GDM group are 1.7 times higher than in those without the condition. This can be alarming, but understanding these risks is the first step toward proactive management.
Dietary habits also play a crucial role in determining whether consuming too much sugar contributes to gestational diabetes. Many women who consume high amounts of refined carbohydrates and sugars often wonder, does eating too much sugar cause gestational diabetes? A comprehensive study emphasizes that excessive weight gain during pregnancy further increases the likelihood of developing GDM. Recognizing these factors underscores the importance of tailored interventions, such as weight management and equitable healthcare access, to improve maternal and infant outcomes.
It's vital to recognize these danger elements for effective management. Expert insights suggest that understanding the interplay between obesity, family history, and dietary choices can empower women to take preventive measures. For instance, case studies have shown that education on hypoglycemia prevention and management is essential for pregnant individuals with blood sugar issues, aiding in reducing risks and ensuring better health outcomes.
Real-world examples illustrate the challenges faced by women at risk of developing this condition, particularly those living in urban areas where health hazards related to hypertension and obesity are prevalent. These socio-demographic vulnerabilities can significantly affect health outcomes. As Quintanilla Rodriguez BS observes, "These clinics not only reduce the workload of obstetricians but also ensure that expectant mothers with temporary high blood sugar receive thorough, coordinated care that addresses both their immediate needs and long-term health concerns."
By identifying these risk factors and applying informed strategies, women can significantly lower their chances of developing pregnancy-related complications. This proactive approach can lead to healthier pregnancies and improved long-term well-being for both mother and child. Remember, you're not alone in this journey; we are here to support you every step of the way.
What Causes Gestational Diabetes? The Role of Diet
Gestational glucose intolerance primarily arises from hormonal changes during pregnancy that lead to insulin resistance. As the placenta develops, it secretes hormones that can hinder insulin's effectiveness, resulting in elevated blood sugar levels. This condition is significantly influenced by dietary choices. The question often arises: does eating too much sugar cause gestational diabetes? Excessive sugar consumption can exacerbate insulin resistance and increase the likelihood of gestational diabetes (GDM).
Research indicates that diets high in simple sugars and low in fiber raise concerns about the potential link between sugar intake and gestational diabetes. Conversely, maintaining a balanced diet rich in whole grains, fruits, and vegetables is essential for effectively managing blood sugar levels throughout pregnancy. Additionally, engaging in organized physical activity for 150 to 180 minutes each week during pregnancy has been shown to reduce the likelihood of GDM by up to 90% compared to standard care.
This emphasizes the importance of adopting healthier lifestyle habits during the preconception period and throughout pregnancy. By understanding the interaction between diet, physical activity, and hormonal changes, you can take proactive steps to reduce the risks associated with pregnancy-related blood sugar issues. You're not alone in this journey, and there are resources available to support you.
At T2DSolutions, we understand the significance of tailored information and resources for managing pregnancy-related blood sugar conditions. As part of our commitment to supporting you, we aim to provide educational materials and community support that empower those affected by GDM. We invite you to subscribe for updates on resources related to pregnancy-related blood sugar management, ensuring you have access to the latest information and support from T2D Solutions.
Preventing Gestational Diabetes: Dietary Strategies
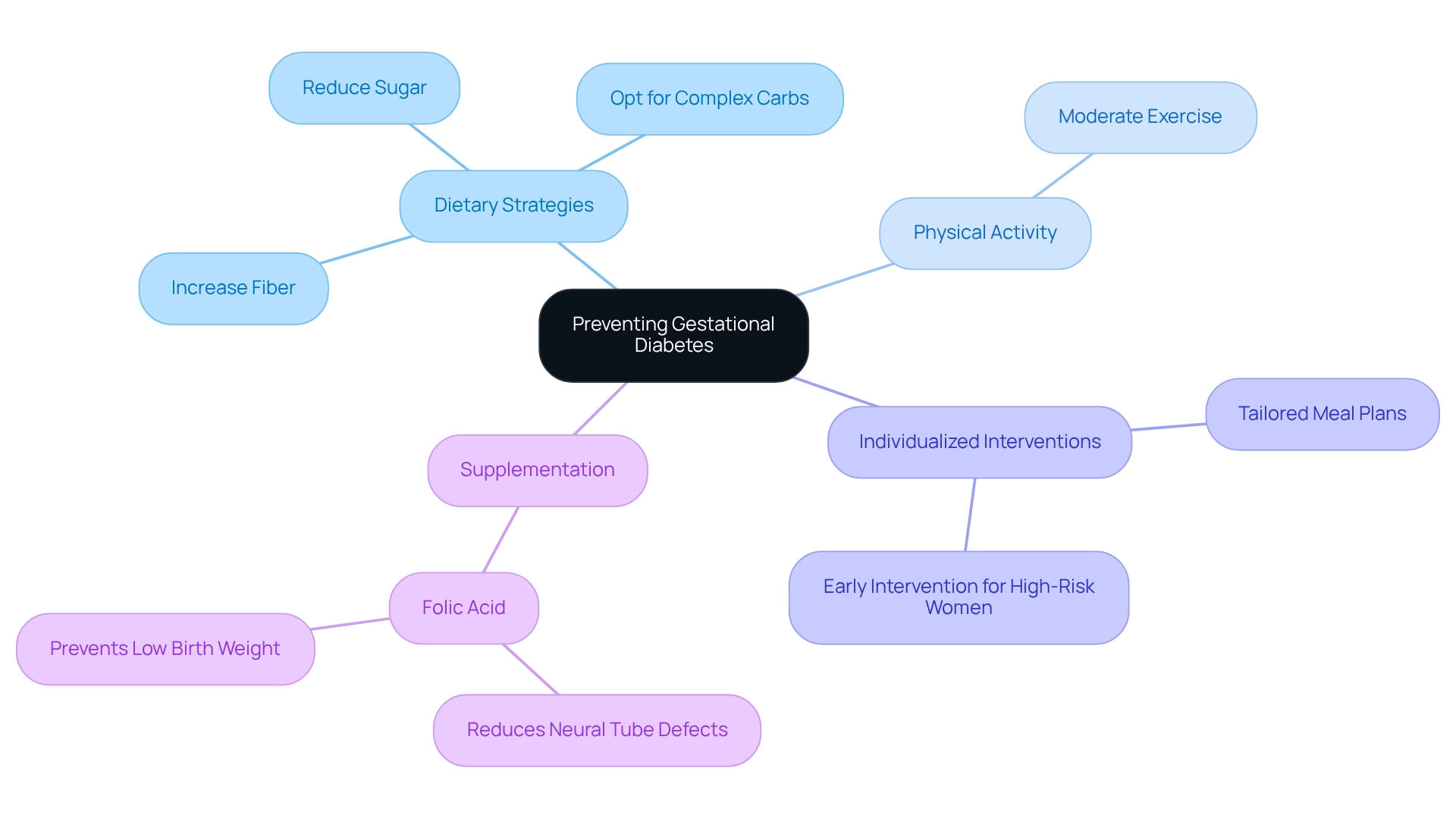
Avoiding pregnancy-related glucose issues requires a proactive strategy centered on a nutritious diet and lifestyle changes. It's important to consider how sugar intake can impact gestational diabetes. Therefore, significantly reducing sugar consumption, opting for complex carbohydrates, and increasing fiber intake are key dietary strategies. As you navigate this journey, focus on balanced meals that include lean proteins, healthy fats, and a variety of fruits and vegetables.
Regular physical activity is equally crucial; even moderate exercise can help regulate blood sugar levels effectively. Remember, you’re not alone in this journey, and every small step counts.
Recent findings highlight the importance of individualized lifestyle interventions, especially for women at higher risk. Saila B. Koivusalo from the Department of Obstetrics and Gynecology at the University of Helsinki emphasizes, "Our findings suggest that individualized lifestyle intervention should be initiated in early pregnancy in high-risk women and continued throughout pregnancy." This truly underscores the significance of tailored approaches for those facing greater vulnerability.
The American Diabetes Association encourages women at risk of developing gestational diabetes to collaborate with healthcare providers in creating personalized meal plans. These plans should focus on whole foods while reducing processed sugars, acknowledging the potential effects of excessive sugar intake.
A systematic review and meta-analysis have shed light on effective interventions for preventing gestational diabetes, reinforcing the importance of dietary choices. For instance, women adhering to a low-carbohydrate diet may experience lower postprandial glucose levels, which is essential for managing blood sugar. However, it’s worth noting that there is no consensus on the optimal carbohydrate intake; some studies show no significant differences in pregnancy outcomes across various carbohydrate diets, emphasizing the need for further investigation.
In addition to dietary approaches, folic acid supplementation is vital during pregnancy, as it reduces the risk of neural tube defects and low birth weight. By following these dietary suggestions and lifestyle modifications, you can significantly lower your risk of developing pregnancy-related conditions. This raises an important question: does eating too much sugar cause gestational diabetes? Ultimately, these steps encourage healthier outcomes during pregnancy.
Managing Gestational Diabetes: Treatment and Dietary Recommendations
Effectively managing gestational diabetes mellitus (GDM) requires a multifaceted approach that includes dietary changes, regular physical activity, and diligent monitoring of blood sugar levels. For women diagnosed with GDM, it's important to follow a structured meal plan that features three balanced meals and two to three snacks each day. Prioritizing low glycemic index foods is essential, as these foods release sugar gradually into the bloodstream, helping to keep blood glucose levels stable.
Regularly checking blood glucose levels is crucial. This practice allows for timely adjustments to your management plan. Research shows that about 15.3% of mothers aged 40 and above experience GDM, while the rate is around 2.5% for mothers under 20. This statistic underscores the need for targeted interventions tailored to different age groups.
If dietary changes alone are not enough, insulin therapy may be considered to achieve better blood sugar control. Collaborating with healthcare providers is vital in crafting a comprehensive management strategy that meets both the mother's and baby's health needs.
For instance, a recent case study on dietary management for pregnancy-related glucose issues found that women who followed a personalized meal plan saw significant improvements in their blood sugar levels. This highlights how effective dietary interventions can be.
As we look towards 2025, experts emphasize the importance of individualized dietary recommendations, which can greatly influence the management of GDM. As Khan notes, "This is a growing problem, and one that requires focused attention and increased awareness." The American Diabetes Association® continues to advocate for research and resources to support effective management of this condition, reinforcing the critical nature of education and awareness in addressing this pressing issue.
By adopting a proactive approach to managing pregnancy-related blood sugar challenges, you can enhance your health outcomes and those of your baby. Remember, you're not alone in this journey; we are here to support you every step of the way.
Long-Term Effects of Gestational Diabetes: What to Expect
Women who encounter gestational diabetes mellitus (GDM) may understandably feel concerned about their health in the long term. It's important to know that those who experience GDM face a significantly increased risk of developing type 2 diabetes later in life. Research shows that nearly 50% of women with a history of GDM will progress to type 2 metabolic disorder within 5 to 10 years after childbirth. This statistic highlights the crucial need for proactive health management during the postpartum period.
Additionally, children born to mothers with GDM are also at a heightened risk for obesity and metabolic disorders as they grow. This emphasizes the intergenerational impact of this condition, reminding us that our health choices can affect not just ourselves but also our children.
To navigate these challenges and promote long-term well-being, it’s essential for women who have experienced GDM to embrace a healthy lifestyle after pregnancy. This means prioritizing:
- Regular medical check-ups to monitor blood sugar levels
- Maintaining a balanced diet rich in whole foods
- Engaging in consistent physical activity
Continuous glucose monitoring (CGM) can be a helpful tool in managing maternal weight gain and reducing the risk of fetal macrosomia, ultimately supporting healthier outcomes for both mothers and their children.
A prospective cohort study involving over 10,000 women revealed that while GDM alone does not correlate with increased all-cause or cardiac mortality, it remains vital for women to focus on long-term metabolic management. This finding suggests that although the immediate dangers associated with GDM may not lead to higher mortality rates, the potential for developing type 2 diabetes remains a significant concern. As Yi-Xin Wang, MD, PhD, poignantly notes, 'The findings underscore the significance of considering pregnancy-related glucose intolerance as a critical element in later-life mortality likelihood.'
In summary, understanding the long-term impacts of gestational conditions is essential for women to effectively manage their health post-pregnancy. By prioritizing lifestyle changes and regular health assessments, you can significantly reduce your risk of developing type 2 diabetes and enhance your overall well-being. Remember, you're not alone in this journey; we are here to support you every step of the way.
Conclusion
Gestational diabetes mellitus (GDM) is a pressing health issue that calls for our attention, especially for expectant mothers and healthcare providers. With a prevalence projected to affect 6-9% of pregnancies in the United States, it’s crucial to understand the condition's causes, symptoms, and risk factors for effective management. Key contributors include:
- High sugar consumption
- Obesity
- Age
This highlights the importance of proactive measures like early screening and personalized dietary strategies.
Managing GDM effectively requires a multifaceted approach that combines:
- Dietary modifications
- Regular physical activity
- Diligent monitoring of blood sugar levels
By embracing a balanced diet rich in whole foods, engaging in consistent exercise, and collaborating with healthcare professionals, women can significantly reduce the risks associated with this condition. It’s important to remember that the long-term implications of GDM, including an increased risk of developing type 2 diabetes, underscore the necessity for ongoing health management even after childbirth.
In conclusion, empowering women with knowledge about gestational diabetes is essential for safeguarding both their health and that of their babies. Through education and support, expectant mothers can navigate the complexities of GDM, ensuring healthier pregnancies and better long-term health outcomes. Remember, proactive management and lifestyle interventions can make a significant difference. You are not alone in this journey; informed and engaged individuals are key to overcoming the challenges posed by gestational diabetes. We are here to support you every step of the way.
Frequently Asked Questions
What is gestational glucose intolerance (GDM)?
Gestational glucose intolerance (GDM) is a condition that occurs during pregnancy, typically identified in the second or third trimester, characterized by elevated blood sugar levels due to the body's inability to produce enough insulin to meet the increased demands of pregnancy.
What are the potential complications of GDM?
GDM can lead to significant complications, including excessive fetal growth, preterm birth, and an increased risk of developing type 2 diabetes later in life.
How prevalent is GDM in the United States?
Estimates suggest that around 6-9% of pregnancies in the United States will be impacted by GDM by 2025.
Why is early screening important for GDM?
Early screening is crucial for effective management of GDM and ensuring favorable outcomes for both the mother and child, particularly for women who may be at higher risk, such as those with a family history of blood sugar issues or those who are overweight.
What management strategies are recommended for GDM?
Recommended management strategies include personalized dietary plans, regular physical activity, and continuous glucose monitoring to help regulate blood sugar levels effectively.
How does sugar intake relate to gestational diabetes?
High sugar consumption can cause rapid spikes in blood glucose levels, potentially overwhelming the body's ability to produce insulin. Excessive intake of simple sugars is linked to greater weight gain during pregnancy and a higher likelihood of developing gestational diabetes.
What does research indicate about sugar consumption and GDM risk?
Research, including a study in the Journal of Clinical Endocrinology & Metabolism, indicates that women consuming large quantities of sugary foods face an increased risk of pregnancy-related glucose intolerance, suggesting that managing sugar consumption is crucial for preventing GDM.
What resources are available for managing concerns about sugar intake during pregnancy?
There are various resources and support systems available to help expectant mothers navigate concerns about sugar intake and manage their health effectively during pregnancy.



